* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Urinary Physiology Urine Formation Urine Formation Glomerular
Electrophysiology wikipedia , lookup
Cardiac output wikipedia , lookup
Intracranial pressure wikipedia , lookup
Stimulus (physiology) wikipedia , lookup
Renal function wikipedia , lookup
Countercurrent exchange wikipedia , lookup
Circulatory system wikipedia , lookup
Haemodynamic response wikipedia , lookup
Biofluid dynamics wikipedia , lookup
Hemodynamics wikipedia , lookup
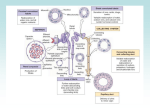
4/24/2016 Urine Formation • Filtrate – Blood plasma minus most proteins Urinary Physiology Urinary Section pages 9-17 • Urine – <1% of total filtrate – Contains metabolic wastes and unneeded substances Urine Formation Afferent arteriole Glomerular capillaries Efferent arteriole 1. Glomerular filtration 2. Tubular reabsorption Cortical radiate artery Glomerular capsule Returns components to blood Rest of renal tubule containing filtrate Glucose, amino acids, water and salt 3. Tubular secretion Reverse of reabsorption Selective addition to urine 4. Water conservation Peritubular capillary Three major renal processes: Glomerular filtration Tubular reabsorption Tubular secretion To cortical radiate vein Urine Figure 25.10 Glomerular Filtration Occurs at renal corpuscle Passive process driven by hydrostatic pressure Glomerulus is a very efficient filter Permeable membrane Water and small solutes pushed through filter Large surface area Higher blood pressure Efferent arteriole Glomerular capsular space Proximal convoluted tubule Afferent arteriole Glomerular capillary covered by podocytecontaining visceral layer of glomerular capsule Cytoplasmic extensions of podocytes Filtration slits Parietal layer of glomerular capsule (a) Glomerular capillaries and the visceral layer of the glomerular capsule Podocyte cell body Fenestrations (pores) Glomerular capillary endothelium (podocyte covering and basement membrane removed) Foot processes of podocyte Figure 25.9a 1 4/24/2016 Glomerular Filtration Filtration membrane • Capillary endothelium • Basement membrane • Foot processes of podocyte of glomerular capsule Capillary • Filtration membrane – 3 components • Fenestrated capillary endothelium • Basement membrane • Podocytes – Allows passage of water and small solutes • Fenestrations prevent filtration of blood cells • Negatively charged basement membrane repels large anions Plasma Fenestration (pore) Filtration slits Filtrate in capsular space Filtration slit Slit diaphragm Foot processes of podocyte (c) Three parts of the filtration membrane Glomerular Filtration Podocyte cell body Foot processes • Net Filtration Pressure (NFP) – Glomerular hydrostatic pressure (HPg) – Capsular hydrostatic pressure (HPc) – Blood osmotic pressure (OPg) (b) Filtration slits between the podocyte foot processes Glomerular Filtration Afferent arteriole Glomerular capsule • Net Filtration Pressure (NFP) – The pressure responsible for filtrate formation NFP = HPg – (OPg + HPc) 10 mm Hg Net filtration pressure Glomerular (blood) hydrostatic pressure (HPg = 55 mm Hg) Blood colloid osmotic pressure (Opg = 30 mm Hg) Capsular hydrostatic pressure (HPc = 15 mm Hg) Figure 25.11 2 4/24/2016 Net Filtration Pressure Glomerular Filtration • Glomerular Filtration Rate (GFR) NFP = HPG – (OPG + HPC) = 55 mm Hg – (30 mmHg + 15 mmHg) = 10 mmHg Glomerular Filtration • Factors affecting GFR – Kidney disease • ↓ blood osmo>c pressure, ↑ capsular osmo>c pressure – Hemorrhage • ↓ glomerular blood hydrostatic pressure – Hypotension • Glomerular blood hydrostatic pressure = capsule hydrostatic and blood osmotic pressure = filtration stops! – 125 ml/min 1800 liters of blood through kidneys/day = 1200 ml/min = about 180 liters filtrate/day Glomerular Filtration • GFR is tightly controlled by two types of mechanisms – Intrinsic control (renal autoregulation) • Act locally within the kidney – Extrinsic controls • Nervous and endocrine mechanisms that maintain blood pressure and affect kidneys – Termed renal suppression Intrinsic Control • Goal = Maintain a nearly constant GFR when MAP is in the range of 80–180 mm Hg – Renal autoregulation • Mechanisms that cause vasoconstriction of afferent arterioles in response to increased BP • Reduces glomerular flow to keep GFR the same Extrinsic Controls • Sympathetic nervous system – At rest • Renal blood vessels are dilated • Renal autoregulation mechanisms prevail • GFR maintained – Extreme stress • Norepinephrine and epinephrine released • Both cause constriction of afferent arterioles – Inhibits filtration – Shunts blood to other vital organs 3 4/24/2016 Tubular Reabsorption • • • • • 125 ml/min of filtrate produced Most of this fluid is reabsorbed A selective transepithelial process Includes active and passive process Most occurs in PCT Tubular Reabsorption • Transcellular route Luminal membranes of tubule cells Cytosol of tubule cells Basolateral membranes of tubule cells Tubular Reabsorption • PCT – Site of most reabsorption • • • • 65% of Na+ and water All nutrients Ions Small proteins Movement via the transcellular route involves: 1 Transport across the luminal membrane. 2 Diffusion through the cytosol. Lateral intercellular space Tight junction Filtrate in tubule lumen The paracellular route involves: • Movement through leaky tight junctions, particularly in the PCT. 3 Transport across the basolateral membrane. (Often involves the lateral intercellular spaces because membrane transporters transport ions into these spaces.) 4 Movement through the interstitial fluid and into the capillary. Interstitial fluid Capillary endothelial cell Tubule cell Peritubular capillary Paracellular H2O 2 1 3 4 Transcellular Luminal membrane 1 Transcellular 3 4 2 Solutes 3 4 Endothelium of peritubular capillaries Paracellular Basolateral membranes Active transport Passive transport Figure 25.13 Tubular Reabsorption • Paracellular route – Between cells – Limited to water movement and reabsorption of Ca2+, Mg2+, K+, and some Na+ in the PCT where tight junctions are leaky Tubular Reabsorption • Sodium – Most abundant cation in filtrate – Primary active transport out of the tubule cell by Na+-K+ ATPase in the basolateral membrane – Na+ passes in through the luminal membrane by secondary active transport or facilitated diffusion mechanisms 4 4/24/2016 Tubular Reabsorption 1 At the basolateral membrane, Na+ Nucleus Filtrate in tubule lumen Na+ Interstitial fluid Tubule cell 2 3Na+ 3Na+ Glucose Amino acids Some ions Vitamins H2O Lipid-soluble substances Cl–, Ca2+, K+ and other ions, urea 1 2K+ 2K+ 3 K+ 4 5 6 Primary active transport Secondary active transport Passive transport (diffusion) Tight junction Cl– Paracellular route Peritubular capillary is pumped into the interstitial space by the Na+-K+ ATPase. Active Na+ transport creates concentration gradients that drive: 2 “Downhill” Na+ entry at the luminal membrane. 3 Reabsorption of organic nutrients and certain ions by cotransport at the luminal membrane. 4 Reabsorption of water by osmosis. Water reabsorption increases the concentration of the solutes that are left behind. These solutes can then be reabsorbed as they move down their concentration gradients: 5 Lipid-soluble substances diffuse by the transcellular route. Transport protein Ion channel or aquaporin • Sodium – Low hydrostatic pressure and high osmotic pressure in the peritubular capillaries • Promotes bulk flow of water and solutes (including Na+) 6 Cl– (and other anions), K+, and urea diffuse by the paracellular route. Figure 25.14 Tubular Maximum – Transport maximum (Tm) reflects the number of carriers in the renal tubules available – When the carriers are saturated, excess of that substance is excreted – Example: too much glucose in the blood entering glomerulus will cause glucosuria Tubular Reabsorption • Reabsorption of nutrients, water and ions – Blood becomes hypertonic to filtrate – Water is reabsorbed by osmosis – Cations and fat-soluble substances follow by diffusion Tubular Secretion • Reabsorption in reverse – K+, H+, NH4+, creatinine and organic acids move from peritubular capillaries or tubule cells into filtrate – Involves active transport since no concentration gradients in this case 5 4/24/2016 Na+ (65%) Glucose Amino acids H2O (65%) and many ions (e.g. Cl– and K+) Milliosmols Tubular Secretion Cortex (d) (a) 300 (e) Outer medulla (b) 600 Some drugs – H+, HCO3 NH4+ • Foreign substances (penicillin and other drugs) • Nitrogenous wastes • Excess K+ Inner medulla Blood pH regulation (a) Proximal convoluted tubule: • 65% of filtrate volume reabsorbed • Na+, glucose, amino acids, and other nutrients actively transported; H2O and many ions follow passively • H+ and NH4+ secretion and HCO3– reabsorption to maintain blood pH (see Chapter 26) • Some drugs are secreted • Principle effects – Rids body of (c) – Controls blood pH: 1200 • Altering amounts of H+ or HCO3– in urine Active transport (primary or secondary) Passive transport Figure 25.18a Variations in Urine Formation • Composition varies – Fluid volume – Solute concentration Variations in Urine Formation • Water intake must equal water loss – Kidney regulates water loss by producing: • Hypotonic urine (dilute) • Hypertonic urine (concentrated) Osmolality of interstitial fluid (mOsm) Countercurrent Mechanism • Role of countercurrent mechanisms – Establish and maintain an osmotic gradient – Creates hypertonic interstitial fluid within kidney medulla – Hypertonic interstitial fluid allows the kidneys to vary urine concentration Active transport H2O NaCI H2O NaCI H2O NaCI H2O NaCI Cortex Passive transport Water impermeable Countercurrent multiplier The long loops of Henle of the juxtamedullary nephrons create the medullary osmotic gradient. Outer medulla H2O NaCI H2O H2O Inner medulla Loop of Henle Figure 25.16a 6 4/24/2016 Active transport Passive transport Formation of Concentrated Urine Collecting duct H2O Descending limb of loop of Henle • Depends on the medullary osmotic gradient and the ability to alter permeability of the collecting tubules DCT H2O Cortex H2O NaCI H2O osmolarity of extracellular fluid (also plasma volume) H2O NaCI Outer medulla ADH release H2O Urea NaCI aquaporins in collecting duct H2O Urea H2O Inner medulla H2O reabsorption in collecting duct H2O (b) Maximal ADH Small volume of concentrated urine Small volume of concentrated urine Figure 25.17b Active transport Passive transport Formation of Dilute Urine Collecting duct • Filtrate is diluted in the ascending Loop of Henle • In the absence of ADH, dilute filtrate continues into the renal pelvis as dilute urine Descending limb of loop of Henle DCT Cortex NaCI osmolarity of extracellular fluid H2O ADH release NaCI Outer medulla NaCI aquaporins in collecting duct H2O reabsorption in collecting duct H2O Urea Inner medulla (a) Absence of ADH Large volume of dilute urine Large volume of dilute urine Acid-Base Balance • pH affects all functional proteins and biochemical reactions in the body – Regulation prevents changes in body’s internal environment • Alkalosis or alkalemia: arterial blood pH >7.45 • Acidosis or acidemia: arterial pH < 7.35 Figure 25.17a Acid-Base Balance • Concentration of hydrogen ions is regulated by 1. Chemical buffer systems in blood • Rapid, first line of defense 2. Brainstem respiratory centers • Acts within 1–3 minutes 3. Renal mechanisms • Most potent • Requires hours to days to affect pH changes 7 4/24/2016 Acid-Base Balance Acid-Base Balance • Most important renal mechanisms: – Blood – Conserving (reabsorbing) HCO3– – Excreting HCO3– – Secretion of H+ • CO2 + H2O ↔ H2CO3 ↔ HCO3- + H+ – Lungs • Regulate carbonic acid levels by CO2 manipulation • H+ secretion occurs in the PCT and in collecting tubules – Kidneys • Selectively secrete and reabsorb to maintain pH Acid-Base Balance • Examples – Respiratory Acidosis • Lungs are unable to eliminate CO2 adequately • Kidneys reabsorb HCO3–, secrete H + (and NH4 +) – Respiratory Alkalosis • CO2 levels are low • Kidneys secrete HCO3–, retain H + (and NH4 +) 1 CO2 combines with water within the tubule cell, forming H2CO3. 3bFor each H+ secreted, a HCO3– enters the peritubular capillary blood either via symport with Na+ or via antiport with CI–. 2 H2CO3 is quickly split, forming H+ and bicarbonate ion (HCO3–). 4 Secreted H+ combines with HCO3– in the filtrate, forming carbonic acid (H2CO3). HCO3– disappears from the filtrate at the same rate that HCO3– (formed within the tubule cell) enters the peritubular capillary blood. 3aH+ is secreted into the filtrate. Nucleus Filtrate in tubule lumen Peritubular capillary PCT cell 2K+ 2K+ ATPase 3Na+ HCO3– + Na+ 3Na+ Cl– Cl– HCO3– 3a H+ HCO3– 4 H+ * 5 HCO3– 2 ATPase H2CO3 3b HCO3– H2CO3 1 Na+ CO2 6 CO2 diffuses into the tubule cell, where it triggers further H+ secretion. Na+ CA 6 H2O 5 The H2CO3 formed in the filtrate dissociates to release CO2 and H2O. CO2 + H2O CO2 Tight junction Primary active transport Secondary active transport Simple diffusion Transport protein Carbonic anhydrase Figure 26.12 Variations in Blood Pressure Variations in Blood Pressure • Activity of kidney related to variations in blood pressure • Renal mechanisms influencing blood pressure – Blood pressure and blood volume are related – Blood volume is controlled by • Solute concentration • Water regulation – ADH • Water – Renin-angiotensin mechanism • Sodium • Potassium 8 4/24/2016 Antidiuretic Hormone (ADH) Aldosterone • Produced in adrenal cortex in response to… • Plasma osmolarity – Low blood volume – Low blood pressure – Low plasma Na + – High plasma K + Increases (what could cause this?) Osmoreceptors stimulated Thirst & ADH secretion • Stimulates K+ secretion and Na+ reabsorption • Changes in plasma sodium levels affect… Water reabsorption (decreased urine output) Increased blood volume – Plasma volume – Blood pressure Increased blood pressure Aldosterone Aldosterone • Regulation of sodium balance • Renin-angiotensin mechanism is the main trigger for aldosterone release – Na+ reabsorption • 65% is reabsorbed in the proximal tubules • 25% is reclaimed in the Loops of Henle – Granular cells of JGA secrete renin in response to • Sympathetic nervous system stimulation • ↓ Filtrate osmolality (decreased sodium) • ↓ Stretch (due to ↓ blood pressure) – Aldosterone causes active reabsorption of remaining Na+ in DCT and collecting ducts – Water follows Na+ – How would this affect blood volume and blood pressure? Efferent arteriole Glomerular capsule Glomerulus Afferent arteriole Parietal layer of glomerular capsule Capsular space Aldosterone Foot processes of podocytes Red blood cell Proximal tubule cell Efferent arteriole Juxtaglomerular apparatus • Macula densa cells of the ascending limb of loop of Henle • Extraglomerular mesangial cells • Granular cells Lumens of glomerular capillaries Endothelial cell of glomerular capillary Mesangial cells between capillaries Afferent arteriole Juxtaglomerular apparatus Podocyte cell body (visceral layer) • Renin catalyzes the production of angiotensin II – Prompts aldosterone release from the adrenal cortex • Targets cells of DCT and collecting ducts • Initiates sodium reabsorption – Causes systemic vasoconstriction – Effect on BP? Renal corpuscle Figure 25.8 9 4/24/2016 K+ (or Na+) concentration in blood plasma* Blood Pressure Control Renin-angiotensin mechanism Stimulates • 3 main mechanisms Adrenal cortex Negative feedback inhibits – Renin-angiotensin system – Neural regulation (sympathetic control) – ADH release Releases Aldosterone Targets Kidney tubules Effects Na+ reabsorption K+ secretion Restores Homeostatic plasma levels of Na+ and K+ Figure 26.8 Systemic blood pressure/volume Filtrate NaCl concentration in ascending limb of loop of Henle Stretch in afferent arterioles (+) Factors Affecting Urine Volume Inhibits baroreceptors in blood vessels (+) (+) (+) • Increased temperature Sympathetic nervous system Granular cells of kidneys Release (+) Renin Systemic arterioles Angiotensin I Angiotensinogen (from liver) – Increases vasodilation and perspiration – Decreases blood flow to kidneys Causes Catalyzes conversion Vasoconstriction Results in Converting enzyme (in lungs) (+) Peripheral resistance Angiotensin II Posterior pituitary • Decreased temperature (+) (+) Releases (+) Systemic arterioles Adrenal cortex ADH (antidiuretic hormone) – Increases blood flow to kidneys Secretes Causes (+) Vasoconstriction Aldosterone Results in Peripheral resistance Targets Collecting ducts of kidneys Causes Distal kidney tubules Causes H2O reabsorption Na+ (and H2O) reabsorption Results in Blood volume (+) stimulates Blood pressure Renin-angiotensin system Neural regulation (sympathetic nervous system effects) ADH release and effects Figure 26.10 Diuretics Factors Affecting Urine Output • Chemicals that increase urine output – Osmotic diuretics • Substances not reabsorbed – Glucose in a diabetic patient – ADH inhibitors • Alcohol and water – Substances that inhibit Na+ reabsorption • Caffeine, thiazides (class of medications), loop diuretics (inhibit Na+-K+-Cl- symport proteins) • • • • ↑ blood pressure ↑ blood solute concentration ↓ plasma proteins Psychological factors – Potassium levels are affected by some diuretics • Can be extremely dangerous 10