* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Endocrinology of Aging
Testosterone wikipedia , lookup
Growth hormone therapy wikipedia , lookup
Hyperandrogenism wikipedia , lookup
Hormonal breast enhancement wikipedia , lookup
Hormone replacement therapy (female-to-male) wikipedia , lookup
Hormone replacement therapy (menopause) wikipedia , lookup
Hormone replacement therapy (male-to-female) wikipedia , lookup
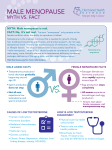
Chapter 28 / Endocrinology of Aging 419 28 Endocrinology of Aging Steven W. J. Lamberts, MD, PhD CONTENTS INTRODUCTION CHANGES IN HORMONE ACTIVITY DURING AGING MENOPAUSE ANDROPAUSE ADRENOPAUSE SOMATOPAUSE 1. INTRODUCTION Throughout adult life, all physiologic functions gradually decline. There is a diminished capacity for cellular protein synthesis, a decline in immune function, an increase in fat mass, a loss of muscle mass and strength, and a decrease in bone mineral density (BMD). Most elderly individuals die from the complications of atherosclerosis, cancer, or dementia. However, in an increasing number of the healthy elderly, loss of muscle strength is the limiting factor that determines their chances of living an independent life until death. Muscle weakness can be caused by aging of muscle fibers and their innervation, pain related to osteoarthritis, and chronic debilitating diseases. In addition, a sedentary lifestyle and decreased physical activity and disuse seem, to be very important determinants in this decline in muscle strength, because exercise training even at a very old age has been demonstrated to reverse significantly the decline in physical capacity. In other words, “use it or lose it;” activity is an extremely important treatment for aging. As the average length of life in Western societies increases further, so does the interest in understanding the considerable variations that have been observed in the course and speed of the aging process within groups From: Endocrinology: Basic and Clinical Principles, Second Edition (S. Melmed and P. M. Conn, eds.) © Humana Press Inc., Totowa, NJ of otherwise healthy individuals, with some people exhibiting extensive decline in physiologic functions with age and others little or none. Genetic factors, lifestyle, and societal investments in a safe and healthy environment are considered to be important determinants of successful aging. As life expectancy increases further in the coming years, it becomes more and more important to find interventions that might compress morbidity during the last part of life, with the goal to increase the number of years of healthy life with a full range of functional and mental capacity, without necessarily prolonging life. Traditionally, the endocrine system in humans has been implicated as a driving part of the aging process. The availability of hormone replacement of all known hormones that might play a role in the aging process has supported this idea. Many signs and symptoms observed in young individuals with selected hormone deficiencies are similar to changes observed during the aging process, and hormone replacement in young individuals reverses virtually all these problems. Apart from these considerations concerning the role of hormones in the physiology of the aging process, the two clinically most prevalent and important changes in endocrine activity during aging that represent pathology (i.e., diseases) are in glucose tolerance and thyroid function. 419 420 Part IV / Hypothalamic–Pituitary complications at an accelerated rate. Pancreatic insulin receptor and postreceptor changes associated with aging are critical components of the endocrinology of aging; apart from relative decreased insulin secretion by β-cells, peripheral insulin resistance related to poor diet, physical inactivity, increased abdominal fat mass, and decreased lean body mass contribute to the deterioration of glucose metabolism. Dietary management, exercise, oral hypoglycemic agents, and insulin are the four components of treatment of these patients, whose medical care is costly and intensive. 1.2. Changes in Thyroid Function Fig. 1. During aging, declines in the activities of a number of hormonal systems occur. Prolactin (PRL), TSH (thyrotropin), and T4 (thyroxin) levels in general remain unchanged. (Left) A decrease in growth hormone (GH) release by the pituitary gland causes a decrease in the production of insulin-like growth factor-1 (IGF-1) by the liver and other organs (somatopause). (Middle) A decrease in the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) and decreased secretion at the gonadal level (from the ovaries, decreased E2 causes menopause, and from the testicles, decreased testosterone [T] causes andropause, respectively). Immediately after the initiation of menopause, serum LH and FSH levels sharply increase. (Right) The adrenocortical cells responsible for the production of dehydroepiandrosterone (DHEA) decrease in activity (adrenopause), without clinically evident changes in adrenocorticotropic hormone and cortisol secretion. A central pacemaker in the hypothalamus or higher brain centers (or both) is hypothesized, which together with changes in the peripheral organs (the ovaries, testicles, and adrenal cortex) regulates the aging process of these endocrine axes. (Reproduced with permission from Lamberts et al., 1997.) 1.1. Glucose Tolerance and Diabetes Mellitus Approximately 40% of individuals 65–74 yr old and >50% of individuals over 80 have impaired glucose tolerance or diabetes mellitus, and nearly half of these elderly diabetics are undiagnosed. These persons are at risk of developing secondary, mainly macrovascular Age-related thyroid dysfunction is common in the elderly. Lowered concentrations of plasma levorotators thyroxine (T4) and increased thyrotropin-stimulating hormone (TSH) occur in 5–10% of elderly women. These abnormalities seem to be mainly caused by autoimmunity and may therefore be an expression of ageassociated disease, rather than a consequence of the aging process. It is well recognized that the general symptoms of aging can be easily confused with hypothyroidism, and in the past, decreased thyroid function was believed to be one of the hallmarks of the aging process. During aging a complex number of changes occur in thyroid hormone concentrations. Reduced outer-ring deiodination mediated by type I deiodinase results in a decline in T4 degradation, with a reduced generation of triiodothyronine (T3) and a decreased clearance of reverse T3. In addition, TSH secretion appears to be slightly decreased in healthy elderly humans when subjects with subclinical hypothyroidism are carefully excluded. The reason for such age-dependent reduction of TSH is uncertain. However, in spite of these complex changes in biochemical parameters, recent studies suggest that normal aging is associated with essentially normal thyroid function. The slight decrease in plasma T3 concentration occurs largely within the broad normal range of the healthy elderly population, and this decrease has not been convincingly causally related to functional changes during the aging process. Evaluation of thyroid function in the elderly is necessary on a regular basis because of the increased prevalence of autoimmune subclinical hypothyroidism and nonthyroidal illness. 2. CHANGES IN HORMONE ACTIVITY DURING AGING During aging three other hormonal systems show decreasing circulating hormone concentrations (Figs. 1 and 2), and these decreases have been considered mainly physiologic. In recent years, hormone replacement strat- Chapter 28 / Endocrinology of Aging 421 Fig. 2. Changes in hormone levels of healthy women (left) and men (right) during aging process. (A,B) Estrogen secretion throughout an individual healthy woman’s life (expressed as urinary estrogen excretion) (A) and mean free testosterone index (ratio of serum total testosterone to sex hormone–binding globulin levels) during the life of healthy men (B). (C,D) Serum DHEAS and E and F serum IGF-1 levels in healthy women and men during aging process. Note the difference in the distribution of ages in different panels. (Reproduced with permission from Lamberts et al., 1997.) egies have been developed in each case, but many of their aspects remain controversial, and increasing hormone blood levels to those found in 30- to 50-yr-old individuals has not been universally proven to be safe and of benefit. 3. MENOPAUSE The most dramatic and rapidly occurring change in women around the age of 50 is menopause. Cycling estradiol (E2) production from the ovarian follicles is suddenly exhausted, reproduction stops, and (very) low, constant E2 levels remain, mainly produced by aromatization of adrenal androgens in nonendocrine tissues, such as adipose tissue. This acute drop in circulating estrogen levels and the permanent cessation of menstruation around age 50 yr is often accompanied by vasomotor reactions, sleep disturbances, changes in skin and body composition, and a 422 depressed mood. The use of hormone replacement therapy ([HRT], estrogens or estrogen plus progestogen) rapidly alleviates these symptoms of menopause. In women with these symptoms, HRT also improves verbal memory, vigilance, reasoning, and motor speed, but there is no enhancement of other cognitive functions. Generally, no benefits of HRT are observed in asymptomatic women. Currently, the long-term use (5–10 yr or more) of HRT after menopause is surrounded by controversy; many studies in the past indicated advantages regarding prevention of the three chronic disorders most common in elderly women: cardiovascular diseases, osteoporosis, and dementia. However, these beneficial effects are a double-edged sword because long-term HRT is accompanied by a significant increase in the incidence of breast cancer, thrombosis, and stroke. The controversy has arisen partly because of differences in the selection of participating menopausal women in the large prospective trials with HRT. For example, the inclusion of nurses, who are probably more aware of the advantages of healthy lifestyle than the “normal” population of menopausal women, might have introduced a “healthy user bias” in several of the best prospective clinical trials, which were, however, mostly observational and not randomized controlled. In 2002, the interim results of the Women’s Health Initiative Trial were published. This is a randomized controlled trial to assess the risks and benefits of intervention strategies in the postmenopausal population in t he United States. The trial has in fact shown that HRT increases the risk of developing cardiovascular disease, including coronary heart disease (the primary outcome) and stroke, although it showed benefits for preventing hip fractures and bowel cancer. The relative risks of developing invasive breast cancer, coronary heart disease, and stroke were increased, although the absolute risks remained very small. One treatment arm of the trial included more than 16,000 postmenopausal women who were taking continuous combined estrogenprogestagen HRT, using conjugated equine estrogens (0.625 mg) plus medroxyprogesterone acetate (2.5 mg daily), tested against placebo. This primary prevention study was due to run for 8.5 yr, but was halted at just over 5 yr because the number of cases of breast cancer had reached a prespecified safety limit. For 10,000 women taking HRT each year, compared with those not taking it, there would be an additional eight cases of invasive breast cancers, seven heart attacks, eight strokes, and eight pulmonary embolisms. However, there would also be six fewer bowel cancers and five fewer hip fractures. Overall mortality was not increased with therapy. Part IV / Hypothalamic–Pituitary The decision to stop the trial and to change US recommendations for the use of postmenopausal HRT for primary prevention of chronic conditions might not be automatically applicable. First, one should realize that the weight and BMI of the US female population were, in general, high, and these factors alone make the participants more prone to breast cancer, stroke, thrombosis, and cardiovascular disease while in their excess adipose tissue enough estrogens might have been produced by aromatization of adrenal androgens, making the intake of additional HRT a pharmacologic rather than a replacement therapy. Second, more and more evidence is provided that genetic testing, such as for estrogen receptor (ER) polymorphisms and factor V Leiden, will not only better predict a positive outcome of HRT on cardiovascular disease, but the chances of developing thrombosis as well. Third, HRT’s potential impact on the incidence of dementia needs to be considered. Women seem to be at higher risk of developing Alzheimer disease, and this is in part owing to their increased longevity. It has been suggested that the abrupt decline of estrogen production at menopause may be associated with a vulnerability of the female brain. Elderly men have an intrinsic supply of estrogen because they aromatize testosterone into estradiol within the brain. There is strong experimental evidence that in the intact brain estradiol might play a key neuroprotective role by delaying the initiation phase of onset of neurodegenerative disease. It was demonstrated that in mice lacking the ERα, estrogen protects the brain from injury by accelerating and amplifying the activity of this receptor. As a consequence, genes that help the brain cells survive are activated, or genes that harm the brain cells are suppressed. Postmenopausal HRT was considered to prevent or delay cognitive decline and dementia in postmenopausal women. In a systematic review and metaanalysis of all observational studies conducted thus far, it was concluded that HRT started at age 50, at the start of menopause, is associated with a decreased risk of dementia (summary odds ratio: 0.66; 95% confidence interval: 0.53–0.82). However, many of these studies also have important methodologic limitations, with the healthy user bias mentioned earlier an important one. In the Women’s Health Initiative Trial, a randomized controlled trial, in which HRT was started at age 65, no improvement of cognitive function was observed. HRT administered for 1 yr in women with mild to moderate Alzheimer disease did not slow disease progression, nor did it improve global, cognitive, or functional outcome. However, the use of high-dose estrogens to improve cognition in women with demen- Chapter 28 / Endocrinology of Aging tia was reported in a small study. In a prospective study of incident dementia among 1357 men (mean age: 73.2 yr) and 1889 women (mean age: 74.5 yr) residing in a single county in Utah, it was again demonstrated that prior HRT use is very closely associated with reduced risk of dementia. There was a highly statistical HRT duration-dependent decrease in incident dementia in women after the age of 80, with a decrease in incident dementia in women who had used HRT more than 10 yr in the past compared with that found in men. There was no apparent benefit of current HRT in the older group of women. These considerations on the advantages and risks of HRT in healthy postmenopausal women are very sobering. There is no doubt that early HRT, taken immediately at menopause, alleviates most symptomatology and is, in principle, safe in the shortterm. In women in whomcardiovascular disease is symptomatic, other (preventive) medications including β-blockers, ACE-inhibitors, aspirin, and/or statins have been proven to be effective. In addition, in symptomatic osteoporosis, bisphosphonates have preventive efficacy similar to or even better than HRT. Recent studies demonstrated that a higher than usual dietary intake of phytoestrogens (isoflavones and lignans) is associated with a lower aortic stiffness in postmenopausal women, suggesting that phytoestrogens have a protective effect on the risk of atherosclerosis and arterial degeneration through an effect on arterial walls, especially among older women. Interestingly, alcohol consumption was also inversely associated with aortic stiffness, supporting the concept that moderate alcohol consumption decreases the risk of cardiovascular disease in postmenopausal women. In summary, the verdict on the use of HRT in healthconscious women is, in general, negative at present. With the further development of genetic testing to identify those women who might benefit most, and/or are most at risk for thrombotic events and/or breast cancer, the decision to prescribe HRT early after menopause in order to obtain the early beneficial effects on subjective well-being, as well as possible late delaying effects on dementia, might remain an option. 3.1. Selective ER Modulators A new development in the preventive treatment of the consequences of long-term estrogen deficiency in menopause is the availability of targeted estrogen replacement therapy using selective estrogen receptor modulators (SERMs). Early studies using tamoxifen in the treatment of breast cancer indicated variable estrogenic and antiestrogenic actions of the compound in different organs. Tamoxifen suppresses the growth 423 of ER-positive breast cancer cells; in addition, longterm tamoxifen treatment of patients surviving breast cancer indicated a partial protection against age-related decrease in BMD. These observations were explained by the fact that tamoxifen, and other compounds such as raloxifene, have antiestrogenic actions on normal and cancerous breast tissue, but agonistic actions on bone, lipids, and blood vessel walls. The differential effects of these SERMs in different organs may be explained by the activation of different forms of ER, in which the form is the “classic” estrogen, whereas the β form mediates the vascular and bone effects of estrogens. Raloxifene, in contrast to tamoxifen and estradiol, does not stimulate endometrial thickness and vaginal bleeding. It has protective effects for vertebral fractures in menopausal women with osteoporosis. A very promising effect of raloxifene is its reported chemoprotective action on breast cancer. 4. ANDROPAUSE Age-associated hypogonadism develops not as clearly in men as in women. The key difference from menopause is the gradual, often subtle change in androgen levels in men compared with the precipitate fall of estrogen production in women (Fig. 2). There is general agreement that as men age, there is a decline in the concentration of serum total testosterone that begins after age 40. In cross-sectional studies, the annual decline in total and “free” testosterone is 0.4 and 1.2%, respectively. The higher decline in free testosterone levels is related to the increase in levels of SHBG with aging. “Andropause” is characterized by a decrease in testicular Leydig cell numbers and in their secretory capacity, as well as by an age-related decrease in episode and stimulated gonadotropin secretion. It remains unclear whether the well-known biologic changes during aging in men, such as reduction in sexual activity, in muscle mass and strength, and in skeletal mineralization, are causally related to these changes in testosterone bioactivity (“andropause”). In a group of more than 400 independently living elderly men ages 73–94 (mean age: 78 yr), a positive association was observed between serum total and free testosterone concentrations and muscle strength as well as an inverse relationship with fat mass. In addition, low bioavailable testosterone was associated with a depressed mood in a population-based study in 856 men (age: 50–89). Many persuasive reports in the literature demonstrate that treatment of men of all ages (young, adult, and old) with clear clinical and biochemical hypogonadism with testosterone replacement instantly reverses vasomotor activity (flushes and sweats): improves libido, sexual 424 activity, and mood; increases muscle mass, strength, and bone mineralization; prevents fractures; decreases fat mass; and decreases fatigue and poor concentration. Additionally, the treatment of adult healthy men with supraphysiologic doses of testosterone, especially when combined with resistance exercise training, increases fat-free mass and muscle size and strength. A search for studies reporting the results of androgen therapy in older men demonstrates that most studies were small, short-term, noncontrolled, and without uniform endpoints. Numerous studies of large populations of healthy men have shown a marked rise in the incidence of impotence to >50% in men ages 60–70. Although this increase in impotence occurs in the same age group that shows a clear decline in serum (free) testosterone levels, no causal relationships have been demonstrated. Testosterone replacement therapy in elderly men is in most instances not effective for the treatment of loss of libido or impotence in individuals with serum testosterone concentrations within the normal age-matched range; other factors such as atherosclerosis, alcohol consumption, smoking, and the quality of personal relationships seem to be more important denominators. Only in the case of clear hypogonadism are the decrease in libido and potency restored by testosterone therapy. This suggests that there is a theshold level of testosterone in the low normal range, below which libido and sexual function are impaired and above which there is no further enhancement of response. Summarizing the literature available on the preventive treatment of healthy elderly men with testosterone at a dose that increases serum testosterone concentrations to those observed in 20-to 30-yr-olds demonstrates limited anabolic effects on body composition (a slight decrease in fat mass, and a slight increase in muscle mass). In addition, minor beneficial effects on muscle strength or physical performance have been observed in a minority of studies. Detailed analysis of a number of studies in which elderly men selected on the basis of the presence of “low” pretreatment serum testosterone concentrations suggests a beneficial effect of testosterone replacement therapy on muscle strength, BMD, mood, as well as (subjective) aspects of the quality of life. In conclusion, testosterone at supraphysiologic doses when administered to eugonadal men increases muscle mass and strength. “Replacement” therapy directed at restoring serum testosterone therapy in healthy elderly males to levels observed between the age of 30 and 50 lowers fat mass and increases lean mass to a limited extent without a clear beneficial effect on muscle strength and physical performance. At Part IV / Hypothalamic–Pituitary present, it remains uncertain whether testosterone replacement produces clinically meaningful improvements in muscle function without significant adverse effects in frail older men or in elderly men with serum testosterone concentrations between 7.0 and 11.4 nmol/L. If one decides to start testosterone replacement the major goal of therapy is to replace testosterone levels to as close to “physiologic” age-matched levels as possible. The dose should thus be titrated according to serum levels. At present, the duration of administration of testosterone is uncertain. Control of prostate size, prostate-specific antigen levels, and hematocrit levels is mandatory. The identification of elderly men who might benefit most from testosterone treatment remains uncertain, and the risks to the prostate and possible effects on the process of atherosclerosis remain subjects for study. The concept of developing androgenic compounds with variable biologic action in different organs (selective androgen receptor modulation) is currently being pursued. 5. ANDRENOPAUSE 5.1. Dehydroepiandrosterone Humans are unique among primates and rodents because the human adrenal cortex secretes large amounts of the steroid precursors DHEA and its sulfate derivative DHEAS. Serum DHEAS concentrations in adult men and women are more than 100 times higher than those of testosterone and more than 1000 times higher than those of estradiol. In healthy subjects, serum concentrations of DHEAS and its sulfate are highest in the third decade of life, after which the concentrations of both gradually decrease, so that by the age of 70–80 yr, the values are about 20% of peak values in men and 30% of peak values in women (Fig. 2). Both DHEA and DHEAS seem to be inactive precursors, which, via a number of enzymes, are transformed within human tissues by a complicated network of enzymes into androgens and/or estrogens. The key enzymes are aromatase, steroid sulfatase, 3β-hydroxysteroid-dehydrogenases, and at least seven organ-specific 17β-hydroxysteroid dehydrogenases. Labrie introduced the name “intracrinology” to describe this synthesis of active steroids in peripheral target tissues, where the action is exerted in the same cells in which synthesis takes place, without release in the extracellular space and general circulation. In postmenopausal women, nearly 100% of sex steroids are synthesized in peripheral tissues from precursors of adrenal origin except for a small contribution from ovarian and/or adrenal testosterone and androstenedione. Thus, in postmenopausal women, virtually all active sex ste- Chapter 28 / Endocrinology of Aging roids are made in target tissues by an intracrine mechanism. Also in elderly males the intracrine production of androgens is important: less than 50% of androgens is derived from testicular production. As already stated, the situation of a high secretion rate of adrenal precursor sex steroids in men and women is completely different from animal models used in the laboratory, in which the secretion of sex steroids takes place exclusively in the gonads. In many experiments, it has been demonstrated that (long-term) administration of DHEA to rats and mice prevents obesity, diabetes mellitus, cancer, and heart disease, while it enhances immune function. These experimental animal data have been used as an argument that administration of DHEA in adult/elderly individuals prolongs life-span and might be an “elixir of youth.” Supportive data in humans are few, however, and highly controversial. Several randomized placebo-controlled studies demonstrated that oral administration of DHEA might have beneficial effects on perceived physical and psychologic well-being in both sexes without an effect on libido. A number of other, well-controlled trials with DHEA subsequently did not demonstrate a clinically significant effect. A physiologic functional role of DHEA in women has been demonstrated. However, in a careful doubleblind study in women with adrenal insufficiency, administration of DHEA (50 mg/d) normalized serum concentrations of DHEA, DHEAS, androstenedione and testosterone. DHEA significantly improved overall well-being, as demonstrated by scores for depression and anxiety, the frequency of sexual thoughts, sexual interest, as well as satisfaction with both mental and physical aspects of sexuality. In conclusion, DHEA(S) is a universal precursor to the peripheral local production and action of estrogens and androgens in the elderly. The addition of DHEA (50 mg) to the existing big pool of DHEA(S) in unselected elderly individuals has no or only limited clinical effects, especially in elderly women. It is unknown whether the increase in sex steroid levels induced by long-term administration of DHEA is safe regarding the development of ovarian, prostate, or other types of steroid-dependent cancers. DHEA is currently widely used within the United States as a “treatment against aging.” With the scientific verdict still out, without further confirmation of DHEA’s reported beneficial actions in humans, and without a better understanding of its potential risks, it is premature to recommend the routine use of DHEA for delaying or preventing the physiologic consequences of aging. 425 5.2. Cortisol Cortisol production by the adrenals seems to have a major impact on memory and cognition. In cross-sectional as well as longitudinal studies, it was demonstrated that higher cortisol levels are associated with poorer memory performance and a higher likelihood of memory decline, especially in women. The detrimental effects of cortisol seem to be directed at the hippocampus. An iv bolus of 35 mg of hydrocortisone reduces hippocampal glucose metabolism, as measured by positron emission tomography scan, in elderly individuals by 12–16%, and the hippocampal volume, measured by magnetyic resonance imaging, is smaller in patients with Cushing’s syndrome. In a small prospective study in healthy elderly individuals, an association between adrenal steroid hormones and cognitive function was confirmed. Free cortisol levels appeared to be associated with cognitive impairment, and a lower degree of cortisol suppression after administration of dexamethasone was associated with an increased risk of cognitive decline. These findings support the concept that stress and anxiety have important consequences regarding to the degree and speed of the decline in memory and other cognitive abilities in the elderly. Clear clinical developments regarding to medical intervention in this process remain elusive, however. 6. SOMATOPAUSE The third endocrine system that gradually declines in activity during aging is the GH/ IGF-1 axis. Mean pulse amplitude, duration and fraction of GH secreted, but not pulse frequency, gradually decrease during aging. In parallel, there is a progressive fall in circulating IGF-1 levels in both sexes. There is no evidence for a “peripheral” factor in this process of somatopause, and its triggering pacemaker seems mainly localized in the hypothalamus, because pituitary somatotropes, even in very old individuals, can be restored to their youthful secretory capacity during treatment with GH-releasing peptides. The expectation that this decline in GH and IGF-1 secretion contributes to the decline in functional capacity in the elderly (“somatopause”) is mainly derived from studies in which GH replacement therapy of GHdeficient adults was shown to increase muscle mass, muscle strength, bone mass, and the quality of life. A beneficial effect on the lipid profile and an important decrease in fat mass were also observed in such patients. As in hypogonadal individuals, adult GH deficiency can thus be considered a model of normal aging, because a number of catabolic processes that are central in the 426 Fig. 3. Schematic representation of the regulation of GH/IGF-1 axis, as well as potential hormonal intervention of different compounds to activate this axis on different levels (left). biology of aging can be reversed by administration of GH. In 1990, Rudman published the findings of a trial that provoked headlines in the popular press. In this trial, healthy older men were administered recombinant human GH, heralded as a treatment for aging. The initial optimism prompted many investigators to start clinical trials to investigate the possible benefits of GH in older people. However, today it seems fair to state that GH remains a promising treatment still looking for a proven indication. Rudman’s study concerned men with IGF-1 levels that were deficient by young adult standards. In the 12 men receiving active treatment for 6 mo, fat mass fell, lean body mass rose by 8.8% (p < 0.05), and lumbar vertebral density (but not other bone sites) rose by 1.6% (p < 0.05). Compared with age-related differences observed in cross-sectional studies, these were massive effects. However, the trial should only be regarded as a pilot study because the treatment groups were not randomized and the subjects were not blinded. In a subsequent similar study, only 18 of 62 subjects completed 12 mo of treatment without experiencing one or more of the three common side effects: carpal tunnel syndrome, gynecomastia, and hyperglycemia. Patients who produced higher IGF-1 levels experienced more side effects. Subsequent trials have generally confirmed the changes in fat and lean tissue but shown inconsistent effects on bone density. Part IV / Hypothalamic–Pituitary Furthermore, in contrast to the findings in younger GH-deficient adults with pituitary disease, the potentially beneficial changes in muscle and other lean body tissue obtainable in older people have not translated into improved functional abilities. Exercise programs have proven ability to enhance muscle mass and strength, even in very frail elderly people. Adding GH treatment to an exercise intervention produced no additional benefit for healthy males. Although the exercise-related GH responses of older people are attenuated, it has not been shown that a youthful GH response is necessary for older people to benefit maximally from exercise. Other components of the GH/IGF-1 axis are effective in activating GH and IGF-1 secretion (Fig. 3). Long-acting derivatives of the hypothalamic peptide GH-releasing hormone (GHRH) given twice daily subcutaneously for 14 d to healthy men 70 yr old increased GH and IGF-1 levels to those encountered in 35-yrolds. This finding supports the concept that somatopause is primarily hypothalamically driven, and that pituitary somatotropes retain their capacity to synthesize and secrete high levels of GH. GH-releasing peptides (GHRPs) are oligopeptides with even more powerful GH-releasing effects. Originally developed by design, it has recently been demonstrated that GHRPs mediate their GH-secretory effects through endogenous specific receptors. Nonpeptide analogs such as MK-677 and L692,429 have powerful GHreleasing effects, restoring IGF-1 secretion in the elderly to levels encountered in young adults. Long-term oral administration of MK-677 to healthy elderly individuals increased lean body mass, but not muscle strength. If proven to be GH specific, these orally active GHRP derivatives might be important alternatives to subcutanously administered GH for studies in the reversal of somatopause, in the prevention of frailty, and in the reversal of acute catabolism. Recombinant IGF-1 produces less fluid retention and lower blood glucose than GH. Four weeks of treatment of healthy older women (mean age: 71 yr) with either GH or recombinant human IGF-1 (rhIGF-1) produced potentially beneficial and adverse effects similar to those seen in men, although rhIGF-1 was better tolerated. In combination with a reducing diet and a program of exercise, these treatments produced weight loss in healthy but obese older women without compromising lean body mass or gains in muscle strength, but side effects were a problem, causing 5 of 33 subjects to drop out. In a 26-wk randomized, double-blind, placebo-controlled parallel-group trial in healthy elderly men and women, the effects of GH and/or sex steroids (testosterone in men, estrogens and progesterone in Chapter 28 / Endocrinology of Aging women) on body composition, strength, and endurance, as well as adverse effects were studied. GH with or without sex steroids induced in these healthy aged women and men the well-known increase in lean body mass and decrease in fat mass. The combination of GH and testosterone caused a marginal increase in muscle strength and maximum oxygen uptake in men, but women had no significant change in strength or cardiovascular endurance. Formation of edema, carpal tunnel syndrome, arthralgias, and deterioration of glucose tolerance or even development of diabetes frequently occurred, limiting the use of GH in aging. Another still unsolved issue is the safety of long-term administration of GH. Epidemiologic studies, together with many experimental data, suggest that the IGF-1 system is involved in tumor development and progression. It remains uncertain at present whether long-term GH treatment in the elderly thereby might contribute to the risk of prostate, breast, and/or colon cancer. In conclusion, the use of GH and/or other compounds that activate IGF-1 bioactivity in the treatment of the elderly, either as a preventive intervention delaying the aging process or as a treatment to counteract frailty and/ or catabolism, has not been proven to be safe and successful. At present, the use of GH therefore cannot be advised in elderly individuals. 427 REFERENCE Lamberts SW, van den Beld AW, van der Lely AJ. The endocrinology of aging. Science 1997;278:419–424. SUGGESTED READINGS Blackman MR, Sorkin JD, Münzer T, et al. Growth hormone and sex steroid administration in healthy aged women and men. JAMA 2002;288:2282–2292. Grady D. Postmenopausal hormones: therapy for symptoms only. N Engl J Med 2003;348:1835–1854. Labrie F, Luu-The V, Lin SX. Intracrinology: role of the family of 17 beta-hydroxysteroid dehydrogenases in human physiology and disease. J Mol Endocrinol 2000;25:1–6. Lamberts SW. The endocrinology of aging and the brain. Arch Neurol 2002;59:1709–1711. Li CI, Malone KE, Porter PL, Weiss NS, Tang MC, CushingHaugen KL, Daling JR. Relationship between long durations and different regimens of hormone therapy and risk of breast cancer. JAMA 2003;289:3254–3263. Riggs BL, Hartmann LC. Selective estrogen-receptor modulators: mechanisms of action and application to clinical practice. N Engl J Med 2003;348:618–629. Rowe JW, Kahn RL. Human aging: usual and successful. Science 1987;237:143-149. Rudman D, Feller AG, Nagraj HS. Effect of human growth hormone in men over 60 years old. N Engl J Med 1990;323:1–6. Vermeulen A. Androgen replacement therapy in the aging male: a critical evaluation. J Clin Endocrinol Metab 2001;86:2380– 2390.