* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download H.5 - HL transport-system
Cardiac contractility modulation wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Coronary artery disease wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Electrocardiography wikipedia , lookup
Artificial heart valve wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac surgery wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Atrial fibrillation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
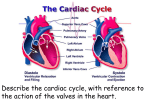
H.5 The Transport System IB Assessment Statement • H.5.1 Explain the events of the cardiac cycle, including atrial and ventricular systole and diastole, and heart sounds. The Cardiac Cycle • The cardiac cycle is the repetitive sequence of events in which the heart chambers contract and relax in a co-ordinated manner to send blood continuously around the circulatory system. • As with all cycles there is strictly speaking no one point that can be considered the beginning. The Cardiac Cycle Diastole: All heart muscle in state of relaxation. • Arterial blood pressure is greater than ventricle pressure. • The semilunar valves are closed • Ventricle pressures are still higher than atrial pressures • Atrio-ventricular valves closed. Atrial Distention • At this point the atria are both filling with blood from both the pulmonary veins and the vena cava. The Cardiac Cycle Atrial Distention: • The heart is still in a state of diastole. • All the valves are all closed. • The passive return of blood to the atria along veins causes the pressure to rise within the atria and the walls to distend. (swell) The Cardiac Cycle Note that this stage is still diastole: • The pressure in the atria is greater than the pressure in the ventricles. • The pressure difference causes the atrio-ventricular valve to open. • The ventricle passively fills with blood. • Note the semi-lunar valves are still closed. The Cardiac Cycle Early Atrial Systole • The atria contract together (see myogenic contraction). • The contraction of the atrial muscle reduces the volume of the atria. • This volume reduction increases the pressure on the blood within the atria. • The pressure increases forces the additional volume of blood into the ventricle. • This stretches the ventricle walls (Starlings Law). The Cardiac Cycle Systole: Contraction of the ventricles. • The ventricle walls contract on both sides. • There is a sudden pressure increase within the ventricles. • The pressure in the ventricles is greater than the pressure in the atria • Atrio-ventricular valves close. (First heart sound "Lub"). • Ventricle pressure is lower than arterial pressure. • Semi-lunar valves remain closed. • graph ref: (2) • Iso-volumetric contraction, in which the ventricle contracts increasing the blood pressure but the blood cannot yet pass out into the artery. This gives a sudden and large pressure increase. The Cardiac Cycle Systole continues • Ventricle pressure is greater than arterial pressure. • The semi-lunar valves open. • Blood ejects into the arteries (a pulse). • graph ref (4) • Pressure in the ventricles peaks rapidly as we come to the end of systole. • Note the atrio-ventricular valves are still closed (graph ref (5)) • As pressure falls in the ventricle the arterial blood will backflow closing the semi-lunar valves and creating the second heart sound, "dub". • graph ref: (6) • We now return to the first diagram in the cycle as we are back in a relaxed condition called diastole. IB ASSESSMENT STATEMENT • H.5.2 Analyse data showing pressure and volume changes in the left atrium, left ventricle and the aorta, during the cardiac cycle. Top-quality animations available from www.medmovie.com : Heart Pressure & Volume Changes during the Cardiac Cycle • a) Diastole (ventricles are relaxed) (b) Systole (ventricles contracted) • (1) Atrial systole • (2) Ventricular Systole , atrioventricular valves close, first heart sound. • (3) Iso-volumetric contraction • (4) Opening semi-lunar valves • (5) Peak of systolic pressures Heart Pressure & Volume Changes during the Cardiac Cycle • (6) End of ventricular systole, closure of the semi-lunar valves, second heart sound. Beginning of diastole • (7) Aorta pressure during ventricular diastole • (8) Falling ventricular pressure (Diastole) • (9) Passive atrial filling with blood/ compression from systole • (10) Passive filling blood by venus return IB ASSESSMENT STATEMENT • H.5.3 Outline the mechanisms that control the heartbeat, including the roles of the SA (sinoatrial) node, AV (atrioventricular) node and conducting fibres in the ventricular walls Control of the Heart Myogenic Rhythm: The heart beat is initiated within the heart muscle itself. • Within the right atrium there are a specialise group of cells called the Sino Atrial Node.(SAN). • These cells can generate an electrochemical potential across the cell membrane and once threshold is reached this can be propagated across the other cells of both atria. • The speed of conduction across the two atria is fast enough that both effectively contract together. • However the cell membrane structure alters across a line rough consistent with the diagram and effectively prevents the conduction of the contraction stimuli traveling down into the ventricles. Control of the Heart a) The impulse is picked up by a specialised group of cells in the right atrium wall called the Atrio-Ventricular Node (AVN). (b) The AVN conducts the impulse down through the central septum of the heart along specialised fibres called the Purkinje fibers. The fibres are insulated from the muscle and do not cause contraction. Control of the Heart . c) The impulse emerges into the muscle at the apex of the heart so that the ventricular contraction begins at the apex. d) The impulse travels on emerging into the heart muscle higher up the ventricle wall in this way the contraction spreads upwards. •Note that this direction of contraction pushes the blood towards the semi-lunar valve and also not that the transmission time down the Purkinje tissue creates a delay between atrial and ventricular systole. This delay maintains the correct directional flow of blood through the different chambers Control of the Heart • Myogenic Rhythm can be modified by the central nervous system to respond to cardiovascular demands. • Within the medulla region of the brain there are a specialised group of receptors and coordinators called the Cardiac Centre. • These are connected to the the SAN via the two sets of nerves. • a) Accelerator nerve that increases the rate SAN activity to produce faster heart rate. • b) Decelerator nerve that decreases the rate SAN activity to slow heart rate. • In addition the SAN is sensitive to hormones such as adrenaline that can directly stimulate heart rate. • The brain is sensitive to a wide range of stimuli including pH and CO2 levels which reflect the demand of the tissues for oxygen. As an example, exercise produces more CO2 in the plasma. Detected by the cardiac centre this stimulates the accelerator nerve and therefore the SAN to increase heart rate. ie your heart beats faster when you exercise Electrocardiogram (EKG or ECG) • An electrocardiogram (EKG or ECG) is a measure of the electrical currents from the heart, measured on the surface of the body. EKG http://library.med.utah.edu/kw/pharm/hyper _heart1.html) IB Assessment Statements • H.5.4 Outline atherosclerosis and the causes of coronary thrombosis. Atherosclerosis is a stage of arteriosclerosis involving fatty deposits (atheroma's) inside the arterial walls The sequence of events in the build up of the atheroma: 1) damage to the arterial wall (perhaps due to high blood pressure) 2) attachment of phagocytes which secrete growth factors 3) enlargement of the muscle layer 4) permeability of the endothelium to low density lipoproteins (LDL) 5) deposition of cholesterol from LDL 6) crystallisation of cholesterol 7) reduction of the lumen space of the artery 8) decreased or interrupted flow 9) turbulence in blood flow can produce clots (thrombosis) 10) thrombosis in the coronary artery may block blood flow to heart muscle (myocardial infarction)resulting in tissue damage or death IB Assessment Statements • H.5.5 Discuss factors that affect the incidence of coronary heart disease.