* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Learning Session 1 Presentation Slides
Remote ischemic conditioning wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
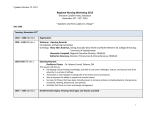
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Shared System of Care COPD/Heart Failure Learning Session 1 www.pspbc.ca Please complete your Evaluation Survey before we begin 2 Faculty/Presenter Disclosures Faculty: [Speaker’s name] Relationships with commercial interests: Grants/Research Support: PharmaCorp ABC Speakers Bureau/Honoraria: XYZ Biopharmaceuticals Ltd. Consulting Fees: MedX Group Inc. Other: Employee of XXY Hospital Group 3 Disclosure of Commercial Support This program has received financial support from [organization name] in the form of [describe support here – e.g. an educational grant]. This program has received in-kind support from [organization name] in the form of [describe support here – e.g. logistical support]. Potential for conflict(s) of interest: [Speaker/Faculty name] has received [payment/funding, etc.] from [organization supporting this program AND/OR organization whose product(s) are being discussed in this program]. [Supporting organization name] [developed/licenses/distributes/benefits from the sale of, etc.] a product that will be discussed in this program: [insert generic and brand name here]. 4 Mitigating Potential Bias [Explain how potential sources of bias identified in slides 1 and 2 have been mitigated]. Refer to “Quick Tips” document 5 Housekeeping www.gpscbc.ca/psp-learning/adult-mental-health/tools-resources 6 Agenda 7 Welcome and Introductions (15) Video Clip or Patient Story (15) COPD 101 (70) Local respiratory services COPD-6 training QuitNow Integrate into Practice Workflow Break (15) Heart Failure 101 (65) Local HF clinic services and cardiologist referral Integration of HF into practice workflow Action Planning Expectations (5) Planning for action Period (25) 7 CME Accreditation Choice of: 10.5 Mainpro Plus credits IF post reflective activity submitted 2-3 months after module completion and at least one action period completed 10.5 Maincert Section 1 8 Module Structure 9 How is a collaborative different than CME? Action-oriented: try what you learn – “What are you going to do next Tuesday?” Test change on small population Track data to evaluate changes When satisfied spread to the larger population Discussion with colleagues 11 AIM To create a system of care that improves the quality of care and experience for patients at risk for and living with COPD and/or HF 12 How will we achieve this aim? Identifying patients earlier who have COPD and/or HF using a case-finding approach Developing relationships and care plans amongst family physicians, specialists, patients, and community services Implementing more standardized referral and consult letters, and improving relationships, hand offs, and communication between GPs and specialists Improving the management of COPD and HF by applying evidenced based practices Supporting patients to quit smoking Enhancing patient self-management skills for patients to manage their condition 13 Action Period 1 Measurement Develop patient registries for COPD and HF. Case-finding and testing with COPD-6 device Referred for Spirometric Diagnostic testing for COPD patients Referred for Ejection Fraction or Brain Natriuretic Peptide (BNP) Diagnostic testing for Heart Failure patients 14 14 Patient Story (15 minutes) Our Aims To foster a shared system of care that improves the quality of care and experience for patients at risk for and living with COPD and Heart Failure by: › Identifying subjects with COPD and Heart Failure earlier › Using a team-based approach › Improving communications between patients and care team as well as within the care team › Developing strategies to prevent progression of COPD or Heart Failure as well as its optimal Improving management 16 How will we achieve this aim? In the FP practice: Enhanced identification and diagnosis of COPD & HF Appropriate risk stratification based on level of airflow obstruction or cardiac output, and symptoms and exacerbation history – followed by review of prescriptions and including a flare-up plan Appropriate use of evidence-based therapies for COPD & HF based on current best evidence, including the development of a flare-up plan 17 How will we achieve this aim? Across the continuum Supporting subjects to quit smoking. Enhancing patient self-management skills to allow better management of their lung health. Improving the patient experience within the system of care. 18 Approach to Dyspnea: COPD/HF Similar clinical presentation Both may be present in the same person Diagnostic confirmation of disease needed What condition is contributing to the dyspnea? 19 COPD/Heart Failure 25-30% HF patients have COPD 20-40% COPD patients have HF “Common partners, common problems” Presence of each other predicts increased mortality 20 Look for clues! 1. Initial clinical judgement 2. Risk factors for heart increase likelihood of HF 3. Symptoms of PND, orthopnea or edema increase likelihood of HF 4. Signs for HF include: › 3rd heart sound, arrythmia or murmur › ↑ JVP › Crackles › Edema 5. Signs for COPD or AECOPD › Air-trapping, wheezing, quiet lungs, prolonged expiration › Worsened cough with increased or purulent phlegm 21 A Case of Dyspnea Postbronchodilator FEV1/FVC 48% FEV1 55% Echo 2 years prior showed EF 45% Shortness of breath has worsened in past week WHY? 22 Approach to Dyspnea: Diff Dx Respiratory • Airway disorders •COPD/AECOPD •Asthma • Parenchymal • Cancer • ILD • Pneumonia • Pleural or chest wall disorders • Vascular • Central Cardiac • CHF • Arrhythmia • Ischemia • Valvular • Pericardial Systemic • Anemia • Acidosis (numerous causes eg renal) • Liver disease • Thyroid • Pregnancy • Anxiety Schwartzstein RM. UpToDate: January 2014. 23 Approach to Dyspnea Onset of symptom › Gradual vs sudden, rest or exertion? Think: CARDIAC, RESP, SYSTEMIC 24 Approach to Dyspnea Associated symptoms › Cough, sputum, wheeze › Chest pain: pleuritic versus exertional › Palpitations, dizziness Think: › Edema, orthopnea, PND CARDIAC, RESP, › Bleeding causing anemia SYSTEMIC 25 Approach to Dyspnea Associated signs › Pallor Think: › Tachycardia or arrhythmia CARDIAC, › Crackles vs wheeze RESP, › Hyperinflation vs chest restrictionSYSTEMIC › Edema › ↑JVP, S3, murmur 26 Examination in 2 minutes General appearance Heart Rate Rhythm BP (O2 sat) Listen to chest Listen to heart JVP assessment Edema 27 Diagnostic Tests O2 sat: rest and on exertion EKG CXR Hb, BNP, LYTES with anion gap, TSH, troponin, renal, liver, PFTS ECHO Other tests: › PE Protocol CT › High resolution CT › Stress test or MIBI, MUGA › ABG 28 Case continued Current inhalers include an lone ICS inhaler and short › Has not followed up with you recently › Renews her prescriptions intermittently Other Rx: rosuvastatin, HCTZ, amlodipine, metformin, daily ASA Exam reveals decreased breath sounds bilaterally, wheeze, Heart rate of 90, JVP of 4 cm, pitting edema to shins and BMI 36 How would you proceed with this case? ICS (inhaled corticosteroid), LABA (long-acting ß-agonist), LAMA (longacting muscarinic antagonists), JVP (jugular venous pressure), HCTZ (hydrochlorothiazide) 29 What tests could be ordered from your office to sort this patient out? Respiratory • CXR • CT scan • Repeat spirometry Cardiac • ECG • CXR • BNP • ECHO • Stress test Systemic • CBC • Electrolytes, • Urea, Cr You may start by sending this patient to lab for an ECG, CXR and Blood work Schwartzstein RM. UpToDate: January 2014. 30 Diagnostic tests have limitations: Spirometry best done when patient stable › HF can reduce FEV and FVC Echo is technically difficult if Afib or COPD › Reduced EF does not necessarily mean that decompensation is acute HF BNP has good negative and good positive predictive values › <100 = not acute HF › >200 = possible HF › >500 = definite HF 31 β-blocker therapy is safe in COPD¹ ² ³ Selective β1-blockers Metoprolol Atenolol Bisoprolol Non-selective α (alpha) and β-blockers used in CHF that are found to be safe in COPD Carvedilol These agents should not be withheld from patients with COPD and cardiac disease 1. Camsari A, Heart Vessels 2003;18:188–192. 2. Salpeter SRAnn Intern Med 2002;137:715–725. Salpeter SR, Respir Med 2003;97:1094–1101. 3. GOLD guidelines 2013 32 COPD 101 (25 minutes) Definition of COPD COPD is a preventable and treatable disease with some significant systemic effects that may contribute to the severity in individual patients. Its pulmonary component is characterized by airflow limitation that is not fully reversible. This leading to significant exercise limitation. The airflow limitation is usually slowly progressive over time. This is accelerated in cases of continued smoking, frequent ‘lung attacks’ or with AAT deficiency. 34 Asthma 35 Clinical Course of COPD 36 Prevalence and Burden of COPD Global Disease Burden 1990 : COPD was 6th leading cause of death 2001: Approx. 2.7 million deaths from COPD (more than 5% of total death worldwide) 2020: COPD is projected to be the 3rd leading cause of death (approx 4.5 million deaths) only after Ischemic Heart Disease and Cerebrovascular Disease Murray and Lopez. Lancet 1997 WHO Report 2002 38 COPD is Under-diagnosed in Canada Patients >40 yrs + 20 pack-year history of smoking visiting a primary care physician for any reason 1,003 patients underwent spirometry: Diagnosis of COPD Spirometry results Normal 79.3% Criteria for COPD 20.7% No 67.3% Yes 32.7% Hill K, et al. CMAJ 2010182:673-678 39 Hill K, et al. CMAJ 2010, 182;673-678 39 Case Finding 40 40 Diagnosis 41 41 Key Message “Most patients with COPD are not diagnosed until the disease is well advanced. Spirometry targeted at individuals who are at risk for COPD can establish an early diagnosis.” Can Respir J 2008;1 5 (Suppl A):1A-8A 42 Fletcher Curve - the Effect of Smoking on FEV1 43 Local respiratory services COPD-6 training The COPD6 If you have a normal result has the potential to rule out COPD May have some false positives due to 6 second exhalation time reducing the denominator ie FEV1/FEV6. 47 47 If FEV1/FEV6 is low ,<0.7 ,then refer to accredited lab for definitive diagnosis Walk in spirometry clinics 48 48 COPD-6 Accurate enough for FEV6 & Ratios (And multi-patient use. Exceeds ATS/ERS guidelines) Simple to use – just turn unit on (enter Age, Height; Sex and blow for 6 seconds Press Enter to view best) Detach flow head for cleaning Includes predicted value sets Built-in quality of blow indicator Large easy to read display Displays FEV1 and % predicted Displays FEV6 and % predicted Displays FEV1/FEV6 and % predicted Lung Age indicator Obstructive Index and displays degree of obstruction Provides GOLD COPD classification (Class I; II; III; IV) AAA Batteries 49 49 COPD-6 (continued) Built-in quality of blow indicator Slow Start Warning: Vext >5% or 150mL of FEV6 Abrupt End: Change of volume is > 25mL in the last sec No coughing: 50% drop & recovery in flow in the 1st sec If Blow <1 sec FEV1 = 0.00 Result out of Range FEV6 (0-8L) Obstructive Index (Measured FEV1/Pred FEV1) & COPD Stage I - IV (with ratio FEV1/FEV6 > 70%) AAA batteries Turns off after 4 minutes Low battery indicator Green ≥ 80% + ratio > 0.70 Green ≥ 80% Yellow = 50 - 80% Orange = 30 - 49% Red < 30% = Not COPD = STAGE I = STAGE II = STAGE III = STAGE IV All boundaries can be reset 50 50 COPD-6 (continued) 1. Turn on (Age Symbol and 50 appears on screen) 2. Scroll up/down To adjust age (if the buttons are kept depressed, the values will scroll faster) 3. Press Enter (Height Symbol and 60 appears on screen) 4. Scroll up/down To adjust height in inches 5. Press Enter (Male Symbol appears on screen) 6. Scroll up/down For Female symbol 7. Press Enter (Population Group Symbol appears on screen) 51 51 Entering subject data continued 8. Scroll up/down to select: C - Caucasian AA - African-American HA - Mexican-American Note: use C for all other races 9. Press Enter 52 52 Copd-6 is now ready for blow • Place the Mouthpiece into the Copd-6 • Hold your head up, breathe in as deeply as possible, place the mouthpiece in your mouth, biting it lightly while sealing your lips firmly around it. • Blow out as HARD and FAST as you can for a full 6 seconds. • Repeat 2 more times when the blow icon appears. • Hold down the enter key to bring up the last session results 53 53 Results of blow Blow is classified as Green, Yellow, or Red Obstructive Index (Measured FEV1/Pred FEV1) & COPD Stage I - IV (with ratio FEV1/FEV6 > 70%) Green ≥ 80% + ratio > 0.70 Green ≥ 80% Yellow = 50 - 80% Orange = 30 - 49% Red < 30% = Not COPD = STAGE I = STAGE II = STAGE III = STAGE IV 54 54 Indication of bad blow The blow icon with an exclamation point indicates a bad blow. Possible reasons are coughing, slow start, blow less than 3 seconds in duration, abrupt stop, or blocking the back of copd-6 unit with hand. 55 55 Test results after three blows Press Enter to display the best of the session Press enter to display the best FEV1 and percent predicted of all blows Press the down arrow to see Lung Age Press the down arrow again to see FEV1/FEV6 Ratio & percent predicted Press the down arrow again to see FEV6 & percent predicted 56 56 The Copd-6 USB version’s printed report 57 57 Training http://www.youtube.com/watch?v=syXXEgZSTOQ 58 58 1 (877) 455-2233 Progress in British Columbia Progress in BC 61 Intention to Quit Intention to Quit 62 Physicians discussing quitting Physicians Discussing Quitting 63 Effect of Physician intervention Effect of Intervention 64 What can Physicians do? What can Physicians do? 65 Strategies to help your patients quit Complete Personal Risk Assessment for Rx for Health Brief advice to quit smoking Refer to behavioural support (like QuitNow) Recommend patients call 8-1-1 for NRT Order Buproprion or Varenicline (prescription) Strategies 66 What is QuitNow? Behavioural quit smoking support Provincially Funded Managed by the BC Lung Association Evidence-based Free, confidential, 24/7 What is QuitNow? 67 Fax Referral Forms 68 [email protected] Online Referral online 69 Integrate into the workflow discussion End 71 Heart Failure 101 (40 minutes) Definitions and Nomenclature Heart Failure A clinical diagnosis Inability for the heart to deliver sufficient blood/oxygen to meet the demands of the peripheral tissues, or to do so at abnormally high filling pressures, or both Characterized by signs and symptoms of decreased cardiac output and/or volume overload Does not suggest a cause or underlying pathological state Cardiomyopathy Disease of the heart muscle due to any number of causes Clinically characterized by heart failure 73 Definitions and Nomenclature Heart Failure with Decreased Ejection Fraction Poor systolic performance of the heart resulting in decreased cardiac output and increased venous pressures Typically occurs in association with impaired left ventricular systolic function due to any number of causes Left ventricular ejection fraction (LVEF) of <40% Heart Failure with Preserved Ejection Fraction (HF-PEF) Poor diastolic performance of the heart resulting in decreased cardiac output and increased venous pressures May occur in association with preserved (LVEF >40%) or decreased LVEF Systolic and Diastolic heart failure frequently co-exist 74 Prevalence of Heart Failure 12 10 Patients in Millions 10.0 Incidence: 550,000 new cases/yr 8 Prevalence: 6 2% in 40 – 60 year olds 4.8 4 10% in those aged 70+ 3.5 2 0 1991 2001 2037 Year adapted from McMurray and Pfeffer, 2003 75 HF Readmissions Hospital readmission rates are high, and mainly due to recurrent heart failure Lee DS et al. Can J Cardiol 2004;20(6):599-607. 76 Survival After Admission to Hospital for Heart Failure in BC Percentage Alive 100 80 50% survival at 30 months 60 40 20 0 0 5 10 15 http://www.healthservices.gov.bc.ca 20 25 30 35 40 45 50 Months 77 NYHA Classification of Heart Failure Classes Description 1 Year Survival Rate Grade I Early failure no symptoms with regular exercise or restrictions Grade II Ordinary activity results in mild symptoms, but comfortable at rest Grade III Advanced failure, comfortable only at rest; increased physical restrictions Grade IV Severe failure; patient has symptoms at rest > 95% 80 - 90% 55 - 65% 5 - 15% 78 Important Causes of Cardiomyopathy and Heart Failure SYSTOLIC DIASTOLIC Myocardial Infarction Myocardial Infarction Mitral and Aortic Regurgitation Aortic Stenosis Alcohol Hypertension Thyroid Disease Infiltrative Disorders Chemotherapy Radiation Therapy Familial/Genetic Cardiomyopathies Hypertrophic Cardiomyopathy Nutritional Deficiencies Amyloidosis Systolic and Diastolic Dysfunction Frequently Co-Exist 79 What tests could be ordered from your office to sort the patient out? Respiratory • CXR • CT scan • Repeat spirometry Cardiac • ECG • CXR • BNP • ECHO • Stress test Systemic • CBC • Electrolytes, • Urea, Cr You may start by sending this patient to lab for an ECG, CXR and Blood work Schwartzstein RM. UpToDate: January 2014. 80 Diagnostic tests have limitations: Spirometry best done when patient stable › HF can reduce FEV and FVC Echo is technically difficult if Afib or COPD › Reduced EF does not necessarily mean that decompensation is acute HF BNP has good negative and good positive predictive values › <100 = not acute HF › >200 = possible HF › >500 = definite HF 81 BNP – B-type Natriuretic peptide or NT-proBNP – N-terminal prohormone of BNP • Biochemical test of choice for ruling-in or ruling-out the diagnosis of HF and should be considered as part of the initial evaluation of patients with dyspnea suspected of having HF. [Amended, 2015] • BNP (or NT-proBNP) testing should not be used routinely for monitoring disease severity. [New, 2015] 82 82 Local HF Clinic Services 83 Referral Resources Indications for Referral to a HFC Heart Function Clinic Referral Form 84 When and Who Should I refer to an HF Clinic? New onset heart failure NYD Recurrent hospitalizations Difficult to manage using standard therapies Young age Advanced functional symptoms Consideration for aggressive therapies ICD or CRT Coronary angiography Surgery Consideration for cardiac transplant 85 BC’s Heart Failure Website www.bcheartfailure.ca 86 Local Heart Failure services Integrate into the workflow discussion Action Period Planning (20 minutes) Action Period 1 Measurement Develop patient registries for COPD and HF. Case-finding and testing with COPD-6 device – Minimum 6 pts. Referred for Ejection Fraction or Brain Natriuretic Peptide (BNP) Diagnostic testing - Minimum 2 patients. 90 90 Questions