* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Ch.4 Powerpoint - St. Clair Schools
Embryonic stem cell wikipedia , lookup
Cell culture wikipedia , lookup
Hematopoietic stem cell wikipedia , lookup
Chimera (genetics) wikipedia , lookup
Neuronal lineage marker wikipedia , lookup
Adoptive cell transfer wikipedia , lookup
Nerve guidance conduit wikipedia , lookup
Human embryogenesis wikipedia , lookup
Cell theory wikipedia , lookup
Organ-on-a-chip wikipedia , lookup
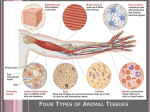
CHAPTER 4 THE TISSUE LEVEL OF ORGANIZATION Pictures from Essentials of Anatomy & Physiology, Third Edition Four Primary Types of Tissue - overview 1. Epithelium • Tightly packed cells form a barrier between external environment on outside & inside. (lumens respiratory & digestive tracts) • Forms endocrine & exocrine glands • Forms nails & hair 2. Connective • Loosely packed • Space between cells occupied by fluid & protein fibers secreted from cells • Collagen is produced in large amts by many (not all) connective cell types. 3. Muscle • Often assoc w/ connective tissue • Cells shorten (contract) in response to voluntary & involuntary nerve activation • Contractions: reduce distance between 2 bones, the circumference of a lumen (capillaries), or the volume of a chamber (heart). • Classification based on the type of innervation (dist of nerves – voluntary or involuntary) and the visibility by light microscope of microfilaments (striated or unstriated). • 3 types: smooth, skeletal, cardiac 4. Nervous • Send & receives info as electrical potentials • Specific nerve cells can release hormones and/or act as a biological clock • Cells of muscle & nervous tissue can alter their membrane electrical potential in response to an electrical, chemical and hormonal stimuli Epithelial Tissue - characteristics • Cover an exposed surface • Cells are bound closely together • Always have a “free” surface exposed to the environment or some internal chamber or passage • Always attached to the connective tissue below via basement membrane • No blood vessels – “avascular” • Line internal and outside body cavities Epithelial 4 Functions 1. Protect exposed & internal surfaces from abrasion, dehydration and damage from chem or biological agents - skin 2. Controls what leaves or enters body – permeable or relatively impermeable 3. Specialized cells can detect changes in the environment & relay this info to the nervous system - skin 4. Produce specialized secretions: glandular epith – Exocrine secretions: released onto body surfaces. Enzymes entering dig tract, sweat, milk – Endocrine secretions: aka hormones, released into surrounding tissues. Produced in pancreas, thyroid, pituitary gland Intercellular Connections • To protect other tissues, ET must be attached to one another by cell junctions. 3 types: Fig. 4-2 1. Tight – prevent water & solutes between cells, exposed to harsh chem or enzymes (dig tract lining protect from acids, wastes, dig enzymes) 2. Gap – held together by interlocked membrane prot, forms a narrow passage, movement of ions (cardiac & smooth muscle) 1. Desmosomes – thin layer of “protein fibers”, can be 1. Button - small discs 2. Belt - surround a cell 3. Hemidesmosomes (attach to basement membrane) • Very strong - can resist stretching – in skin, dead cells are shed in sheets Cell Attachments Epithelial Surface • Microvilli – absorption or secretions – digestive & urinary tracts • Cilia – to move substances across – respiratory tract Epithelial Surface See Fig. 4-3 b Basement Membrane • Holds cell to the underlying connective tissues • Made of protein fibers • Provides a barrier from underlying tissue into epithelial tissue Epithelial Renewal & Repair • Must continually repair & renew itself because of exposure to enzymes, bacteria, abrasion, chemicals • Survive ~ 1-2 days • Stem or germinative cells – division of these make new cells, near basement membranes Classifying Epithelia • Number of cell layers and shape of cell • Refer to figures in book • Layers: – Simple: 1 cell thick, in contact with basement membrane protect areas inside the body (line body cavities, blood vessels), secretion, absorption, gas exchange – thinness is an advantage – Stratified: multi cell thick, more protection. Areas that have mechanical or chemical stress (skin, linings of mouth) Epithelial – Cell Shape • Squamous – thin, flat, large nucleus (look like fried eggs from the top) • Cuboidal – squarish, form neat rows, nuclei in middle • Columnar – squarish, taller & thinner, nuclei near basement membrane • Refer to Figures 4-4 & 4-5 for cell examples Simple Squamous Epithelium Simple Cuboidal Epithelium Simple Columnar Epithelium Pseudostratified Epithelia • Looks stratified but all of the cells contact the basement membrane • Layered appearance – usually have cilia Transitional Epithelia • Withstands considerable stretching, seems to have many layers Stratified Squamous Epithelia • Where there is great mechanical stress Glandular Epithelia • Figure 4-6 • Contain gland cells – produce secretion • Endocrine – discharged into blood, surrounding tissue or tissue fluids – hormones • Exocrine – discharge onto internal or external surface (skin) or into a duct or tube Glandular Secretion Connective Tissue • Most diverse tissue – never exposed to outside environment – highly vascular • All have 3 basic components: 1. Specialized cells 2. Protein fibers 3. Ground substance – varies in consistency • Matrix that surrounds the cells – made of protein fibers & ground substance Connective Tissue - Functions: 1. Support, protect (bone) 2. Transport materials (blood, lymph) 3. Store energy reserves (adipose) 4. Defend body (antibodies) Classifying Connective Tissues Connective Tissue Proper Connective Tissue Proper - cell population • Fibroblasts - most abundant; produce & maintain connective fibers & ground sub. • Macrophages - phagocytize damaged cells or pathogens & release chem. that get the immune system going; fixed (long time) & free (an infected area) • Fat cells (adipose cells or adipocytes) - contains large drop of lipid (nucleus is squeezed to one side); # of cells differs depending on the area of body • Mast cells - small, mobile cells near blood vessels, cytoplasm is packed w/ vesicles that secrete chemicals after injury or infection • WBCs also present - produce antibodies (destroy pathogens or foreign substances) Connective Tissue Fibers • Collagen - most common; unbranched; strong & flexible; claimed to be "replenished" in skin cream ads • Elastic - contains elastin; branched; return to original length; prevents cheeks from remaining permanently disfigured when grandmother pinches them. • Reticular - least common; branching; form framework Ground Sub • Clear, colorless, maple syrup - slows pathogens down so phagocytes can catch them Connective Tissue is Characterized as 1. Loose 2. Adipose (type of loose) 3. Dense Loose Connective Tissue • Areolar tissue - little space • Packing material – fills spaces between organs, provides cushioning and support to epithelia tissue beneath skin • Has all cells & fibers • Lot blood vessels Loose Connective Tissue Adipose • Type of loose c.t. that is dominated by fat cells • Provides another source of padding, cushion, insulation that slows heat loss, storage for energy • Liposuction – removes unwanted adipose tissue temporarily Adipose Tissue (type of loose) Dense Connective Tissue • Tough, strong, durable • Consist mostly of collagen fibers • Tendons attach muscles to bones • Ligaments connect bones to bones. Dense Connective Tissue Fluid Connective Tissue • Distinct cells, no fibers • Blood - RBC (1/2 vol of blood); matrix is plasma containing WBCs & platelets (blood clotting) • Extracellular fluid - plasma, interstitial fluid & lymph. • Arteries (away from heart) & veins (to heart), water and solutes move from capillaries to tissues • Lymph (contain WBCs) carried in lymphatic vessels next to capillaries in tissues; returned to cardio system at vein Fluid Connective Tissue Cartilage – don’t have to know the 3 types • Matrix containing cartilage is a firm gel with fibers • Chondrocytes – only cells that live in the matrix • Covers bones between joints • Connects ribs to breastbone • Forms ear & ear canal • Between vertebrae in spine • Pads in knee joint (prevents bone-bone contact, limits movement, shock absorbers) • Heals slowly - avascular. Cartilage (Hyaline) Cartilage (Elastic) Cartilage (Fibrocartilage) Bone • Osseous tissue – bone cells are “osteocytes” • Not much ground substance • Matrix is mainly of hard calcium compounds & flexible collagen fibers – makes them strong & resists shattering. • See Table 4-2 (page 99) for comparison of bone & cartilage Bone – more on this later…. Membranes • At cellular level – lipid bilayer • At tissue level – form a barrier • Basement membrane that separates epithelia from connective tissue • Epithelia & connective tissue combine to form membranes that cover & protect other structures & tissues Muscle Tissue • Specialized for contraction • 3 types – Skeletal – Cardiac – Smooth • Contraction is the same, organization of their actin & myosin filaments is different Skeletal Muscle Tissue • Contain large, multinucleated cells held together by collagen & elastic fibers • Look striped because of the organization of the actin & myosin fibers • AKA “striated voluntary muscle” – don’t contract unless stimulated by nerves • Cannot divide, however, new muscle fibers are produced through divisions of stem cells in adult tissue – partial repairs can occur after an injury Skeletal Muscle Tissue Cardiac Muscle Tissue • Found only in the heart • Much smaller than skeletal fibers & usually have only 1 nucleus • AKA “striated involuntary muscle” • Do not rely on nerve activity – “pacemaker cells” establish a regular rate of contraction Cardiac Muscle Tissue Smooth Muscle Tissue • Found in the walls of blood vessels, around hollow organs (bladder) and in layers around various tracts (respiratory, circulatory, digestive, reproductive) • Small, slender, tapering to a point at each end, 1 nucleus • Actin & myosin are scattered throughout the cells so there are no striations (stripes) • AKA “nonstriated involuntary muscle” • Can divide – regenerate after injury Smooth Muscle Tissue Neural Tissue • Specialized to conduct electrical impulses that communicate info from one area of the body to another • 2 types of cells – Neurons: transmit info as electrical impulses in their cell membranes, longest cells in body, most cannot divide under normal circumstances & therefore have a very limited ability to repair themselves after injury – Neuroglia: supporting cells Neurons Tissue Injuries & Repair • Injuries affect several tissues at the same time – respond together • Requires 2 processes: – Inflammation – Repair or regeneration Inflammation • Isolates damaged tissue from healthy tissue – swelling, warmth, redness, pain • Damaged cells, tissue parts & pathogens are cleaned up. Infection – inflammation caused from pathogens • Mast cells stimulated – release histamine & heparin that cause bv to dilate & become more permeable. Skin becomes red, swollen, pain. Increases delivery of nutrients, oxygen and phagocytic wbc’s, blood clotting proteins, speed removal of waste products and toxins. Regeneration • Tissue is replaced or repaired to normal function • Fibroblasts produce dense collagen fibers (scar tissue) – over time this usually disappears • Epithelia, connective tissue – regenerate well • Smooth, skeletal muscle tissues – regenerate poorly • Cardiac and neural tissue – cannot regenerate • Therefore, different patterns of tissue organization dictate how each organ can regenerate after injury. Tissues & Aging • Decrease in the speed and effectiveness of tissue repair • Cumulative injuries from health problems or other damage, inactivity, diet, reduction in estrogens • Some effects are genetically programmed