* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Nursing Care Plan
Survey
Document related concepts
Transcript
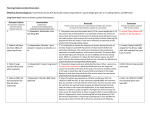
Planning/Implementation/Evaluation Med/Surg Nursing Diagnosis: Decreased cardiac output R/T Slow Heart Rate and insufficient blood supply to the body AEB increased BNP Long-Term Goal: Patient cardiac output will improve Outcome Criteria Interventions One outcome criteria for each intervention. Number each one. Label each as assess/monitor/independent/ dependent/teaching/collaboration 1. Patient will have no peripheral edema by 10/6/2014 1. Independent: Monitor edema q shift 2. Patients heart rate will be 60-100 bpm when assessed 2. Independent: Assess heart rate q 8 hours 3. Patient LOC will not change during each shift 3. Independent: Monitor changes in LOC at all times 4. Patient BNP will trend toward 0-99 by 10/6/2014 4. dependent: Monitor BNP as ordered Rationale Evaluation Answers why, how, what your interventions will help solve, prevent, Or lesson the stated problem specific to each patient. Evaluate the patient outcome, NOT the intervention 1. Decreased cardiac output causes a backup of blood on the right side of the heart which causes the blood to stay in the veins. The outcome is peripheral edema. The patient is 92 years old and has a decrease in her cardiac output. When she was admitted to hospital she had bilateral lower extremity +1 pitting edema. Monitoring peripheral edema will help determine if the cardiac output is improving or getting worst. 2. The patient came into the emergency room with a heart rate of 36 BPM and was experiencing bradycardia. A normal heart rate is 60100 BPM. When the heart rate is this low, there is not enough cardiac output to meet the demands of the body and a decrease in tissue and organ perfusion. Symptoms of bradycardia are hypotension, weakness, angina, dizziness or syncope, SOB, and cool pale skin. She was weak, fatigued, and disorientated when she was admitted. They eventually inserted a pacemaker to help keep her heart rate above 60 BPM. 3. Restlessness, agitation and confusion are early signs of decrease cerebral perfusion. When a patient’s cardiac output is decreased there is not enough oxygenated blood in the brain. Determining a baseline mental status is important for this patient because of the dementia. Monitoring and noting any change in behavior will help determine her cerebral perfusion. 4. B-Type natriuretic peptide (BNP) are hormones that are secreted in the left ventricle of the heart. The level increase when the ventricles are working harder to pump the blood through the body, which is known as left ventricular dysfunction. It also helps determine if dyspnea is related to cardiac problems. The higher the levels increase the more severe the heart failure is. The patient’s BNP levels on 9/26/2014 during admission were 968 then increased to 1034 on 9/27/14, so it showed an increase in left ventricle dysfunction. When a patient’s BNP are above 900 heart failure is diagnosed as severe. Monitoring BNP will help determine if the left 1. Partially met. Her +1 pitting edema went down, but she still had some. 2. Met. Her heart rate was between 60-100 BPM during my shift 3. Met. Her LOC did not change during my shift 4. Not met. BNP where not obtain during my shift 5. Patients Na+ 135145, Mg2+ 1.6-2.6 mg/dl, Ca 9-10.5 mg/dl, and K+ 3.5-5 mg/dl by 10/6/2014 5. Dependent: Monitor electrolytes daily 6. Patients I/O will be with 200 ml by 10/06/2014 6. Independent: Monitor I/O q shift 7. Patient will have no peripheral edema by the end of Lasix therapy 7. Dependent: Administer Lasix 20mg QD 8. Patient will have no liver enlargement or tenderness when assessed. 8. Independent: Assess for hepatomegaly q shift 9. Patient will have a clear chest x-ray by 10/06/2014 9.Dependent: Monitor chest X-ray when completed 10. Patient will perform ADL’s without fatigue each day 10. Independent: Encourage rest and activity periods daily ventricle dysfunction is improving or getting worst. 5. Proper electrolyte balance of Na+, Ca, K+ and Mg are important for cardiac output. A change in electrolyte levels could cause dysrhythmias which could further decrease the patients cardiac output. Upon admission the patient’s electrolyte levels where in normal limits, but they all decreased due to the Lasix treatment. It is important to monitor any changes in levels so you can properly correct them as soon as possible. 6. Monitoring intake and output is an important indicator of fluid balance. If a person is taking in more fluid than they are excreting and their cardiac output is low, it can exacerbate their peripheral and pulmonary edema. The patient cardiac output is low she had Bilateral lower extremities 1+ pitting edema and the chest x-rays showed some pleural effusion in her right lung. 7. Lasix is important therapy for reducing edema and improving cardiac output. By using Lasix there will be an increase in renal excretion of fluids. Research has shown reducing fluids in the vascular system reduces the patients preload by reducing the venous return. Reducing the preload will allow the heart to work more efficiently by improving stroke volume and increasing cardiac output. The patient was in fluid volume overload when she was admitted, causing her to have a decreased cardiac output. Therefore, the Lasix was prescribed. 8. When a person has heart failure and reduction in the venous blood return it can cause blood and fluid to become backed up in the body. The excess blood and fluid cause’s congestion in the liver. This causes the liver to increase in side and become tender. The patient was admitted with peripheral edema but did not have hepatomegaly. By assessing for the development of hepatomegaly you can assess if the heart failure treatment is working and or if cardiac output is decreasing. 9. Chest x-rays are a way to monitor excess fluids in the lungs. When a person has decreased cardiac output, the blood in the lungs gets backed up causing pulmonary edema. When the patient was admitted she already had some fluids in her lungs due to decrease cardiac output. Monitoring chest x-rays will determine a shift in cardiac output. 10. When a person has decreased cardiac output they are receiving a reduction in oxygenated blood in their body. The decrease level of oxygen leaves the person short of breath and fatigued. Having time to rest during activities will allow the energy to perform their ADL. The patient is 92 years old, but still lives alone with the help of a home nurse. It is important that she can accomplish as many of her ADL’s independent as possible for her. 5.Not met: Her Na+ and Ca where low on 10/3/2014 6. Partially met: she still had edema and was on fluid restriction. Her output was greater than her intake. 7. Partially met: Her edema was going down put she still had some peripheral edema 8. Met: She had no signs of hepatomegaly when assessed 9. Not met: there were no new chest x-ray during my shift 10 Met: encouraged rest when she was eating 11. Patient will not have S3 and S4 heart sounds when assessed. 11. Independent: Assess heart sounds for S3 and S4 11. A S3 heart sound occurs right after the S2. You hear it in adults when 12. Patients strength will improve and she will be able to independently perform more of her ADL’s while in STR 13. Patient will verbalize knowledge of medication by 10/6/2014 12. Dependent: Collaborate with Short-term rehab now 14. Patient will trend towards clear when assessed 14. Independent: assess lungs sounds q 8 hrs 15. Patient will not gain more than 1lb daily. 15.Independent: Monitor patient weight q day 16. Patients heart rate will be between 60-100 bpm when assessed 16. Dependent: Administer Atropine 1mg q 6 hrs PRN 12. The patient is 92 years old with dementia and lives alone right now. She has been in the hospital 9/26/14 and needs help in her ADL’s right now. Short term rehab will help the patient recover from her illness and improve her strength so she can perform her ADL’s independently. They can also assess her for the need of skilled nursing home placement. 13. Evidence based medicine has proven heart failure medications reduce morbidly, mortality and improve patient’s quality of life. The patient is 92 years old and has dementia which makes teaching medication compliance even more important. Work with her home nurse and daughter to educate on new or changes in current medications. Give a list of each medication and how and when to take them. 14. When cardiac output is decreased fluids back up in the lungs causing fine crackles at the base of the lungs. Increased crackles is an indication that the heart failure is worsening and cardiac output is decreasing. Currently the patient lungs sounds are negative for crackles. Assessing for the appearances of crackles would indicate cardiac output is decreasing and the heart failure is worsening. 15. When a person gains more than 2 lbs in one day it is an indication of fluid volume excess related to a decrease in cardiac output. Weighing the patient daily will help determine if there is a change in their fluid volume. The patient was admitted with peripheral edema, so to determine if her cardiac output was increasing she should lose any weight she has gained due to the edema. 16. Atropine inhibits the action of acetylcholine at postganglionic sites located the smooth muscle. This blocks the effects of the parasympathetic nervous system and causes an increase in a person’s heart rate. The patient heart rate was a 36 BPM when she came into the emergency room and Atropine was prescribed if they needed it to use to get her heart rate above 60 BPM. 13. Independent: Teach medication compliance now there is fluid volume overload in the ventricle that is usually caused by heart failure. An S4 occurs right before the S1 and is caused by ventricle hypertrophy which could be caused by coronary heart disease. Upon admission the patient had a 3/6 systolic murmur over the aorta which was caused by stenosis of the aorta. There were no S3 or S4 sound detected. Assessing the heart sounds for S3 and S4 will help determine if there is an increase in fluids or hypertrophy. 11. Met: there were no S3 or S4 during when auscultating heart sounds. 12. partially met: working on getting her placed in a short term rehab 13. unmet: patient did not verbalize medication compliance 14. Partially met: patient lung sounds where diminished 15. Met: patient did not gain weight. 16. Met: Patient heart rate was 83 and 62 17. Patient K+ level will be between 3.5-5 mEq/l while taking Lasix. 17. Dependent: Administer Potassium Chloride 30 mEq/l PO TID 17. Potassium Chloride is prescribe to prevent the depletion of potassium due to the Lasix the patient was receiving for her edema. Potassium is an activator in many enzymatic reactions and is essential to transmission of nerve impulses, and the contraction of cardiac, skeletal, and smooth muscle cells. When the potassium level falls below 3.5 mEq/l can develop dysrhythmia. It is important to monitor her potassium daily so you know she is not being depleted due to her Lasix therapy. 17 Met: on 10/3/14 her K+ level was 3.9 mEq/l Psychosocial Need Prioritized Psychosocial Nursing Diagnosis: Risk for anxiety R/T chronic illness Long-Term Goal: Patients will not have an increased level of anxiety Outcome Criteria Interventions One outcome criteria for each intervention. Number each one. Label each as assess/monitor/independent/ dependent/teaching/collaboration 1. Patient HR 60-100, BP 120/80, no diaphoresis and body or facial tension when assessed 1. Independent: assess patients level of anxiety q shift 2. Patient anxiety level will remain low when interacting with her 2. Independent: Maintain a calm manner while interacting with the patient 3. Patient room will be quiet and stimuli free at all times 3. Independent: Maintain a quiet environment at all times. 4. Patient will discuss feelings she experiencing increased feelings of anxiety 4. Independent: practice active listening when interacting with the patient. Rationale Evaluation Answers why, how, what your interventions will help solve, prevent, Or lesson the stated problem specific to each patient. Evaluate the patient outcome, NOT the intervention 1. When a patient’s level of anxiety increases they start to have physical changes. You can see a change in their HR, BP, diaphoresis, and facial and body tension. This happens because of the fight or flight response of the sympathetic nervous system. The patient was recently living at home and now she has to adjust to the hospital environment. This could increase her anxiety level. Assessing an increase in her anxiety level and treating it would help to control her anxiety level. 2. A patient can sense when a nurse is stressed and is experiencing their own anxiety. This can be projected to the patient and increase their own anxiety. The patient experienced fecal incontinence and she verbalized slight anxiety because of it. Keeping a calm manner helped her keep her anxiety to a minimum. 3. Anxiety can increase with excessive noise and stimuli that seems to go hand in hand with hospitalizations. The patient is used to living in a quiet environment, so the increase noise and stimuli in a hospital could increase her anxiety. Keep voices, noises and stimuli to minimum will help keep her anxiety down. 4. A very important part of the nurse- patient therapeutic relationship is active listening. The patient is 92 years old and expressed feelings of boredom and being scared. Stopping what you are doing and just listen to her express her feeling and fears without judgment or opinions will help keep her anxiety level low. 1. Met: Patient’s HR, BP remained between 60-100 and BP 106/70 when assessed 2. Partially met: I tried to keep a calm manner when I was interacting with her, but I’m not sure I succeeded. 3. Partially met: There were a lot of people going in and out of the room. I tried to keep other stimuli to a minimum. 4. Met: I took the time to listen to her when she was expressing her feelings