* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiovascular System
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
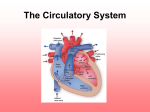
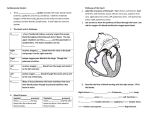
Cardiovascular System THE HEART AND CIRCULATORY SYSTEM Heart Anatomy Size: approximately the size of a person’s fist Left side of thoracic cavity Coverings: Pericardium Double layered sac Contains 10 – 20 cc. Of pericardial fluid to reduce the friction of the beating heart Heart Wall Myocardium: heart muscle; thicker on left side of the heart Chambers Atria (L & R Atrium) 2 upper chambers of heart Thin walls, smooth inner surface Foramen ovale: passageway between the 2 atria so that the lungs are bypassed in the developing fetus Cont. (Atrium) Fossa ovale: scar tissue where the foramen ovale existed until it closed up shortly after birth Responsible for receiving blood Ventricles Thicker walls, irregular inner surface Contain chordae tendineae (prevent heart valves from turning inside out when ventricles contract) Left wall 3 times as thick as right wall; forms apex of heart Responsible for pumping blood away from the heart Accessory Structures Septum: muscular wall dividing the heart into right and left halves Heart valves – prevents the backflow of blood Great Vessels Superior and inferior vena cava: receive deoxygenated blood from all parts of the body Pulmonary arteries: carry deoxygenated blood to the lungs from the right ventricle Pulmonary veins: carry oxygenated blood to the left atrium from the lungs Aorta: carries oxygenated blood to distribute to all parts of the body Pathway of Blood Through the Heart and All Body Tissues 1. Superior and inferior vena cava 2. Right atrium 3. Tricuspid valve 4. Right ventricle 5. Pulmonary semilunar valve Continue pathway 6. Pulmonary arteries 7. Lungs ( O2 and CO2 exchange = external respiration) 8. Pulmonary veins 9. Left atrium 10. Bicuspid/Mitral valve Continue pathway 11. Left ventricle 12. Aortic semilunar valve 13. Aorta - all parts of body via arteries Cont. pathway 14. Arterioles 15. Capillaries of individual tissues (O2 and CO2 exchange = internal respiration) 16. Venules 17. Veins 18. Superior and inferior vena cava Cardiovascular Circuits Pulmonary circuit: transport of blood from the right side of the heart to the lungs and then back to the left side of the heart Systemic circuit: transport of blood from the left side of the heart to all parts of the body and then back to the right side of the heart Coronary circuit: transport blood from the left side of the heart to the heart tissues and back to the right side of the heart Valves Tough fibrous tissue between the heart chambers and major blood vessels of the heart Gate-like structures to keep the blood flowing in one direction and to prevent regurgitation or backflow of blood Atrioventricular valves: when ventricles contract, blood is forced upward and the valves close; attached by papillary muscles and chordae tendineae Tricuspid valve: between the right atrium and the right ventricle Bicuspid/mitral valve: between the left atrium and the left ventricle continue Valves Semilunar Valves: 3 half moon pockets that catch blood and balloon out to close the opening Pulmonary semilunar valve: between the right ventricle and the pulmonary arteries Aortic semilunar valve: between the left ventricle and the aortic arch/aorta 5. Heart Sounds When the AV (atrioventricular) and semilunar valves close, they make the sound heard as “lubdub” (auscultated with stethoscope) Cardiac Circulation (Blood Supply to the Heart) 1. Aorta - coronary arteries - capillaries in myocardium coronary veins - coronary sinus - right atrium 2. Blood in chambers nourishes endocardium 3. Coronary circuit open ONLY during relaxation phase of cardiac cycle 4. Occlusion of coronary artery - myocardial infarction (heart attack) if collateral circulation is inadequate Heart Physiology Nerve Supply to Heart Alters rate and force of cardiac contraction Vagus nerve (parasympathetic nervous system): slows heart rate Sympathetic nerves: increase heart rate Epinephrine/Norepinephrine: increase heart rate Nerve supply to heart Sensory (afferent) nerves: detect atria being stretched and lack of oxygen (changes rate of contractions) Angina: chest pain due to lack of oxygen in coronary circulation Automaticity Enables heart to contract rhythmically and continuously without motor nerve impulses SA (sinoatrial) node: pacemaker located where the superior and inferior vena cava enter the right atrium ▪ http://www.argosymedical.com/Circulatory/samples/ani mations/Heart%20Conduction%20System/index.html AV (Atrioventricular) node: sends impulses to ventricles Purkinje fibers: in heart wall to distribute nerve impulses Overview of Blood Vessels Arteries ALWAYS Carry blood AWAY from the heart All BUT pulmonary arteries carry oxygenated blood Aorta: largest artery; 1 inch in diameter Arterioles: smallest arteries Arteries Coronary arteries: most important; supply blood to the heart muscle Veins Carry blood TOWARD the heart All BUT pulmonary veins carry deoxygenated blood Layers much thinner, less elastic Series of internal valves that work against the flow of gravity to prevent reflux Superior and inferior vena cava: largest veins Venules: smallest veins Capillaries Tiny, microscopic vessels Walls one cell layer thick Function: to transport and diffuse essential materials to and from the body’s cells and the blood Blood Pressure Blood Pressure Systole: maximum pressure formed during a ventricular contraction Diastole: minimum pressure during ventricular relaxation (atrial contraction) Blood Pressure Normals Systolic = 100 – 140 Diastolic = 60 – 90 Hypotension: Systolic < 90 Hypertension: Systolic > 150 and/or Diastolic > 90 Blood Pressure Factors Affecting BP Cardiac output Peripheral resistance Blood volume Diseases of the Cardiovascular System 1. Arteriosclerosis 2. Atherosclerosis 3. Hypertension 4. Ischemic Heart Disease http://www.argosymedical.com/Circulatory/samples/anim ations/Myocardial%20Damage/index.html 5. Cardiac Arrhythmias 6. Bacterial Endocarditis 7. Valvular Heart Disease 8. Congenital Heart Disease 9. Congestive Heart Failure (CHF) http://www.argosymedical.com/Circulatory/samples/anim ations/Congestive%20Heart%20Failure/index.html Blood Functions of blood Transportation 1. Blood carries oxygen and nutrients from digestive and respiratory systems and delivers them to each cell. 2. Blood carries waste products from cells to excretory organs. a. Carbon dioxide from cells to lungs b. Other waste products of metabolism to kidneys Defense against disease 1. White blood cells combat bacterial invasion 2. Antibodies Components of Blood Plasma – liquid part of blood. May contain digested food, metabolic wastes, carbon dioxide, oxygen, hormones or enzymes. Formed elements - ….. Formed Elements ▪ Red blood cells (erythrocytes) Contain hemoglobin (from red bone marrow) Transport Oxygen from lungs to cells and C02 from cells to lungs ▪ White blood cells (leukocytes) formed in bone marrow or lymph tissue destroy invading bacteria ▪ Platelets (thrombocytes) tiny fragments of bone marrow cells; required for clotting of blood Blood Types ▪ The population is divided into four blood groups called A, B, AB or O. The types are distinguished by the presence or absence of specific proteins on the surface of the red blood cells or in the blood serum. ▪ Blood type is important in transfusion Antigen and Antibody Antigens Antibodies ▪ There are two antigens, A and B. If you have the A antigen on the RBC, then you have type A blood. When B antigen is present, you have type B blood. When both A and B antigens are present, you have type AB blood. When neither are present, you have type O blood. ▪ When an antigen is present on the RBC, then the opposite antibody present in the plasma. For instance, type A blood has anti-type-B antibodies. Type B blood has anti-type-A antibodies. Type AB blood has no antibodies in the plasma, and type O blood has both anti-type-A and anti-type-B antibodies in the plasma. These antibodies are not present at birth but are formed spontaneously during infancy and last throughout life. ▪ Type A would have B agglutinins (antibody) in the plasma. ▪ Type B would have A agglutinins (antibody) in the plasma. ▪ Type AB would not have agglutinins (antibody) in the plasma. ▪ Type O would have A and B agglutinins (antibody) in the plasma. ▪ Universal Donor ▪ Group O ▪ Carries no A or B antigens ▪ Packed and processed units have little antibody ▪ Universal Recipient ▪ Group AB ▪ ▪ ▪ ▪ Patient has no anti-A or anti-B present Cannot lyse any transfused cells Beware: other antibodies may be present Average Percents ▪ Type O—46% ▪ Type A—40% ▪ Type B—10% ▪ Type AB—4% A B O Blood Type Calculator ▪ http://www.biology.arizona.edu/human_bio/pro blem_sets/blood_types/btcalcA_popup.html ▪ http://www.biology.arizona.edu/human_bio/pro blem_sets/blood_types/inherited.html#calculato r inheritance Rh factor ▪ First found in the Rhesus Monkey ▪ The Rh factor is another protein factor in red blood cells, separate from A, B, O proteins. ▪ Rh positive blood means the Rh factor (protein) is present in the red blood cells. (85% of the U.S. population is Rh positive). ▪ Rh negative blood means no Rh antigen is present in red blood cells. ▪ The Rh factor is important in transfusion and pregnancy. Percentage population ▪ Population Caucasian Rh(D) pos Rh(D) neg 86% 14% African-American 95% 5% Oriental <1% >99% Pregnancy and blood type ▪ Father--Rh+ blood ▪ Mother is Rh– ▪ Child could be Rh +. ▪ 1st pregnancy--if the baby is rh +, then there are no complications. ▪ However, the mother will start to develop antibodies against the Rh factor Pregnancy ▪ Second pregnancy, if the child is +, the mother’s antibodies can cross the placenta and start to attack the fetus’ blood cells, causing hemolysis. ▪ Hemolysis--breakdown of RBC and the release of hemoglobin into the plasma which can damage organs. ▪ This is called erythroblastosis fetalis,can cause severe anemia, jaundice possibly death. Inheritance ▪ ABO & RH genes are not linked ▪ ABO & Rh(D) type are inherited independently For example: An A Rh(D) pos mother and a B Rh(D) pos father could have an O Rh(D) neg child ▪ http://www.biology.arizona.edu/human_bio/pro blem_sets/blood_types/rh_factor.html Blood humor