* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Myocardial structure, function and ischaemic tolerance in a rodent
Survey
Document related concepts
Transcript
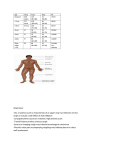
Griffith Research Online https://research-repository.griffith.edu.au Myocardial structure, function and ischaemic tolerance in a rodent model of obesity with insulin resistance Author Wensley, Isaac, Salaveria, Kris, Bulmer, Andrew, Donner, Dan, Du Toit, Eugene Published 2013 Journal Title Experimental Physiology DOI https://doi.org/10.1113/expphysiol.2013.074948 Copyright Statement Copyright 2013 The Physiological Society. This is the author-manuscript version of the paper. Reproduced in accordance with the copyright policy of the publisher. The definitive version is available at http://onlinelibrary.wiley.com/ Downloaded from http://hdl.handle.net/10072/58610 Myocardial Structure, Function, and Ischaemic Tolerance in a Rodent Model of Obesity with Insulin Resistance. I. Wensley, K. Salaveria, A.C. Bulmer, D.G. Donner, E.F. du Toit. Heart Foundation Research Centre, Griffith Health Institute Griffith University Gold Coast, Southport QLD 4222, Australia. Running Title: Obesity and Cardiac Function and Ischaemic Tolerance Keywords: Ischaemia-reperfusion; Myocardial Infarction; Echocardiography; Obesity; Reperfusion Injury; Reperfusion Injury Salvage Kinase. Corresponding Author: Dr. E.F. Du Toit School of Medical Science Griffith University Southport QLD 4222 AUSTRALIA Ph: (+61) 7 55 529728 Fax: (+61) 7 55 528908 E-mail: [email protected] 0 Central question • Does obesity with insulin resistance decrease left ventricular pump function and/or myocardial tolerance to ischaemia in a rodent model of metabolic syndrome and, • What mechanisms are involved in these changes? Findings and its importance • These data suggest that although left ventricular pump function may be maintained with obesity and insulin resistance, the hearts from these animals are more prone to ischaemia/reperfusion injury which is in part due to changes in the functionality of the myocardial RISK pathway. • Interventions/therapies aimed at normalising RISK pathway function have the potential to normalise myocardial tolerance to ischaemia/reperfusion in patients with the metabolic syndrome. 1 Abstract Obesity and its co-morbidities (dyslipidaemia, insulin resistance and hypertension) that together constitute the metabolic syndrome (MetS) are all risk factors for ischaemic heart disease (IHD). Although obesity has been reported to be an independent risk factor for congestive heart failure (CHF), whether obesity induced heart failure develops in the absence of increased afterload (induced by hypertension) is not clear. We have previously shown that obesity with insulin resistance decreases myocardial tolerance to ischaemia/reperfusion but the mechanisms for this decreased tolerance remains unclear. We hypothesise that obesity with insulin resistance induces: 1) adverse cardiac remodelling and pump dysfunction and, 2) adverse changes in myocardial pro-survival RISK pathway signalling to reduce myocardial tolerance to ischaemia/reperfusion. Wistar rats were fed an obesogenic (Obese) or a standard rat chow diet (Control) for 30 weeks. Echocardiography was performed over the 32 weeks before isolated Langendorff perfused hearts were subjected to 40 min coronary artery ligation followed by reperfusion and functional recovery (Rate Pressure Product-RPP), infarct size, and RISK pathway function assessed (Western blot analysis). Obesity with insulin resistance increased myocardial lipid accumulation but had no effect on in vivo or ex vivo left ventricular structure/function. Hearts from obese rats had lower reperfusion RPPs (13115±562 bpm*mmHg for obese vs. 17781±1109 bpm*mmHg for control, p<0.05) and larger infarcts (36.3±5.6% of AAR in obese vs. 14.1±2.8% of area at risk in control rats, p<0.01) as compared to control hearts. These changes were associated with reductions in RISK pathway function with 30-50%, and 40-60% reductions in Akt and GSK-3β expression and phosphorylation respectively in obese rat hearts compared to controls. Total eNOS expression was reduced by 25% in obese rats. We conclude that obesity with insulin resistance had no effect on basal cardiac structure or function but decreased myocardial tolerance to ischaemia/reperfusion. This reduction in ischaemic tolerance was likely due to compromised RISK pathway function in obese insulin resistant animals. 2 Introduction The alarming increase in the incidence of obesity and its comorbidities (dyslipidemia, insulin resistance/type II diabetes and hypertension) has led to an increased incidence of the metabolic syndrome (MetS) (Eckel et al., 2005). Individually, these cardiometabolic abnormalities represent risk factors for cardiovascular disease and acute myocardial infarction (AMI) (Kannel et al., 1961; Kannel et al., 1965). Besides increasing the risk of coronary artery disease (CAD) by promoting atherosclerosis, obesity is also an independent risk factor for heart failure (Kenchaiah et al., 2002) which is seemingly caused by abnormal myocardial triglyceride accumulation and lipotoxicity associated with obesity (Christoffersen et al., 2003; Polidori et al., 2009). Lipotoxicity has the potential to compromise myocardial pro-survival kinase function (Reperfusion Injury Salvage Kinase – RISK pathway) to promote apoptosis which could induce adverse cardiac remodeling and decrease left ventricular (LV) function and tolerance to ischaemia (Chess et al., 2008). Ourselves (Majane et al., 2009) and others (Avelar et al., 2007; Norton et al., 2009; Wang et al., 2010) have demonstrated that obesity may accelerate hypertension induced cardiac remodelling and left ventricular dysfunction. Our data (Majane et al., 2009) suggests that in combination with hypertension, obesity promotes cardiomyocyte apoptosis, LV dilatation and pump dysfunction. Several other mechanisms for obesity induced cardiac remodelling have however been proposed (Alpert, 2001; Chess et al., 2008; Lopaschuk et al., 2007). Increased blood volume (Alpert, 2001) and insulin resistance (Chess et al., 2008) associated with obesity have been implicated in the aetiology of obesity induced cardiac remodelling and LV pump dysfunction. Lipotoxicity, Cardiac Remodelling and Ventricular Dysfunction: Lipotoxicity caused by abnormal myocardial lipid accumulation plays an important role in cardiac remodelling and loss of function in obesity (Chess et al., 2008; Lopaschuk et al., 2007). Although lipids are continually taken up and metabolised by the myocardium, elevated myocardial acetyl-CoA in obesity exceeds the myocardial ability to metabolise acetyl-CoA (Lee et al., 2006). Accumulated acetyl-CoA serves as a precursor in non-oxidative pathways, resulting in the formation of diacylglycerol (DAG), ceramide and triglycerides (Trigs) (Chess et al., 2008; Lopaschuk et al., 2007). DAG increases protein kinase C (PKC) activation while ceramide promotes mPTP opening and apoptosis (Agudo-Lopez et al., 2011; Chess et al., 2008). 3 Lipotoxicity also promotes ER stress, ER reactive oxygen species (ROS) formation and apoptosis (Gustafsson et al., 2007; Lu et al., 2007; Nishida et al., 2008; Santos et al., 2011). Insulin Resistance, Cardiac Remodelling and Mechanical Dysfunction: Obesity with dyslipidaemia is closely associated with insulin resistance (Turinsky et al., 1990; Yu et al., 2002; Zhang et al., 2010) which plays a key role in both LV pump dysfunction (Buchanan et al., 2005; Ouwens et al., 2007) and myocardial ischaemic intolerance in obesity (du Toit et al., 2005; du Toit et al., 2008; Nduhirabandi et al., 2011). The hyperinsulinaemia of insulin resistance could also contribute to abnormal cardiac remodelling and LV pump dysfunction through the growth promoting properties of insulin (Abel et al., 2008). Besides its metabolic and growth promoting effects, insulin resistance also adversely affects insulin receptor activation of the pro-survival PI3K-Akt pathway (Dhanasekaran et al., 2008). These signalling changes potentially contribute to left ventricular cell loss, wall thinning (Millis et al., 2012), and decreased LV pump function (Young, 2010). Metabolic Syndrome and Ischaemic Tolerance: Ourselves (Clark et al., 2011; du Toit et al., 2005; du Toit et al., 2008; Essop et al., 2009; Maarman et al., 2012; Nduhirabandi et al., 2011) and others (Bouhidel et al., 2008; Katakam et al., 2007; Wagner et al., 2008) have shown that diet induced obesity with insulin resistance (MetS) decreases myocardial resistance to ischaemia/reperfusion injury. Clinically, MetS is strongly associated with increased incidence of myocardial infarction (Ninomiya et al., 2004) and an increase in morbidity after an acute myocardial infarction (Clavijo et al., 2006). Despite compelling evidence to suggest that obesity with insulin resistance (MetS) decreases myocardial tolerance to ischaemia in humans and animal models, the cellular mechanisms for this decreased ischaemic tolerance is poorly understood. The ability of the heart to withstand injury during ischaemia/reperfusion depends in part upon normal expression and functionality of pro-survival RISK pathways (Downey et al., 2007; Halestrap et al., 2007; Hausenloy et al., 2009). The RISK pathway comprises cell surface Gprotein coupled receptors (GPCRs), a signalling kinase network (e.g. PI3K-Akt-eNOS, Erk1/2, PKC, p38-MAPK, GSK3β), and the end effectors (K ATP channels and the mitochondrial permeability transition pore - mPTP). Central to this pathway is the pro- 4 survival/anti-apoptotic protein kinase PKB/Akt which is also key in both myocardial insulin signalling (Bertrand et al., 2008) and myocardial hypertrophy (Bernardo et al., 2010). Changes in insulin signalling as occurs in insulin resistance may therefore have a significant impact on functionality of the RISK pathway. Although we have previously shown that MetS decreases myocardial tolerance to ischaemia in our rodent model, the mechanisms for this decreased ischaemic tolerance have not been elucidated and were investigated in this study. We also set out to determine whether obesity with insulin resistance causes adverse cardiac remodeling and cardiac dysfunction and, whether cellular mechanisms implicated in obesity induced cardiac remodeling are involved in this model. We hypothesized that MetS induces adverse cardiac remodeling and LV pump dysfunction and decreases myocardial tolerance to ischaemia by compromising myocardial RISK pathway functionality. We assessed myocardial morphology, mechanical function, infarct size and the expression and activation of signaling proteins (Akt, GSK-3β, eNOS, Bcl2 and Bax) implicated in myocardial RISK signaling and apoptosis in lean and in obese, insulin resistant rats. Methods Ethical approval All studies were approved and performed in accordance with the guidelines of the Animal Ethics Committee of Griffith University, which is accredited by the Queensland Government, Department of Primary Industries and Fisheries under the guidelines of The Animal Care and Protection Act 2001, section 757. Animals Rats were housed at the Griffith University Animal Facility on a 12-hour day/night cycle with room temperature maintained at 23oC. Thirty male Wistar rats (8 week old) were randomly assigned to either a control diet (Control) or high fat diet (Obese) for 32 weeks to induce dietary obesity with insulin resistance and MetS. Standard rat chow contained: 70% carbohydrates, 24% proteins and 6% fat while the HFD contained: 70% carbohydrates, 15% proteins and 15% fat). Both groups were allowed ad libitum access to fresh food and water daily. Seven rats from each dietary group were randomly assigned for ex vivo Langendorff perfusion experiments. Left ventricular function before and after 40 min coronary artery ligation (CAL) was assessed and infarct size quantified. The remaining 8 rats from each 5 group were used for myocardial sample collection for biochemical analysis of blood, Western Immunoblot analysis, hydroxyproline determination and histology. Biochemical Analyses Animals set aside for biochemical analyses were anaesthetised, blood collected and heart excised. Peritoneal and retro-peritoneal fat was removed and weighed. Serum triglycerides, high density lipoprotein (HDL) cholesterol and glucose levels were determined in fresh whole-blood using a Blood-Lipid and Glucose Analyser (L.D.X. Cholestech Analyser, Alere™, Australia). For serum analysis, remaining blood samples were placed in serum separation tubes (BD Vacutainer tubes), centrifuged and serum stored at -80 °C for later analysis. Levels of insulin (ALPCO Immunoassays™, Salem) were determined in 96-well enzyme-linked immunosorbant assay’s (ELISAs) according to manufacturer instructions. To assess insulin resistance in control and obese animals the homeostasis model assessment (HOMA) index was determined. Fasting blood glucose and insulin levels were used to determine the HOMA index using the standard formula: [fasting insulin (μIU/ml) x fasting glucose (mmol/l)] / 22.5. Assessment of in vivo Cardiac Structure and Function Using Echocardiography Echocardiography was performed at 4 week intervals to assess myocardial dimensions and mechanical function. A 710B ultrasound scanhead (Visualsonics) and a Vevo 770 High Resolution In Vivo Micro-imaging System (Visualsonics) was used to determine cardiac dimensions in all echocardiographic analysis. The scanhead was mounted on a purpose built micromanipulator and stage on which the rat was placed and secured. All rats were anaesthetised (5% isofluorane, (Delvet, Australia) in 100% medical-grade oxygen), placed on the micromanipulator stage, ECG electrodes attached with ECG and heart and respiration rates recorded throughout the procedure. Core temperature was monitored using a rectal thermometer and maintained at 37oC. Parasternal long axis imaging was used to quantify left ventricular dimensions using M-mode imaging. Left ventricular wall thickness and chamber width was measured at the left anterior papillary muscle. Parasternal short axis imaging was achieved by rotating the scanhead through 90-degrees and repeating the measurements using M-mode imaging. All anatomical 6 M-mode images were quantified in accordance with the American Society of Echocardiography’s border definitions (Foppa et al., 2005). Ex Vivo Heart Perfusions Rats were anaesthetized (60 mg/kg sodium pentobarbital i.p.) and hearts perfused in a Langendorff mode as described in detail previously (du Toit et al., 2005; du Toit et al., 2008; Essop et al., 2009; Maarman et al., 2012; Nduhirabandi et al., 2012). Briefly, hearts were excised into ice-cold perfusion fluid, the aorta cannulated and coronary vessels perfused at a pressure of 100 cm H 2 O with modified Krebs- Henseleit buffer containing (in mM): 118 NaCl, 25 NaHCO 3 , 4.7 KCl, 1.75 CaCl 2 , 1.2 MgSO 4 , 11 D-glucose, and 0.5 EDTA. Perfusion fluid was saturated with 95% O 2 -5% CO 2 at 37°C giving a pH of 7.4. A fluid-filled polyvinyl chloride film balloon was inserted into the left ventricle and connected to a P23XL pressure transducer (Viggo-Spectramed, USA) for measurement of ventricular pressure. Balloon volume was adjusted to an initial end-diastolic pressure of 4-6 mmHg and then left unchanged. Functional data were recorded at 1 KHz on a 4-channel MacLab system (ADInstruments, Australia) connected to an Apple iMac computer. Peak systolic, diastolic and developed pressures, heart rate, and rates of contraction or relaxation over time (dP/dt) were documented. Coronary flow was monitored via volumetric analysis of coronary effluent. After balloon placement, hearts were immersed in a water-jacketed chamber maintained at 37°C. Temperature of perfusion fluid was monitored by a needle thermometer probe (Model 52II, Fluke Corporation, Australia) in the coronary sinus. Hearts were excluded from study after a 15-min stabilization period if they failed to meet any of the following functional criteria: i) coronary flow >25 ml/min, ii) unstable (fluctuating) contractile function, iii) left ventricular systolic pressure <90 mmHg, or iv) significant cardiac arrhythmias. After an initial 15 min stabilization period hearts were switched to ventricular pacing at 300 beats/min (Grass S9 stimulator, Quincy, USA), normalizing rate to allow comparison of ratedependent measures of contractile function (systolic and developed ventricular pressures) and inotropic state (dP/dt). Baseline measures were made at 10 min intervals for 30min before hearts were subjected to 40 min coronary artery ligation (normothermic regional ischemia) followed by 120 min of aerobic reperfusion. Pacing was terminated on initiation of ischemia 7 and resumed after 5 min of reperfusion. Myocardial Infarct Size Quantification At the end of reperfusion hearts were stained with Evan’s blue dye (Sigma, USA), frozen at – 20 °C overnight and triphenyltetrazolium chloride (TTC) stained the following morning to define area at risk and viable and infarcted myocardium. Infarct size was expressed as a percentage of the area at risk and was quantified by volumetric planimetry using a flat-bed scanner for image capture and computer software for analysis (UTHSCSA Image Tool, V3). Western Immunoblot Analyses Left ventricular tissue samples were homogenized in lysis buffer (50 mmol/l HEPES, 150 mmol/l NaCl, 1.5 mmol/l MgCl 2 , 1 mmol/l EGTA, 10% glycerol plus 8.6 μmol/l leupeptin, 5.8 μmol/l pepstatin A, 4 mmol/l phenylmethylsulfonyl fluoride, 0.6 μmol/l aprotinin, 4 mmol/l sodium fluoride, and 0.8 mmol/l sodium orthovanadate) and centrifuged at 10000 g for 15 min to remove nuclei and debris. Since protein activation processes may involve translocation from soluble to particulate fractions, we investigated expression of total and phosphorylated protein in both membrane and cytosolic fractions. The supernatant was centrifuged at 10,000 g to enrich for the cytosolic fraction, with the pelleted membrane fraction re-suspended by ultra-sonication in a lysis buffer containing 1% Triton X. Fraction protein concentrations were determined by the Pierce assay. Equal quantities of protein (35 μg) were subsequently loaded onto 10% Tris–HCl gels and after electrophoresis (150 V, 1.5 h), transferred to PVDF membranes (50 V, 2 h). Membranes were blocked with 3% bovine serum albumin solution followed by probing overnight with antibodies (Cell Signalling Technology Inc., Danvers, MA, USA) for total or phosphorylated Akt (Ser473), GSK-3β (Ser9), eNOS (Ser1177), Bax, Bcl-2 followed by secondary antibody application (1:2500, Cell Signalling; 1:10 000, Santa Cruz) and ECL. Equal sample loading was confirmed by co-analysis of actin or GAPDH. Protein was detected by X-ray film, and densitometry assessed using NIH Image 1.63, with total expression and phosphorylation ratios normalized to values for untreated control (CD) tissue for the purposes of comparison across groups. Histology and Oil Red-O staining Heart tissue samples collected at the time of sacrifice were mounted in optimum cutting temperature (OCT) compound (Tissue-Tek), and stored at -80°C until processed. Sections 8 were cut (10μm widths) using a CM1850 microtome (Leica) and mounted on Superfrost Plus slides (Lomb). Slides were air dried for 60 min and fixed in ice-cold formalin for 10 min before being rinsed three times using distilled water. Sample dehydration was achieved by transferring slides into 100% propylene glycol for 5 min before being stained in 60°C Oil Red-O solution (composed of 0.5% Oil Red-O stain in 100% propylene glycol). Slides were differentiated in 85% propylene glycol for 2 min, followed by two rinses in distilled water. They were then transferred into Mayer’s haematoxylin for 30 sec to stain for nuclei. Once removed from Mayer’s haematoxylin, slides were rinsed in distilled water, before a drop of glycerine jelly was applied to the slide for mounting. Photomicrographs were taken at 20x optic zoom using a B201 light microscope (Olympus, Australia). Lipid content in the sections was quantified using Daime digital image analyser (version 2). Hydroxyproline assay for myocardial total collagen content Myocardial hydroxyproline content was determined using methods described previously (Majane et al., 2009; Stegemann et al., 1967). Statistical Analyses Unless otherwise stated, all results are expressed as means ± S.E.M. A two-tailed Student’s ttest was employed to contrast measures between control and obese groups, with multi-way ANOVA used for multiple comparisons. Evidence of statistical significance was accepted for P<0.05. 9 Results Characteristics of Obese and Lean Animals Rats on the HFD became obese with 20% greater body mass and two-fold increases in visceral fat content (Table 1). HFD fed rats were dyslipidaemic with a two-fold increase in serum triglyceride levels in obese rats. Fasting blood glucose levels were comparable between the two groups however HOMA-IR indices and insulin levels were elevated in the obese, HFD fed rats compared to controls (Table 1). In Vivo Cardiac Structure and Function Cardiac morphology and left ventricular function was assessed at 4 week intervals for 22 weeks of the 32 week feeding program to monitor myocardial structural remodelling during the development of obesity. Posterior wall thickness and left ventricular mass remained unchanged between the two groups (Table 2). Left ventricular mechanical function (ejection fraction, fractional shortening, stroke volume and cardiac output) was assessed and remained similar over the 22 weeks for the two groups. Ex vivo Pre-ischaemic and Reperfusion Myocardial Function Rate pressure product (RPP) was assessed before and after 40 min CAL. Pre-ischaemic RPP was similar in the two groups of animals (25867±1376 bpm*mmHg for the Control hearts vs. 22240±1112 bpm*mmHg for the Obese hearts). Reperfusion RPP was however reduced in hearts from the obese rats throughout reperfusion (Figure 1). RPP after 120 min reperfusion was 18564±963 for the control hearts and 13116±562 for the obese rat hearts (p<0.05). Impact of Obesity on Myocardial Infarct Size Hearts from the obese rats had larger myocardial infarct sizes after 40 min CAL than the lean littermate controls (36.28±5.56% for Obese vs. 14.14±2.8% of the area at risk for Controls, p=0.004) (Figure 2). 10 Myocardial Lipid and Hydroxyproline Content Lipids: Oil red-O staining indicated greater intracellular and extracellular triglyceride accumulation in the hearts from the obese animals than the controls. One of the 8 control hearts stained positive for intracellular lipids while 7 of the 9 obese rat hearts stained positive for intracellular lipid droplets (p=0.015). Three of 8 control hearts and 6 of 9 obese hearts stained positive for extracellular lipids in the myocardium (p=0.23) (Figure 3A&B). The increase in myocardial lipid content in obese hearts is further demonstrated by a 36-fold increase in the total tissue triglyceride content compared with the lean hearts (Figure 3B). Collagen content: Myocardial collagen content as assessed from total myocardial hydroxyproline concentrations was similar in the control and obese rat hearts (0.90±0.02 µg/mg w.w. for control (n=8) and 0.65±0.08 µg/mg w.w. for obese rat hearts (n=8), p=0.21). Myocardial Expression of Pro- and Anti-Apoptotic Proteins There were no differences in the myocardial expression of the pro-apoptotic Bax or the antiapoptotic Bcl-2 in the hearts from obese animals compared with their control littermates. Expression and Activity/Phosphorylation of RISK Pathway Proteins Both total and phosphorylated Akt expression was decreased (p<0.05)in the membrane and cytosolic fractions of the hearts from obese rats (Figure 4A & 4B). Myocardial total GSK-3β expression was decreased in the cytosolic and membrane fractions of the hearts from obese rats (Figure 5A) while phospho-GSK-3β expression was reduced in the cytosolic but not in the membrane fraction of hearts from the obese rats (Figure 5B). Endothelial NOS was only present in the membrane fraction of the myocardium with total eNOS expression being reduced in the hearts from the obese rats (Figure 6). 11 Discussion In this study we demonstrate that diet induced obesity causes dyslipidaemia and insulin resistance. These obesity induced changes were associated with increased myocardial lipid accumulation without promoting myocardial pro-apoptotic signaling, adverse cardiac remodeling or LV pump dysfunction. The hearts from the obese, insulin resistant (MetS) rats were however less resistant to ischaemia/reperfusion injury and had larger infarcts and poorer reperfusion LV function compared to those from lean insulin sensitive littermates. The decrease in myocardial ischaemic tolerance in the obese, insulin resistant animals was associated with decreased basal expression and/or phosphorylation of key pro-survival kinases of the RISK pathway. Effects of Obesity on Cardiac Structure and Function Obesity induced changes in cardiac structure may be elicited directly by obesity induced increases in cardiac loading conditions (preload and afterload) or indirectly by obesity induced cardio-metabolic abnormalities such as dyslipidaemia and insulin resistance/diabetes. In obesity chronically elevated circulating free fatty acids cause abnormal tissue triglyceride accumulation and lipotoxicity which potentially promotes apoptosis and adverse cardiac remodeling (Christoffersen et al., 2003; Polidori et al., 2009). Role of Obesity Induced Insulin Resistance in Cardiac Remodelling: Obesity induced insulin resistance (with associated hyperinsulinaemia) may induce cardiac remodelling via the growth promoting properties of insulin (Abel et al., 2008) or by attenuating the anti-apoptotic signaling of the PI3K-Akt pathway elicited by insulin receptor activation (Dhanasekaran et al., 2008). These changes potentially contribute to abnormal rates of apoptosis, LV wall thinning and adverse remodelling (Millis et al., 2012). Lipotoxicity and Apoptosis: Lipotoxicity caused by abnormal intracellular lipid accumulation potentially plays an important role in cardiac remodelling and loss of function in obesity (Chess et al., 2008). Although lipids are continually taken up and metabolised by the myocardium, the levels of acetyl-CoA in the myocardium in obesity exceed its ability to metabolise acetyl-CoA (Lee et al., 2006) causing DAG, ceramide and Trigs accumulation (Lopaschuk et al., 2007). Elevated myocardial ceramide concentrations increase PKC-ε activation which promotes mPTP opening, cytochrome c release and apoptosis (Agudo12 Lopez et al., 2011; Chiu et al., 2001). Lipotoxicity also causes ER stress, increased ER ROS formation and mitochondrial mPTP opening (Santos et al., 2011) which suppresses prosurvival Bcl-2 expression (Lu et al., 2007) and promotes the translocation of pro-apoptotic Bax and Bad to the mitochondrial membrane (Gustafsson et al., 2007), where they form a channel that facilitates cytochrome c release (Nishida et al., 2008). We have previously shown that obesity promotes cardiac dilatation and pump dysfunction in spontaneously hypertensive rats (SHR) and that these changes in cardiac structure and function were associated with increased myocardial apoptosis and collagenase (MMP-2) activity in obesity with hypertension (Majane et al., 2009). In the current study we used echocardiography to track possible changes in LV structure (LV mass, anterior and posterior wall thickness and LV volume) and function (fractional shortening, stroke volume, cardiac output and ejection fraction) in our normotensive lean insulin sensitive and obese insulin resistant rats. There were no differences in these parameters in the obese, insulin resistant animals when compared to their lean insulin sensitive littermates. These data suggest that in vivo cardiac structure was unchanged by obesity with insulin resistance and support our previous observations in Wistar rats (Majane et al., 2009) and those of others (Carroll et al., 2006) who demonstrated no change in several measures of cardiac structure/morphology in normotensive, obese, insulin resistant rats. Although data from our previous study in SHRs suggests that obesity may promote apoptosis and cardiac dilatation in these hypertensive rats the data from the current study support our observations regarding the effects of isolated obesity (without hypertension) on cardiac remodelling. Despite evidence to suggest that there was myocardial lipid accumulation in the obese, insulin resistant rats (Figure 3), there were no differences in myocardial Bcl-2 and Bax expression in the hearts from the obese rats when compared with lean controls. The effect of obesity with insulin resistance on myocardial function is controversial. Clinical studies have reported unaltered LV function (Stoddard et al., 1992; Peterson et al., 2004) diastolic dysfunction (Berkalp et al., 1995; Pascual et al., 2003; Peterson et al., 2004; Stoddard et al., 1992; Zarich et al., 1991) or subclinical systolic dysfunction (Scaglione et al., 1992; Wong et al., 2006) in obese patients. In animal models obesity and insulin resistance has been reported to increase (Buchanan et al., 2005), have no effect (Mazumder et al., 13 2004), or decrease left ventricular function in rabbits (Carroll et al., 1997), rats (du Toit et al., 2008; Wilson et al., 2007) and mice (Aasum et al., 2008). Contrary to our current findings suggesting that obesity with insulin resistance has no effect on in vivo cardiac function, studies have documented cardiac dysfunction in lean insulin resistant animals (Ouwens et al., 2007; Vasanji et al., 2006). In one of these studies (Ouwens et al., 2007) rats were however hypo-insulinaemic and hyperglycemic which would suggest they were overtly diabetic. In addition, since insulin is known to have some positive inotropic effects (Baron, 1994; Ferrannini et al., 1993) the hypo-insulinaemia in these animals may have contributed to the decreased contractile function observed in this study. Similar decreases in ex vivo cardiac function in insulin resistant obese rats (Wold et al., 2005) and mice (Dong et al., 2006) have been documented using isolated heart models to assess LV function. These studies were however performed without fatty acids or insulin in the perfusion medium which may contribute to the cardiac dysfunction observed. Other research groups have demonstrated a dependence of hearts from obese, insulin resistant animals on elevated free fatty acid and insulin levels for the maintenance of normal left ventricular systolic function (Buchanan et al., 2005; Mazumder et al., 2004). Data obtained from the ex vivo experiments support our echocardiography data. No changes in basal LV function (RPP) were observed with obesity and insulin resistance when assessed using the Langendorff perfusion model (Figure 1). Although these data are contrary to our previous observations using the working heart model (du Toit et al., 2005; du Toit et al., 2008; Nduhirabandi et al., 2011), they support our findings (Maarman et al., 2012) indicating that cardiac functional deficits are not detected in these insulin resistant hearts when function is assessed using the isovolumic Langendorff perfusion heart model. These discrepancies are evidently due to differences in loading conditions between the two ex vivo heart perfusion models and are not yet fully understood. Effect of Obesity with Insulin Resistance on Myocardial Tolerance to Ischaemia We have previously shown that the hearts from obese insulin resistant animals are less tolerant of ischaemia/reperfusion (Clark et al., 2011; du Toit et al., 2005; du Toit et al., 2008; Essop et al., 2009; Maarman et al., 2012; Nduhirabandi et al., 2011) than their lean insulin sensitive littermates. Although we were able to demonstrate that chronic angiotensin receptor 14 antagonism with losartan (du Toit et al., 2005), CPT-1 inhibition with oxfenicine (Maarman et al., 2012), antioxidant treatment with melatonin (Nduhirabandi et al., 2011), or insulin treatment during ischaemia (du Toit et al., 2008) improved myocardial ischaemia/reperfusion tolerance in these animals, the cellular mechanisms for this reduced ischaemic tolerance are not well understood. The ability of the heart to withstand injury during ischaemia/reperfusion depends in part upon normal expression and functionality of pro-survival RISK pathways which comprises of cell surface GPCRs, a signalling kinase network (e.g. PI3K-Akt-eNOS, Erk1/2, PKC, p38MAPK, GSK3β), and the end effectors (K ATP channels and the mitochondrial permeability transition pore – mPTP) (Downey et al., 2007; Halestrap et al., 2007; Hausenloy et al., 2009). Activation of the RISK pathway during ischaemia and particularly during reperfusion confers myocardial protection against ischaemia/reperfusion injury and is believed to be the underlying mechanism for the protection elicited by both pre- and post-conditioning. Previous studies have investigated the effects of obesity on myocardial responses to preconditioning and post-conditioning and demonstrated that these hearts are refractory to these cardioprotective interventions (Bouhidel et al., 2008; Katakam et al., 2007; Wagner et al., 2008). Reduced responsiveness to ischaemic preconditioning (Wagner et al., 2008) and impaired expression/activation of RISK pathway proteins (Nduhirabandi et al., 2011) suggest that dysfunctional pro-survival signalling may contribute to the ischaemic intolerance in obesity with insulin resistance. In this study we report that although obesity with insulin resistance had no effect on the expression of proteins directly implicated in apoptosis (Bcl-2 and Bax), hearts from obese animals had compromised basal expression and activation/phosphorylation of proteins involved in pro-survival RISK pathway signalling (Figures 4-6). Not only was the expression of various proteins decreased in obese insulin resistant rat hearts, but phosphorylation/activation of these proteins was also decreased. These data provide evidence to suggest that compromised RISK pathway function may be involved in the decreased myocardial tolerance to ischaemia/reperfusion seen in obese, insulin resistant hearts. The clinical importance of the elucidation of the mechanistic pathways underlying decreased myocardial tolerance to ischaemia/reperfusion in obesity and insulin resistance cannot be 15 overstated. The current data suggest compromised RISK pathway functionality in these animals. Pharmacological activation and manipulation of the RISK pathway may be effective in reducing the severity of ischaemia/reperfusion injury in obese, insulin resistant AMI patients and patients undergoing elective cardiac surgery. Several clinical studies have already demonstrated that pharmacological interventions that activate the RISK pathway (Kloner et al., 2006; Nikolaidis et al., 2004; Piot et al., 2008) or block the mPTP (Piot et al., 2008) improve percutaneous coronary intervention (PCI) outcomes and may be particularly effective in an obese insulin resistant patient cohort. The Impact of Fatty Acids on Myocardial Ischaemia/Reperfusion Injury: There is strong evidence to suggest that elevated circulating fatty acids as seen in obesity may adversely affects myocardial tolerance to ischaemia (Kantor et al., 1999; Liedtke et al., 1988). Although fatty acids were not included in the perfusion medium in the current study we have previously investigated the effects of fatty acids and insulin on myocardial tolerance to ischaemia in this model of MetS (du Toit et al., 2008). We found that although the inclusion of insulin in the perfusion medium improved myocardial tolerance to ischaemia in both the lean and obese insulin resistant rat hearts, the addition of free fatty acids to the perfusion medium in concentrations that matched those in the circulation in the obese and lean rats exacerbated ischaemic/reperfusion injury in both groups of hearts. The addition of fatty acids to the perfusion medium in these studies doubled the infarct size in both lean and obese hearts when compared to hearts perfused with glucose and insulin alone (du Toit et al., 2008). These observations were further corroborated by studies in which we induced in vivo infarcts in this model of diet induced obesity and observed similar infarct sizes to those documented in the ex vivo working heart model with insulin and fatty acids in the perfusion medium (Clark et al., 2011). Conclusions Obesity with insulin resistance had no effect on cardiac structure or in vivo and ex vivo left ventricular pump function in our rodent model of obesity and MetS. Obesity with insulin resistance however increased myocardial lipid content and decreased myocardial tolerance to ischemia/reperfusion. This reduction in ischaemia/reperfusion tolerance was likely due to compromised RISK pathway function in the obese, insulin resistant rat hearts. 16 Acknowledgements and Disclosures This study was supported by funds from the Griffith University Research Grant scheme and the Griffith Health Institute. No conflicts of interest, financial or otherwise, are declared by the authors. Author contributions Conceived and designed experiments: EFDT, DD. Performed the experiments: IW, KS. DD, EFDT. Analysed the data: DD, EFDT, IW, KS. Interpreted data: EFDT, DD, IW, KS, AB. Prepared the figures and manuscript: EFDT, DD, IW, KS, AB. 17 Table 1. Biometric and metabolic parameters for control (CTRL) and high fat diet fed, obese (OB) rats. CTRL OB Mean ±SEM n Mean ±SEM n p-value 710 ±37 14 857 ±22 12 <0.001 Visceral Fat Weight (g) 42.25 ±7.27 14 80.21 ±3.89 12 <0.001 Visceral Fat (%) 5.85 ±1.95 14 9.13 ±0.41 12 <0.001 Total Cholesterol (mmol/L) 2.86 ±0.19 14 2.89 ±0.11 12 0.872 HDL (mmol/L) 0.68 ±0.04 8 0.62 ±0.06 9 0.411 Triglycerides (mmol/L) 1.51 ±0.02 9 3.11 ±0.42 10 <0.05 Glucose (mmol/L) 7.09 ±0.39 11 6.65 ±0.36 10 0.423 Insulin (µIU/ml) 18.44±2.39 10 31.88±5.06 10 <0.05 5.85±1.0 10 9.43±1.2 10 <0.05 Body Weight (g) HOMA-IR HOMA-IR: Homeostasis Model Assessment for Insulin Resistance 18 Table 2. Echocardiographic data for control (CTRL) and obese (OB) rats after 2, 10 and 22 weeks on the respective diets. Week 2 Week 10 Week 22 CTRL OB CTRL OB CTRL OB n=7 n=7 n=7 n=8 n=9 n=8 LVAWd (mm) 1.9±0.1 1.9±0.1 2.3±0.3 2.2±0.2 1.9±0.1 2.1±0.1 LVAWs (mm) 1.9±0.1 1.9±0.1 2.0±0.1 2.1±0.1 2.0±0.1 2.3±0.1 LVPWd (mm) 3.7±0.2 3.8±0.1 4.1±0.3 3.9±0.2 3.9±0.2 4.1±0.2 LVPWs (mm) 3.2±0.1 3.2±0.1 3.2±0.2 3.3±0.1 3.2±0.2 3.4±0.2 LVMass (mg) 817±29 843±24 1026±55 969±55 957±65 1065±54 EF (%) 79.1±2.4 78.6±1.7 75.3±2.4 74.3±3.0 79.2±1.9 75.7±2.3 FS (%) 50.1±2.4 49.0±1.7 46.0±2.3 47.1±2.2 50.1±1.9 46.6±2.1 HR (BPM) 353.9±50.5 354.4±52.6 400.5±12.4 399.1±12.7 459.1±60.6 403.5±13.5 LVSV (ul) 534.1±98.9 425.6±71.2 403.5±48.8 399±21.0 303.9±30.3 354.1±73.3 LVCO (ml/min) 233.7±48.6 193.8±27.0 161.7±21.2 159.1±9.5 137.6±18.6 141.6±29.2 LVAWd: Left ventricular anterior wall thickness in diastole LVAWs: Left ventricular anterior wall thickness in systole LVPWd: Left ventricular posterior wall thickness in diastole LVPWs: Left ventricular posterior wall thickness in systole LVMASS: Left ventricular mass. EF: Ejection fraction FS: Fractional shortening HR; Heart rate. BPM: Beats per minute LVSV: Left ventricular stroke volume LVCO: Left ventricular cardiac output 19 Figure 1. Pre-ischaemic and reperfusion rate pressure product (RPP) for control and obese rat hearts perfused on the Langendorff perfusion system (* p<0.05, ** p<0.01, *** p<0.001, n=6-7). 20 Figure 2. Myocardial infarct size expressed as a percentage of the area at risk for hearts from control and obese rats (*** p<0.01). Representative images of left ventricular sections from control and obese rat hearts are presented below respective bars. 21 Figure 3A&B. Photomicrographs of myocardial sections stained with Oil Red-O for lipid detection at 20x optical zoom. Panel A is a representative section from control hearts while panel B is a representative section from obese hearts. Red granules in tissue sections represent lipids. The blue structures represent the nuclei bound with Mayer’s Hemotoxylin. (scale bar = 50µm). Figure 3C. Myocardial lipid content in the hearts from control and obese rats demonstrating a 36 fold increase in triglyceride content in obese compared to control hearts (n=6, p<0.001). 22 Figure 4A. Effects of obesity on myocardial total Akt expression in cytosolic and membrane fractions (* p< 0.05, *** p<0.001). Data is normalized to values for control hearts. Representative Western blots are presented below each bar. Data are means ± S.E.M. (n=5). 23 Figure 4B. Effects of obesity on myocardial phospho-Akt expression in cytosolic and membrane fractions (*** p<0.01). Expression data is normalized to values for control hearts. Representative Western blots are presented below each bar. Data are means ± S.E.M. (n=5). 24 Figure 5A. Effects of obesity on myocardial total GSK-3β expression in cytosolic and membrane fractions (* p<0.05, *** p<0.001). Expression data is normalized to values for control hearts. Representative Western blots are presented below each bar. Data are means ± S.E.M. (n=5). 25 Figure 5B. Effects of obesity on myocardial phospho-GSK-3β expression in cytosolic and membrane fractions (* p<0.05). Expression data is normalized to values for control hearts. Representative Western blots are presented below each bar. Data are means ± S.E.M. (n=5). 26 Figure 6. Effects of obesity on myocardial total eNOS expression in membrane fractions (*** p<0.001). Expression data is normalized to values for control hearts. Representative Western blots are presented below each bar. Data are means ± S.E.M. (n=5). 27 References Aasum E, Khalid AM, Gudbrandsen OA, How OJ, Berge RK, Larsen TS (2008). Fenofibrate modulates cardiac and hepatic metabolism and increases ischemic tolerance in diet-induced obese mice. Journal of molecular and cellular cardiology 44(1): 201-209. Abel ED, Litwin SE, Sweeney G (2008). Cardiac remodeling in obesity. Physiological reviews 88(2): 389-419. Agudo-Lopez A, Miguel BG, Fernandez I, Martinez AM (2011). Role of protein kinase C and mitochondrial permeability transition pore in the neuroprotective effect of ceramide in ischemiainduced cell death. FEBS letters 585(1): 99-103. Alpert MA (2001). Obesity cardiomyopathy: pathophysiology and evolution of the clinical syndrome. The American journal of the medical sciences 321(4): 225-236. Avelar E, Cloward TV, Walker JM, Farney RJ, Strong M, Pendleton RC, et al. (2007). Left ventricular hypertrophy in severe obesity: interactions among blood pressure, nocturnal hypoxemia, and body mass. Hypertension 49(1): 34-39. Baron AD (1994). Hemodynamic actions of insulin. The American journal of physiology 267(2 Pt 1): E187-202. Berkalp B, Cesur V, Corapcioglu D, Erol C, Baskal N (1995). Obesity and left ventricular diastolic dysfunction. International journal of cardiology 52(1): 23-26. Bernardo BC, Weeks KL, Pretorius L, McMullen JR (2010). Molecular distinction between physiological and pathological cardiac hypertrophy: experimental findings and therapeutic strategies. Pharmacol Ther 128(1): 191-227. Bertrand L, Horman S, Beauloye C, Vanoverschelde JL (2008). Insulin signalling in the heart. Cardiovascular research 79(2): 238-248. Bouhidel O, Pons S, Souktani R, Zini R, Berdeaux A, Ghaleh B (2008). Myocardial ischemic postconditioning against ischemia-reperfusion is impaired in ob/ob mice. American journal of physiology. Heart and circulatory physiology 295(4): H1580-1586. Buchanan J, Mazumder PK, Hu P, Chakrabarti G, Roberts MW, Yun UJ, et al. (2005). Reduced cardiac efficiency and altered substrate metabolism precedes the onset of hyperglycemia and contractile dysfunction in two mouse models of insulin resistance and obesity. Endocrinology 146(12): 53415349. Carroll JF, Jones AE, Hester RL, Reinhart GA, Cockrell K, Mizelle HL (1997). Reduced cardiac contractile responsiveness to isoproterenol in obese rabbits. Hypertension 30(6): 1376-1381. 28 Carroll JF, Zenebe WJ, Strange TB (2006). Cardiovascular function in a rat model of diet-induced obesity. Hypertension 48(1): 65-72. Chess DJ, Stanley WC (2008). Role of diet and fuel overabundance in the development and progression of heart failure. Cardiovascular research 79(2): 269-278. Chiu SM, Oleinick NL (2001). Dissociation of mitochondrial depolarization from cytochrome c release during apoptosis induced by photodynamic therapy. Br J Cancer 84(8): 1099-1106. Christoffersen C, Bollano E, Lindegaard ML, Bartels ED, Goetze JP, Andersen CB, et al. (2003). Cardiac lipid accumulation associated with diastolic dysfunction in obese mice. Endocrinology 144(8): 34833490. Clark C, Smith W, Lochner A, du Toit EF (2011). The effects of gender and obesity on myocardial tolerance to ischemia. Physiological research / Academia Scientiarum Bohemoslovaca 60(2): 291301. Clavijo LC, Pinto TL, Kuchulakanti PK, Torguson R, Chu WW, Satler LF, et al. (2006). Metabolic syndrome in patients with acute myocardial infarction is associated with increased infarct size and in-hospital complications. Cardiovascular revascularization medicine : including molecular interventions 7(1): 7-11. Dhanasekaran A, Gruenloh SK, Buonaccorsi JN, Zhang R, Gross GJ, Falck JR, et al. (2008). Multiple antiapoptotic targets of the PI3K/Akt survival pathway are activated by epoxyeicosatrienoic acids to protect cardiomyocytes from hypoxia/anoxia. American journal of physiology. Heart and circulatory physiology 294(2): H724-735. Dong F, Zhang X, Yang X, Esberg LB, Yang H, Zhang Z, et al. (2006). Impaired cardiac contractile function in ventricular myocytes from leptin-deficient ob/ob obese mice. The Journal of endocrinology 188(1): 25-36. Downey JM, Davis AM, Cohen MV (2007). Signaling pathways in ischemic preconditioning. Heart failure reviews 12(3-4): 181-188. du Toit EF, Nabben M, Lochner A (2005). A potential role for angiotensin II in obesity induced cardiac hypertrophy and ischaemic/reperfusion injury. Basic research in cardiology 100(4): 346-354. du Toit EF, Smith W, Muller C, Strijdom H, Stouthammer B, Woodiwiss AJ, et al. (2008). Myocardial susceptibility to ischemic-reperfusion injury in a prediabetic model of dietary-induced obesity. American journal of physiology. Heart and circulatory physiology 294(5): H2336-2343. 29 Eckel RH, Grundy SM, Zimmet PZ (2005). The metabolic syndrome. The Lancet 365(9468): 14151428. Essop MF, Anna Chan WY, Valle A, Garcia-Palmer FJ, Du Toit EF (2009). Impaired contractile function and mitochondrial respiratory capacity in response to oxygen deprivation in a rat model of prediabetes. Acta Physiol (Oxf) 197(4): 289-296. Ferrannini E, Santoro D, Bonadonna R, Natali A, Parodi O, Camici PG (1993). Metabolic and hemodynamic effects of insulin on human hearts. The American journal of physiology 264(2 Pt 1): E308-315. Foppa M, Duncan BB, Rohde LE (2005). Echocardiography-based left ventricular mass estimation. How should we define hypertrophy? Cardiovascular ultrasound 3: 17. Gustafsson AB, Gottlieb RA (2007). Bcl-2 family members and apoptosis, taken to heart. American journal of physiology. Cell physiology 292(1): C45-51. Halestrap AP, Clarke SJ, Khaliulin I (2007). The role of mitochondria in protection of the heart by preconditioning. Biochimica et biophysica acta 1767(8): 1007-1031. Hausenloy DJ, Yellon DM (2009). Preconditioning and postconditioning: underlying mechanisms and clinical application. Atherosclerosis 204(2): 334-341. Kannel WB, Dawber TR, Kagan A, Revotskie N, Stokes J, 3rd (1961). Factors of risk in the development of coronary heart disease--six year follow-up experience. The Framingham Study. Annals of internal medicine 55: 33-50. Kannel WB, Dawber TR, Thomas HE, Jr., McNamara PM (1965). Comparison of Serum Lipids in the Prediction of Coronary Heart Disease. Framingham Study Indicates That Cholesterol Level and Blood Pressure Are Major Factors in Coronary Heart Disease; Effect of Obesity and Cigarette Smoking Also Noted. Rhode Island medical journal 48: 243-250. Kantor PF, Dyck JR, Lopaschuk GD (1999). Fatty acid oxidation in the reperfused ischemic heart. The American journal of the medical sciences 318(1): 3-14. Katakam PV, Jordan JE, Snipes JA, Tulbert CD, Miller AW, Busija DW (2007). Myocardial preconditioning against ischemia-reperfusion injury is abolished in Zucker obese rats with insulin resistance. American journal of physiology. Regulatory, integrative and comparative physiology 292(2): R920-926. Kenchaiah S, Evans JC, Levy D, Wilson PW, Benjamin EJ, Larson MG, et al. (2002). Obesity and the risk of heart failure. N Engl J Med 347(5): 305-313. 30 Kloner RA, Forman MB, Gibbons RJ, Ross AM, Alexander RW, Stone GW (2006). Impact of time to therapy and reperfusion modality on the efficacy of adenosine in acute myocardial infarction: the AMISTAD-2 trial. European heart journal 27(20): 2400-2405. Lee Y, Naseem RH, Park BH, Garry DJ, Rishardson JA, Shaffer JE, et al. (2006). α-Lipoic acid prevents lipotoxic cardiomyopathy in acyl-CoA synthase transgenic mice. Biochem Biophys Res 344: 446-452. Liedtke AJ, DeMaison L, Eggleston AM, Cohen LM, Nellis SH (1988). Changes in substrate metabolism and effects of excess fatty acids in reperfused myocardium. Circulation research 62(3): 535-542. Lopaschuk GD, Folmes CD, Stanley WC (2007). Cardiac energy metabolism in obesity. Circulation research 101(4): 335-347. Lu MC, Tzang BS, Kuo WW, Wu FL, Chen YS, Tsai CH, et al. (2007). More activated cardiac mitochondrial-dependent apoptotic pathway in obese Zucker rats. Obesity 15(11): 2634-2642. Maarman G, Marais E, Lochner A, du Toit EF (2012). Effect of chronic CPT-1 inhibition on myocardial ischemia-reperfusion injury (I/R) in a model of diet-induced obesity. Cardiovasc Drugs Ther 26(3): 205-216. Majane OH, Vengethasamy L, du Toit EF, Makaula S, Woodiwiss AJ, Norton GR (2009). Dietaryinduced obesity hastens the progression from concentric cardiac hypertrophy to pump dysfunction in spontaneously hypertensive rats. Hypertension 54(6): 1376-1383. Mazumder PK, O'Neill BT, Roberts MW, Buchanan J, Yun UJ, Cooksey RC, et al. (2004). Impaired cardiac efficiency and increased fatty acid oxidation in insulin-resistant ob/ob mouse hearts. Diabetes 53(9): 2366-2374. Millis RM, Alvin ZV, Zhao A, Haddad GE (2012). Effects of IGF-1 on I(K) and I(K1) Channels via PI3K/Akt Signaling in Neonatal Cardiac Myocytes. International journal of cell biology 2012: 712153. Nduhirabandi F, Du Toit EF, Blackhurst D, Marais D, Lochner A (2011). Chronic melatonin consumption prevents obesity-related metabolic abnormalities and protects the heart against myocardial ischemia and reperfusion injury in a prediabetic model of diet-induced obesity. Journal of pineal research 50(2): 171-182. Nduhirabandi F, du Toit EF, Lochner A (2012). Melatonin and the metabolic syndrome: a tool for effective therapy in obesity-associated abnormalities? Acta Physiol (Oxf) 205(2): 209-223. Nikolaidis LA, Mankad S, Sokos GG, Miske G, Shah A, Elahi D, et al. (2004). Effects of glucagon-like peptide-1 in patients with acute myocardial infarction and left ventricular dysfunction after successful reperfusion. Circulation 109(8): 962-965. 31 Ninomiya JK, L'Italien G, Criqui MH, Whyte JL, Gamst A, Chen RS (2004). Association of the metabolic syndrome with history of myocardial infarction and stroke in the Third National Health and Nutrition Examination Survey. Circulation 109(1): 42-46. Nishida K, Otsu K (2008). Cell death in heart failure. Circulation journal : official journal of the Japanese Circulation Society 72 Suppl A: A17-21. Norton GR, Majane OH, Libhaber E, Maseko MJ, Makaula S, Libhaber C, et al. (2009). The relationship between blood pressure and left ventricular mass index depends on an excess adiposity. Journal of hypertension 27(9): 1873-1883. Ouwens DM, Diamant M, Fodor M, Habets DD, Pelsers MM, El Hasnaoui M, et al. (2007). Cardiac contractile dysfunction in insulin-resistant rats fed a high-fat diet is associated with elevated CD36mediated fatty acid uptake and esterification. Diabetologia 50(9): 1938-1948. Pascual M, Pascual DA, Soria F, Vicente T, Hernandez AM, Tebar FJ, et al. (2003). Effects of isolated obesity on systolic and diastolic left ventricular function. Heart 89(10): 1152-1156. Peterson LR, Herrero P, Schechtman KB, Racette SB, Waggoner AD, Kisrieva-Ware Z, et al. (2004). Effect of obesity and insulin resistance on myocardial substrate metabolism and efficiency in young women. Circulation 109(18): 2191-2196. Piot C, Croisille P, Staat P, Thibault H, Rioufol G, Mewton N, et al. (2008). Effect of cyclosporine on reperfusion injury in acute myocardial infarction. N Engl J Med 359(5): 473-481. Polidori C, Bartels ED, Nielsen JM, Hellgren LI, Ploug T, Nielsen LB (2009). Cardiac Expression of Microsomal Triglyceride Transfer Protein Is Increased in Obesity and Serves to Attenuate Cardiac Triglyceride Accumulation. PLoS ONE 4(4): e5300. Santos CX, Anilkumar N, Zhang M, Brewer AC, Shah AM (2011). Redox signaling in cardiac myocytes. Free radical biology & medicine 50(7): 777-793. Scaglione R, Dichiara MA, Indovina A, Lipari R, Ganguzza A, Parrinello G, et al. (1992). Left ventricular diastolic and systolic function in normotensive obese subjects: influence of degree and duration of obesity. European heart journal 13(6): 738-742. Stegemann H, Stalder K (1967). Determination of hydroxyproline. Clinica chimica acta; international journal of clinical chemistry 18(2): 267-273. Stoddard MF, Tseuda K, Thomas M, Dillon S, Kupersmith J (1992). The influence of obesity on left ventricular filling and systolic function. American heart journal 124(3): 694-699. 32 Turinsky J, O'Sullivan DM, Bayly BP (1990). 1,2-Diacylglycerol and ceramide levels in insulin-resistant tissues of the rat in vivo. J Biol Chem 265(28): 16880-16885. Vasanji Z, Cantor EJ, Juric D, Moyen M, Netticadan T (2006). Alterations in cardiac contractile performance and sarcoplasmic reticulum function in sucrose-fed rats is associated with insulin resistance. American journal of physiology. Cell physiology 291(4): C772-780. Wagner C, Kloeting I, Strasser RH, Weinbrenner C (2008). Cardioprotection by postconditioning is lost in WOKW rats with metabolic syndrome: role of glycogen synthase kinase 3beta. Journal of cardiovascular pharmacology 52(5): 430-437. Wang J, Sarnola K, Ruotsalainen S, Moilanen L, Lepisto P, Laakso M, et al. (2010). The metabolic syndrome predicts incident congestive heart failure: a 20-year follow-up study of elderly Finns. Atherosclerosis 210(1): 237-242. Wilson CR, Tran MK, Salazar KL, Young ME, Taegtmeyer H (2007). Western diet, but not high fat diet, causes derangements of fatty acid metabolism and contractile dysfunction in the heart of Wistar rats. The Biochemical journal 406(3): 457-467. Wold LE, Dutta K, Mason MM, Ren J, Cala SE, Schwanke ML, et al. (2005). Impaired SERCA function contributes to cardiomyocyte dysfunction in insulin resistant rats. Journal of molecular and cellular cardiology 39(2): 297-307. Wong CY, O'Moore-Sullivan T, Leano R, Hukins C, Jenkins C, Marwick TH (2006). Association of subclinical right ventricular dysfunction with obesity. Journal of the American College of Cardiology 47(3): 611-616. Young LH (2010). Diet-induced obesity obstructs insulin signaling in the heart. American journal of physiology. Heart and circulatory physiology 298(2): H306-307. Yu C, Chen Y, Cline GW, Zhang D, Zong H, Wang Y, et al. (2002). Mechanism by which fatty acids inhibit insulin activation of insulin receptor substrate-1 (IRS-1)-associated phosphatidylinositol 3kinase activity in muscle. J Biol Chem 277(52): 50230-50236. Zarich SW, Kowalchuk GJ, McGuire MP, Benotti PN, Mascioli EA, Nesto RW (1991). Left ventricular filling abnormalities in asymptomatic morbid obesity. The American journal of cardiology 68(4): 377381. Zhang L, Keung W, Samokhvalov V, Wang W, Lopaschuk GD (2010). Role of fatty acid uptake and fatty acid beta-oxidation in mediating insulin resistance in heart and skeletal muscle. Biochimica et biophysica acta 1801(1): 1-22. 33