* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download presentation source
Cardiac contractility modulation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
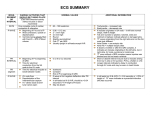
EKG Basics # 2 That Squigglely Line What Does It Really Mean ? Part # 2 David Arnall, Ph.D., P.T. (2000) The V Leads The Precordial Chest Leads Record The Heart’s Electrical Activity In The Transverse Or Horizontal Plane. http://www.publicsafetynet.net/12lead_dx.htm#electrode To Create The Six Precordial Chest Leads, Each Chest Lead Is Made Positive & The Whole Body Is Considered Negative. Lead Positioning V1 Is Placed In The Fourth Intercostal Space To The Right Of The Sternum. V2 Is Placed In The Fourth Intercostal Space To The Left Of The Sternum. V3 Is Placed In Between V2 And V4. V4 Is Placed In The Fifth Intercostal Space In The Midclavicular Line Near The Nipple. V5 Is Placed In Between V4 And V6. V6 Is Placed In The Fifth Intercostal Space In The Midaxillary Line. http://endeavor.med.nyu.edu/courses/physiology/courseware/ekg _pt1/EKGprecordial.html When placing the precordial chest leads across the thorax, the clinician places the electrodes under the pectoralis major & not over the breasts. In The Chest Cavity, The Heart Is Positioned With The Right Ventricle Lying Anteriorly & Medially While The Left Ventricle Lies Anterolaterally & Posteriorly Therefore, Leads V1 & V2 Lie Directly Over The Right Ventricle. Their Line Of Sight Is To View The Electrical Activity Coming From The Right Ventricle. Leads V3 & V4 Lie Directly Over The Interventricular Septum. Their Line Of Sight Is To View The Electrical Activity Of The Interventricular Septum. http://endeavor.med.nyu.edu/courses/physiology/courseware/ekg _pt1/EKGprecolead.html Leads V5 & V6 Lie Over The Left Ventricle. Therefore, These Leads View The Electrical Activity Of The Left Ventricle. The Precordial Chest Leads Can Be Divided Up Into Areas Of The Heart They View. Leads V1, V2, V3, & V4 Are The Anterior Leads. Leads V5 & V6 Look At The Left Lateral Wall. In Review Anterior Chest Leads V1, V2, V3 & V4 Left Lateral Wall Leads aVL, Lead I , V5 & V6 Inferior Chest Leads Lead II, Lead III, & Lead aVF No Man’s Land aVR A Review Of The Waves & Intervals Of The EKG The P Wave The P Wave Is The Signal That Electrical Potential Has Left The SA Node, Swept Across The Atria, & Has Initiated Atrial Contraction. What Is A Normal P Wave ? Duration : The Normal Duration Of A P Wave is 2.0 2.5 mm (.04 - .1 sec) If It Is Greater Than 2.75 mm (.11 sec) It Is Considered To Be An Abnormal P Wave. http://www.ovcnet.uoguelph.ca/ClinStudies/Courses/Public/Card iology/Concepts/ECGConcepts13-16.htm Amplitude A Normal Amplitude For A P Wave Is 2-3 mm. The P Wave Should Always Be Gently Rounded - Never Pointed Or Peaked. Abnormal Amplitude Of The P Wave Is Often Seen In Cor Pulmonale, A-V Valve Disease, Hypertension & In Patients With Congenital Heart Disease P Waves Within The Same Lead That Are Multiformic Indicate The Presence Of More Than One Pacemaker In The Right Atrium. In The Six Limb Leads, You Will Generally See P Waves In The Upright Position Except In aVR & V1 Where They Are Negatively Deflected. http://bioscience.org/images/normalh.gif You Will Frequently See Biphasic P Waves In Lead III, Lead V2 & Occasionally In Lead aVL. BiPhasic P Wave In V1 The PR Interval After The P Wave There Is A “Silent Period” Where Nothing Is Happening In The EKG Tracing. This Quiescent Period Is Called The PR Interval. The PR Interval Is A Time Lag And Represents The Period During Which There Is AV Nodal Capture Of The SA Node Signal. The PR Interval Allows The Atria To Contract (atrial systole) Which “Tops Off” The Ventricles With Blood - An Event Called Atrial Kick. The PR Interval Is Measured From The Beginning Of The P Wave To The Beginning Of The Q Wave Or The Beginning Of The R Wave If The Q Wave Is Absent. http://doyle.ibme.utoronto.ca/EKG/rhythm/EKGTUTORIAL.htm The PR Interval Represents The Time Period Encompassing Atrial Depolarization Up To But Not Including The Start Of Ventricular Depolarization. “A major portion of the PR interval reflects the slow conduction through the AV node which is controlled by the sympathetic-parasympathetic balance within the autonomic nervous system”. Marriott’s Practical Electrocardiography, 9th ed., Galen S. Wagner, pg 39, 1994 Duration : The Adult PR Interval Is Normally Between 3-5 mm Or .12 - .20 Seconds In Duration. Some Cardiologists Will Say It Is Normal Out To .22 Seconds (5 1/2 mm) If The PR Interval Is Longer Than 5 mm, It Is Called A Prolonged PR Interval & May Indicate The Presence Of An AV Block. First Degree AV Block The PR Interval Shortens During Exercise Because Of The Sympathetic Tone That Predominates Over The Heart. If The PR Interval Could Not Shorten, Along With Other Segments In The EKG, Then Acceleration Of Heart Rate During Exercise Would Be Difficult If Not Impossible. In Young Children, The PR Interval Is Shorter Than In Adults. The Child’s Heart Rate Is Also Faster. In A 1 Year Old Child At Rest, The Normal P-R Interval Is Typically .11 sec. Or Slightly Under 3 mm. For Children Who Are 6 Years Of Age, The P-R Interval At Rest Is .13 Seconds Or Slightly Over 3 mm. In Children 12 Years Of Age, The P-R Interval At Rest Will Be .14 Seconds Or About 3.5 mm. In Grown Adults 18 Years Of Age And Older, The P-R Interval At Rest Will Be 3-5 mm In Length. Prolonged P-R Intervals Are Symptomatic Of : AV Blocks Due To Coronary Disease & Rheumatic Fever. Sometimes, Prolonged P-R Intervals Not Related To Heart Disease, Can Be Seen In Healthy Athletes - An Aberration Called A Normal Variant. This Can Be Seen In About ~ 1% - 2% Of The Healthy, Young Population. Pathologies Resulting In PR Interval Shortening Shortened P-R Intervals Are Seen In Patients With Pheochromocytoma And Wolfe-Parkinson-White Syndrome Pheochromocytoma is a tumor in the adrenal medulla that results in a greater-than-normal release of catecholamines. The high blood concentration of catecholamines causes the heart rate to accelerate. Wolff-Parkinson-White Syndrome is a medical condition in which atrioventricular myocardial accessory pathways electrically pre-excite the ventricles to contract producing an extremely short PR interval. These accessory electrical pathways are remnants of fetal pathways that did not disappear after birth. The Bundle Of Kent has been implicated as a common aberrant pathway in W-P-W. W-P-W occurs in ~ .15% - .20% of the population or 2:1,000 people. Patients with W-P-W are otherwise healthy. W-P-W effects men more than women and can evolve into atrial and ventricular dysrhythmias with a general mortality up to 4% of the effected population. Patients with W-P-W often complain of episodic symptoms that include chest discomfort, dizziness, and palpitations. http://homepages.enterprise.net/djenkins/ecghome.html http://www.heartinfo.org/physician/ecg/wpw.htm The Q Wave Definition : The Q Wave Is The First Downward Deflection After The P Wave & Before The R Wave. Sometimes Q Waves Are Present & Sometimes They Are Absent Depending On The Lead. It is common to normally see Q waves in leads I, II, aVL and in V4-6. A Normal Q Wave Is Not Wider In Duration Than 0.5 mm Or About .02 Seconds. Its Normal Amplitude Is < 1 mm. Q Waves Are An Indication Of Ventricular Septal Wall Depolarization. They Appear Before The QRS Complex Because The Fascicle That Conducts The Signal Is Higher Than The Right And Left Bundle Branch That Give You The QRS Complex. Q Waves Of Normal Size Have No Diagnostic Meaning In Normal Hearts Except That The Septum Has Depolarized. Significant Q Waves Q waves In Leads I, II, aVF, & aVL Can Mean Something If ... 1. They Are Between 25% - 33% Of The Amplitude Of The R Wave. 2. They Are Greater Than 0.04 Seconds (1 mm) In Duration. Q waves of any size are normal in leads aVR. If They Are 25%-33% Of The Total Amplitude Of The R Wave, Then They Are Significant For The Presence Of An MI In The Lead Where The Q Wave Appears. In Other Words, If The Significant Q Wave Appears In Leads II, III Or aVF, Then The MI Must Have Occurred In The Inferior Portion Of The Heart The Right Coronary Is Blocked. If The Significant Q Wave Appeared In Lead I Or aVL, Then The MI Must Have Occurred In The Antero-Lateral Or Lateral Portions Of The Left Ventricle. Since Lead I & aVL Cover The Lateral Wall Of The Left Ventricle, Then The Occlusion Likely Occurred In The Circumflex Or The Marginal Branches Of The Left Coronary. Use The Precordial Chest Leads To Look For Significant Q Waves For The Presence Of An MI In The Anterior Portion Of The Heart V1 - V6 - The LAD Is Occluded. The R Wave Definition : The R Wave Is The First Upward Deflection After The P Wave. In the precordial chest leads, there should be an R wave progression - i.e. - an ever increasing amplitude of the R wave from V1 through V6 http://www.heartinfo.org/physician/ecg/norm.htm R wave progression occurs because the precordial chest leads sweep across the thoracic cage looking from the thinner right ventricle across to the thicker left ventricle. Loss of the R wave progression is abnormal and signals the possible presence of bundle branch blocks or the occurrence of a myocardial infarction. The S Wave Definition : The S Wave Is Defined As The First Downward Deflection After The R Wave. There is a normal progressive decrease in the size of the S wave in the precordial leads. V1 through V2 should have large S waves with a decreasing appearance of S through V5 and V6. http://www.heartinfo.org/physician/ecg/norm.htm QRS Complex Generalities Mostly Upward Deflected QRS Complexes Are Found In Leads I, II, III, aVF, aVL, V4, V5, and V6. Mostly Downward Deflected QRS Complexes Will Be Seen In Leads aVR And V1,V2, And Sometimes V3. The QRS Complex Signals The Depolarization Of The Ventricles. A Normal QRS Complex Has A Duration of ~ .06 - .12 Sec. Or About 1.5 - 3.0 mm. If The QRS Is >3mm, The Medical Staff Will Construe It To Mean There Is An Abnormal Intraventricular Conduction Pathway. The ST Segment The ST Segment Is The Pause After The QRS Complex - The Interval Between The End Of The QRS Complex & The Beginning Of The T Wave. It Symbolizes The End Of Ventricular Depolarization To The Start Of Ventricular Repolarization. It Is During This Phase Of The EKG When The Heart Is Being Passively Perfused - The Windkessel Effect. The ST Segment Slopes Gently Up Toward The Isoelectric Line From The J Point And Ends At The Beginning Of The T Wave. The ST Segment Normal EKG w/ J Point In aVL Normal Up Sloping Of The ST Segment May Be 1-2 mm In IndoEuropeans And As Much As 4 mm In African-Americans The Normal Duration Of The ST Segment Is About 2-3 mm. ST Segment Elevation When The ST Segment Is Elevated In A Patient With Known Disease, It Is Usually A Sign Of An Evolving Transmural Infarction - An MI In Progress. ST Segment Elevation ST Segment Elevation So...., The Classic Signs Of An Acute MI In Progress Are : –Elevated ST Segment –Inverted T Wave –Presence Of A Q Wave Signs Of An Anterior Wall Infarction Anterior Wall Infarction An anterior wall MI is usually caused by an occlusion of the LAD EKG changes are seen in any of the precordial chest leads - V1 - V6 ST Segment Changes With An Acute Anterior MI ST segment elevation in V1-V6 and in Leads I and aVL (the lateral wall leads). Reciprocal ST segment depression in Leads II, III & aVF (the inferior leads) Acute Anterior Myocardial Infarction http://homepages.enterprise.net/djenkins/ami.html In An Uncomplicated MI, These EKG Changes Will Largely Disappear Once The Infarction Has Frankly Resolved - Usually In About 3 Or More Days. Mature Anterior Wall MI Signs Of An Inferior Wall Infarction Inferior Wall Infarction This infarction occurs on the diaphragmatic surface of the heart. It is frequently caused by an occlusion to blood flow through the right coronary ST Segment Changes With An Acute Inferior MI ST segment elevations in Leads II, III and aVF Reciprocal ST segment changes in Leads I, aVL, V1-V6. Acute Inferior Myocardial Infarction http://homepages.enterprise.net/djenkins/ami.html In An Uncomplicated MI, These EKG Changes Will Largely Disappear Once The Infarction Has Frankly Resolved - Usually In About 3 Days. A Mature Inferior Wall MI Old Inferior Wall MI Signs Of A Lateral Wall Infarction Lateral Wall Infarction This type of MI involves the lateral wall of the heart - the left ventricle. It is often caused by an occlusion to blood flow through the circumflex artery. ST segment elevations will be seen in the lateral chest leads Leads I, aVL and V5 and V6. Acute Lateral Wall MI In An Uncomplicated MI, These EKG Changes Will Largely Disappear Once The Infarction Has Frankly Resolved - Usually In About 3 Days. Mature Lateral Wall Infarct For All Types Of MI’s, The Q Wave Often Remains As The Only Residual Sign That An Infarction Has Occurred. Also, The ST Segment May Be Permanently Depressed. ST Segment Depression When The ST Segment Is Depressed, Then It Is Usually A Sign Of Cardiac Ischemia. ST Segment Depression Types Of ST Segment Depression ST Segment Depression May Be A Permanent Part Of The EKG Tracing. At Rest The Patient May Have A Normal ST Segment. However, It May Become Depressed As The Person’s Exercise Level Is Increased Above The Heart’s Ability To Receive Adequate Perfusion. The ST segment depression will begin to appear as the heart becomes ischemic It will continue to be more depressed the more ischemic the heart becomes. The ST segment will normalize once the exercise intensity is reduced to a level in which the heart receives enough perfusion to support the work that is being demanded. The T Wave The T Wave Represents Repolarization Of The Ventricles. Repolarization Proceeds From The Apex Of The Heart To The Base Of The Heart. In Normal Hearts, The T Wave Is Usually Upright In Leads I, II, III, aVF, aVL, & V2-V6. In Normal Hearts, The T Wave Will Usually Be Upside Down In aVR And V1. The Normal Duration Of The T Wave Is About 1-2 mm. Normal Amplitude For The T Wave Is Highly Variable. T Waves Get Taller During GXT’s And Exercise. T Waves During Infarction With infarction, the T wave usually becomes tall and narrow referred to as “peaking”. With time and the onset of ischemia, the T wave will invert. The QT Interval The QT Interval Encompasses The Time From The Beginning Of The Q Or R Wave Through The End Of The T Wave. The QT Interval Represents 40% Of The Normal Cardiac Cycle Whether At Rest Or During Exercise. The QT Interval Becomes Shorter As The Heart Rate Increases. Summary Of Durations & Amplitudes Of The P-QRS-T P Waves Normal Duration : 2.5 mm Normal Amplitude : 2-3 mm PR Intervals Normal Duration : 3-5 mm Q Waves Normal Duration : < .5 mm Normal Amplitude : <25% of R amplitude or ~ 1.0 mm QRS Complex Normal Duration : < 3.0 mm Normal Amplitude : Variable ST Segment Normal Amplitude : 1-2 mm Normal Duration : 2-3 mm T Wave Normal Duration : 2 mm Normal Amplitude : < 5 mm in Limb Leads & < 10 mm in Precordial Leads