* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Peripartum cardiomyopathy- a pregnancy related disorder
Survey
Document related concepts
Electrocardiography wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Echocardiography wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac surgery wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Transcript
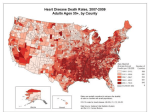
Peripartum cardiomyopathy- a pregnancy related disorder A Review Dr I.Kjaev, Dr S.Jovanova Abstract Peripartum cardiomyopathy is a pregnancy related disorder of unknown origin, it is an Idiopathic heart failure that occurs in the absence of any determinable heart disease in the last month of pregnancy and within 5 months of delivery. Worldwide incidence varies among nations with the highest prevalence in Nigeria 1% and Haiti 0,33%.These numbers are far lower in more industrialized countries like South Africa 0,1% and the USA 1 in 3000-4000 deliveries. Prognostic criteria depend on the normalization of the left ventricular size and function within 6 months of delivery. Up to 50% of patients with Peripartum cardiomyopathy (PPCM) recovers with out complications even though this may not be apparent in the first 6 months. Mortality ranges between 3,3 – 9,6% in well developed countries. The incidence in Macedonia is unknown. A lack of well organized multidisciplinary approach leads to misdiagnosis and late discovery. Key words: cardiomyopathy , pregnancy, ventricular end-systolic dimensions, left ventricular ejection fraction, postpartum period, epidemiology, heart failure, therapy, pregnancy complications, prognosis, consecutive pregnancy 1 Introduction Peripartum or sometimes called postpartum cardiomyopathy ( PPCM) is a serious life Treating diseases that occurs during pregnancy or during the post partum period1.Heart Failure during pregnancy has been discussed and recognized as early as in the 19th Century, however the first steps towards understanding the complex of the issue were done in the late 1930 and with the pioneer work of Demakis et al. His criteria for the diagnosis of PPCM included, development of cardiac failure in the last month of pregnancy or within 5 months after delivery, absence of determinable etiology for the cardiac failure and absence of demonstrable heart disease prior to the last month of pregnancy. The clinical form of peripartal cardiomyopathy is similar to other cardiomyopathies the main difference is the rapid onset of symptoms, previously normal healthy individuals can acquire a condition that could in some circumstances only be managed by heart transplantation. Recent studies have shown that an estimated 80% of symptomatic patients recover, however completed recover is only expected in 30% of the cases with normalization of the left ventricular function and size2. A central element in the establishing the right diagnose is an ejection fraction of less then 45% or the combination of an M-mode fractional shortening of less than 30% and an end-diastolic dimension greater than 2,7sm/m2. Symptoms that are often seen with this condition include dyspnea, cough, orthopnea, hemoptysis, chest and abdominal discomfort. These are symptoms commonly found in normal pregnancy which makes an early diagnose very difficult to make. Most 2 affected patients have New York Heart Association (NYHA) class III or IV function.3 Many differential diagnosis can be found the fulfill the previously stated symptoms, those would include preeclampsia, eclampsia, pulmonary embolus, pneumonia or systemic infection. Diagnosis and postpartum monitoring are helped by, echocardiography, MRI, endometrial biopsy, chest x-ray, electrocardiography and others. Epidemiological findings suggest that black race, multiparty, maternal age >30 years, twin gestation and history of hypertension ,preeclampsia or eclampsia are associated with higher incidence of peripartum cardiomyopathy4,5.The incidence of PPCM is quoted as 1 in 3000-4000 deliveries for the USA and Europe,1-1000 deliveries in South Africa and 1-300 in Haiti2 Materials and Methods Information was gathered through Pub med Central. Key words used were peripartum cardiomyopathy and postpartum cardiomyopathy. Most of the selected literature represent small study groups and most of the information a not sufficient enough to establish a good overview. Discussion The over goal of this research is to establish a clear algorithm of early discovery and treatment. Multidisciplinary treatment which would include a gynecologist, anestihiologyst and a cardiologist would certainly help. The reality is that the delay between the first symptoms and the diagnosis can range from a few weeks to several months in as much as 30% of all cases.6 3 The right way to start understanding peripartum cardiomyopathy is to find the causes, although it seems to be an idiopathic disease several theories exist. - Inflammation High concentrations of tumor necrosis factor –α(TNFα),intertferon- γ,interleukin -6,CRP and Fas/aptosis antigen 1(Apo-1) in PPCM7 suggest an underlying inflammatory process for the pathophisiological development of PPCM. - Myocarditis Most of the patients that suffer from peripartal cardiomyopathy have been found to have myocardial inflammation reports range from 29% - 100%3.It is still unclear whether an actual infection is a trigger to this condition because most of the studies were done at different times from the episode of cardiomyopathy. Future research is needed for a clear answer. - Fetal Chimerism Fetal cells escaping in to the maternal circulation during pregnancy are usually destroyed by the mothers immune system. In rare circumstances a weakened immune system during pregnancy would allow these cells to settle in the maternal heart and so triggering a response when the immune system has normalized 8.This casual relationship is still yet to be confirmed - Genetics associations Several family mutations such as MYH7,SCN5A and PSEN2 and sporadic mutations in MYH6 and TNNT2 DCM were found in patients with peripartum cardiomyoptahy. However if these findings are true they would pave a way to genetic screening test for PPCM. Clinical symptoms Most of the early symptoms such as dyspnea, orthopnea, dizziness , pedal edema occur in normal pregnancies. That’s why it’s difficult to diagnose PPCM. Dyspnea in normal pregnancy is thought to be due to hyperventilation caused by the effects of 4 progesterone and also due to the pressure of the growing uterus9 .Peripheral edema is also common among pregnant patients. Among a lot of other symptoms that might be involved it is worth mentioning thromboembolism, cardiac arrhythmias, preexisting hypertension and preeclampsia . Preeclampsia is commonly seen in pregnancy, symptoms like high blood pressure, protein in the urine,swelling,sudden weight gain, headaches and blurred vision that occur after the 20th week of gestation. Some reports exist about a latent form of cardiomyopathy with out significant signs and symptoms10 . Doctors should consider peripartum cardiomyoptahy in any patient with unexplained symptoms, delayed diagnosis may be associated with higher rates of illness and death. The aim should be focused on excluding other causes of cardiomyopathy and to confirm left systolic dysfunction by echocardiography. The diagnosis and postpartum monitoring are facilitated by echocardiography, ECG, MRI, endometrial biopsy and laboratory test. Echocardiography is the single most effective test in establishing a diagnosis. Common findings include globally decreased contractility and LV enlargement without hyperttophy11 Follow up studies have shown that patients with higher LVEF at presentation portends better cure rates and shorter recovery time.12It is also true that those patients with high initial LVEF are less likely to have a relapse during a subsequent pregnancy.13Echocardiography as a non invasive test can help diagnose all symptomatic patients with undiagnosed PPCM and so treatment can start sooner. Follow up echocardiography is usually done before discharge from the 5 hospital , at 6 weeks and 6 months postpartum and annually therafeter.14 MRI – enables the precise diagnosis of myocarditis,necrosis and LV thrombi and can acquire accurate measurements of ventricular volumes, however it’s and expensive technique that is not as effective as echocardiography. ECG commonly seen changes are left ventricular hypertrophy and ST-T wave abnormalities.14 Less common signs include atrial fibrillation ,flutter, prolonged PR and QRS intervals. Chest Radiography When evaluating new onset of dyspnea,tachycardia or hypoxia, obtain a chest radiograph to detect pulmonary edema. This should be preformed with abdominal shielding to evaluate the etiology of hypoxia and exclude pneumonia. Fetal radiation exposure with 2 maternal chest radiographs with abdominal shielding is about 0,00007 rads. The accepted limit of fetal radiation exposure is 5 rads. Endometrial biopsy is highly specific technique for diagnosing myocarditis, however because it is an invasive procedure it is not the first line diagnostic tool. Endometrial biopsy might be considered when myocarditis is suspected or when no improvement is seen 2 weeks after heart failure therapy.3 Cardiac protein assays They are not a standard diagnostic tool , however a recent prospective trail of 106 patients with high troponin T levels ( > 0,4ng/ml) witin 2 weeks of peripartum cardiomyopathy onset significantly predicted smaller LVEF and persistent LV dysfunction at 6 months follow up ( P< 0,001)15 Therapy 6 Much research has been done in trying to find the right treatment. It is specific because the setting is in the peripartum period were some drugs are not recommended. A well balanced and multidisciplinary approach is needed that would involve cardiovascular medicine,obstetrics,immunology,pathology and others. The goal of the therapies is similar like a other condition of cardiomyopathy , that is through pharmacological therapy to resolve the issue . It is also worth mentioning that patient education is essential,every treatment option should be first discussed with the patient so that she can feel that she is actively involved with therapy. One must remember that a healthy fetus depends on a healthy mother. Medications should only be used when the benefit to the mother is clear. Some of the medications used have clear teratogenicity so careful use is warranted. Diuretics – reduce preload and treat pulmonary congestion or peripheral edema, both hydrochlorthiazide and furosemide are safe during pregnancy and lactation. The known side effects include uterine hypoperfusion and maternal metabolic acidosis16 , as with any medication caution is needed. ACE inhibitors –are considered first line therapies for heart failure therapy but they are known to be contraindicated in pregnancy17. They can be used when the pregnancy has ended but breast feeding should also be stopped. Vasodilatators – Hydralazine is safe during pregnancy and is the primary vasodilatotor drug antepartum11, in more severe case the use of nitroglycerin is warranted. 7 Digoxin – an inotropic and dromotropic agent is safe to use antepartum,because of few available options during that period digoxin is an easy choice18 Inotropic agents – the use of dobutamin and dopamine is warranted only in cases of severe low output, as soon as a patient is stable (hemodinamicaly) different treatment option should be used.14 Beta- blockers – these drugs can be a second line of therapy during pregnancy when clinically indicated. All are compatible with breast feeding Calcium Channel blockers – are found to reduce the interlukin -6 levels in heart failure patients19,some caution is needed due to uterine hypoperfusion. Arrhythmia management – atrial fibrillation is the most common arrhythmia in patients with peripartum cardiomyopathy.20 Quinidine and proacinamide are relatively safe to use in puerperium and can therefore can be considered as a first line therapy 21, digoxin can also be used. Anticoagulants – Peripartum cardiomyopathy is associated with high rate of tromboembolic complications, heart faiulure and pregnancy21 are both independent risk factors. Cases of arterial or venous thrombosis have been reported in as much as 50% of women with PPCM. Because pregnancy is a hypercoagulable state once the diagnosis of PPCM has been made prophylactic anticoagulant therapy should be given during pregnancy. Full dose anticoagulation should be initiated ante partum for women with deep venous thrombosis,atrial fibrillation, ventricular thrombi , embolic events or when the ejection fraction is less then 30%.Treatment should be continued 8 at least 6 weeks postpartum. Other agents – Several studies are currently being done to find new drugs or treatment options for PPCM, those include immunosuppressive drugs, intravenous immunoglobulin, pentoxifylline( antiplatelet) and bromcriptine. Mechanical Circulatory Support and Transplantation In some severe cases mechanical circulatory support or even transplantation may be needed. Both intra-aortic balloon pumps and LV assist devices ( LVADs) have been used to bridge transplantation.22 .In recent years bridging the recovery via prolonged circulatory support has helped to dramatically decrease the percentage of PPCM requiring transplantation from 33% to 4%-7%14 .The potential for organ rejection in peripartum cardiomyopathy is high due to the increased prevalence of autoimmune mechanisms. Route of delivery Vaginal deliveries are preferred because they are associated with much lower rates of complications, such as endometritis and embolism. Cesarean section is responsible for 75% of incidents with embolism. Vaginal deliveries are not associated with the post operative third spacing of fluid that occurs after cesarean deliveries. Unless the mother is decompensating, managing her medically and waiting for a spontaneous vaginal delivery is reasonable. However if she is not responding to medical therapy or if the fetus must be delivered for obstetrics reasons, the best plan is to induce the labor with the goal of vaginal delivery. Effective control of maternal pain during delivery is 9 paramount. Regional anesthesia such as epidural or spinal is not associated with myocardial depression as observed with inhaled anesthetics. The patient should not be allowed to push, the uterus can expel the fetus without maternal pushing. The use of low-forceps or vacuum can be used in the final stages of delivery. Prognosis Recovery from PPCM is defined as a recovery of LVEF to >0,50 or improvement by >20.Recovery usually occurs between 3 and 6 months post partum, but in some rare circumstances as late as 48 months postpartum23.The estimated mortality rate associated with PPCM in the US is 6%-10%24.Death usually occurs within 30 days. Even after a complete recovery from peripartum cardiomyopathy, the risk of recurrence in subsequent pregnancy remains high and LVEF once improved can worsen again. At this moment in time subsequent pregnancy is not advised for a patient that had an episode of PPCM. Conclusion Periaprtum cardiomyopathy is a potentially life-treating illness which usually arises shortly after delivery. Early diagnosis is prognostic ally important in these young women. Hence the possibility of PPCM should be kept in mind by the doctor as a possible complication of the postpartum period, wherever there are symptoms of heart failure. Management of peripartum cardiomyopathy should first aim at improving heart-failure symptoms through conventional therapies and then administering target therapies. Luckily despite a high risk of recurrence in subsequent pregnancies many patients with peripartum cardiomyopathy recover within 3 to 6 months. 10 1 1. Demakis J, Rahimtoola S, Sutton G, Meadows R, Szanto P, Tobin J, et al. Natural course of peripartum cardiomyopathy. Circulation 1971;44:1053-61. [PubMed] 2 Sliwa K,Fett J, Elkayam U ; Peripartum cardiomyopathy.Lancet 2006; 368:687-93 3 Bhakta P, Biswas BK, Banerjee B. Peripartum cardiomyopathy: review of the literature. Yonsei Med J 2007;48(5):731–47. [PMC free article] [PubMed] 4 Gentry MB, Dias JK, Luis A, Patel R, Thornton J, Reed GL. African-American women have a higher risk for developing peripartum cardiomyopathy. J Am Coll Cardiol 2010;55(7): 654–9. [PubMed] 5 Homans DC. Peripartum cardiomyopathy. N Engl J Med 1985;312(22):1432–7. [PubMed] Denise Hilfiker-Kliener,Elisabeth Schieffer,Gerd Peter Mayer,Edith Podewski,Helmut Drexler – Deutssches Artzteblatt International 2008; 105(44):751-6 6 7 Sliwa K, Forster O, Libhaber E, Fett JD, Sundstrom JB, Hilfiker-Kleiner D, Ansari AA. Peripartum cardiomyopathy: inflammatory markers as predictors of outcome in 100 prospectively studied patients. Eur Heart J 2006;27 (4):441–6. [PubMed] 8 Lapaire O, Hosli I, Zanetti-Daellenbach R, Huang D, Jaeggi C, Gatfield-Mergenthaler S, et al. Impact of fetal-maternal microchimerism on women's health–a review. J Matern Fetal Neonatal Med 2007;20(1):1–5. [PubMed] 9 Simon PM,Schwartzstein RM,Weiss JW,Fenci V,Teghtsoonian M,Weinberger SE Distinguishable typer of dyspnea in patients with shortness of breath.Am Rev Respir Dis 1990;142:1009-1014 10 Fett JD,Christie LG,Carraway RD,Ansari AA,Sundstorm JB,Murphy JG Unrecognized peripartum cardiomyopathy in Haitian women. Int J Gynecol Obstet 2005; 90:161-166 11 Lampert MB, Lang RM. Peripartum cardiomyopathy. Am Heart J 1995;130(4):860–70. [PubMed] 12 Fett JD, Sannon H, Thelisma E, Sprunger T, Suresh V. Recovery from severe heart failure following peripartum cardiomyopathy. Int J Gynaecol Obstet 2009;104(2):125–7. [PubMed] 13 Fett JD, Fristoe KL, Welsh SN. Risk of heart failure relapse in subsequent pregnancy among peripartum cardiomyopathy mothers. Int J Gynaecol Obstet 2010;109(1):34–6. [PubMed] 14 Sliwa K, Hilfiker-Kleiner D, Petrie MC, Mebazaa A, Pieske B, Buchmann E, et al. Current state of knowledge on aetiology, diagnosis, management, and therapy of peripartum cardiomyopathy: a position statement from the Heart Failure Association of the European Society of Cardiology Working Group on peripartum cardiomyopathy. Eur J Heart Fail 2010;12(8): 767–78. [PubMed] 11 14 Demakis JG, Rahimtoola SH, Sutton GC, Meadows WR, Szanto PB, Tobin JR, Gunnar RM. Natural course of peripartum cardiomyopathy. Circulation 1971;44(6):1053–61. [PubMed] 15 Hu CL, Li YB, Zou YG, Zhang JM, Chen JB, Liu J, et al. Troponin T measurement can predict persistent left ventricular dysfunction in peripartum cardiomyopathy. Heart 2007; 93(4):488–90. [PMC free article] [PubMed] 16 Lindheimer MD, Katz AI. Sodium and diuretics in pregnancy. N Engl J Med 1973;288(17):891–4. [PubMed] 6 17 Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: developed in collaboration with the International Society for Heart and Lung Transplantation [published erratum appears in Circulation 2010;121(12):e258]. Circulation 2009;119(14):e391–479. [PubMed] 18 Widerhorn J, Rubin JN, Frishman WH, Elkayam U. Cardiovascular drugs in pregnancy. Cardiol Clin 1987;5(4):651–74. [PubMed] 19 Packer M, O'Connor CM, Ghali JK, Pressler ML, Carson PE, Belkin RN, et al. Effect of amlodipine on morbidity and mortality in severe chronic heart failure. Prospective Randomized Amlodipine Survival Evaluation Study Group. N Engl J Med 1996;335(15):1107–14. [PubMed] 20 Isezuo SA, Abubakar SA. Epidemiologic profile of peripartum cardiomyopathy in a tertiary care hospital. Ethn Dis 2007;17 (2):228–33. [PubMed] 21 Ferrero S, Colombo BM, Ragni N. Maternal arrhythmias during pregnancy. Arch Gynecol Obstet 2004;269(4):244–53. [PubMed] 21 Refuerzo JS, Hechtman JL, Redman ME, Whitty JE. Venous thromboembolism during pregnancy. Clinical suspicion warrants evaluation. J Reprod Med 2003;48(10):767–70. [PubMed] 22 Gevaert S, Van Belleghem Y, Bouchez S, Herck I, De Somer F, De Block Y, et al. Acute and critically ill peripartum cardiomyopathy and ‘bridge tO’ therapeutic options: a single center experience with intra-aortic balloon pump, extra corporeal membrane oxygenation and continuous-flow left ventricular assist devices. Crit Care 23 Fett JD, Sannon H, Thelisma E, Sprunger T, Suresh V. Recovery from severe heart failure following peripartum cardiomyopathy. Int J Gynaecol Obstet 2009;104(2):125–7. [PubMed] 24 Felker GM, Jaeger CJ, Klodas E, Thiemann DR, Hare JM, Hruban RH, et al. Myocarditis and long-term survival in peripartum cardiomyopathy. Am Heart J 2000;140(5):785–91. [PubMed] 12 13