* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Cardiac Disease and Anesthesia Anesthetic management of
Survey
Document related concepts
Remote ischemic conditioning wikipedia , lookup
Heart failure wikipedia , lookup
Electrocardiography wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Coronary artery disease wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Transcript
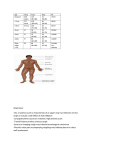
Cardiac Disease and Anesthesia Anesthetic management of patients with underlying heart disease can be very challenging as most anesthetic drugs depress cardiac function, alter vascular tone and heart rate as well as their potential for arrhythmogenesis. The subsequent reduction in cardiac output and arterial blood pressure decrease tissue perfusion with potential organ damage and patient death. Limited cardiac reserve as a consequence of the underlying heart disease enhances the cardio-‐depressant effects and restricts common methods of patient stabilization. Patient Evaluation Proper preanesthetic evaluation of the patient helps minimize deleterious effects of anesthesia, improving the overall patient safety. The anesthetist should review the patient’s history in search for evidence of clinical signs indicating deterioration of patient status and current medication regiment. The physical examination should also focus on the clinical status of the patient’s heart disease including hemodynamic assessment with blood pressure, hydration status, respiratory function and the presence of pleural/abdominal effusion. Blood urea nitrogen, creatinine and electrolytes need to be evaluated due to the high incidence of concurrent renal disease and diuretic induced electrolyte abnormalities. Thoracic radiographs are essential for assessment of cardiac size and the presence of pulmonary edema. ECG and echocardiography provide useful information but are not necessary in all cases. Anesthesia is contraindicated in patients with decompensated heart disease (ASA Catergory IV & V) until stabilization of cardiac complications. Anesthetic Drug Selection Due to the vast array of cardiovascular diseases affecting dogs and cats, one anesthetic protocol is not appropriate for all patients. Appropriate drug selection is based on an understanding of the cardiovascular pathophysiology and the cardiovascular effects of the anesthetic drugs. A multimodal approach using reduced dosages of drugs from multiple pharmacologic categories is preferred to minimize extreme cardiovascular effects of any one drug. Medications to Avoid While there are circumstances when the below drugs could be used in patients with heart disease, it is best to avoid them. Most of these medications are no longer in common use anyhow. o o o Alpha-‐2 Adrenergic Drugs § Intense vasoconstriction and depression of myocardial contractility § Bradycardia Barbiturates § Potent cardiovascular depressant effects § Arrhythmogenic Halothane § Greatest decrease on contractility of inhalants, arrhythmogenic Premedications The benefits of premedicating cardiac patients with a combination of a sedative and analgesic include reducing preoperative anxiety and stress, preemptive analgesia, lowering the amounts of induction agents and inhalants and a smoother recovery. Opioids do not affect contractility or stimulate arrhythmias. They may cause a mild decrease in blood pressure secondary to vasodilation and vagally mediated bradycardia responsive to anticholinergics. Most opioids do not possess profound sedative effects when administered alone in dogs and may trigger hyperexcitability in cats. Opioids used in combination with benzodiazepines for neuroleptanalgesia generally result in adequate sedation. The benzodiazepines also produce minimal cardiovascular effects with the potential for a mild vasodilation and myocardial depression. Acepromazine may be administered for sedation in patients with cardiovascular disease. However, it causes vasodilation secondary to alpha adrenergic blockade. Pending the disease, low dose acepromazine is beneficial with the decreased peripheral resistance or afterload increasing cardiac output. The sedative and vasodilatory effects of acepromazine are of long duration (4-‐6 hours) and nonreversible. Anticholinergics increase heart rate and myocardial oxygen consumption, increase the possibility of cardiac arrhythmias and decrease the threshold for ventricular fibrillation. Some patients may not tolerate excessive increases in heart rate. Therefore, anticholinergics should not be a routine component of the anesthetic protocol but reserved for treatment of bradycardia that limits cardiac output. Induction drugs The use of inhalant gases for induction by mask or chamber is not recommended for patients with cardiovascular disease due to associated stress, respiratory depression and potential for hypotension. Propofol causes a dose dependent decreased contractility and hypotension similar to that of the thiobarbituates. Use of preanesthetic medication greatly reduces dose of required propofol necessary for induction. Etomidate is the preferred drug for severe cardiac disease due to its minimal effects on myocardial contractility, heart rate and cardiac output. Etomidate may trigger vasodilation decreasing blood pressure. Etomidate has minimal effects on arrhythmia development. It may produce a rough induction with patient excitement, muscle twitching and vocalization. Effects are minimized by the administration of a benzodiazepine or acepromazine prior to administration. Ketamine is a commonly used induction agent in heart disease but never to be used alone. Ketamine indirectly increases heart rate, blood pressure and contractility by stimulation of the sympathetic nervous system. Such effects are beneficial in diseases with decreased contractility and low heart rates but can be detrimental in patients with hypertrophic cardiomyopathy, hypertension, hyperthyroidism and arrhythmias. Ketamine should also be used with caution in patients with end stage heart failure as a dose dependent decrease in myocardial contractility may occur secondary to catecholamine exhaustion. Maintenance Drugs Inhalant anesthetics all cause dose dependent cardiovascular depression. Isoflurane and sevoflurane have similar effects of hypotension with a dose dependent peripheral vasodilation and minimal effects on rhythm and contractility. The heart rate usually remains constant. A drug with less cardio-‐depressant effects may be administered as a CRI during the maintenance phase to further reduce or even eliminate the dose of inhalant necessary for maintenance of a surgical plane. A CRI of an opioid, ketamine or a combination are often used in patients with severe disease to minimize the inhalant. In dogs, lidocaine may also be added for arrhythmia suppression. Fluids Most patients will require fluid support for maintenance of blood pressure. Ideally, a sodium restricted crystalloid fluid (0.45% NaCl/2.5% dextrose) should be used in the face of heart disease. The rate of fluid therapy however, is far more important than fluid type. The standard anesthetic fluid rate of 10 ml/kg/hr would likely result in fluid overload in patients with moderate disease. A general rate of 3-‐5 ml/kg/hr for patients with mild to moderate disease and 2-‐3 ml/kg/hr for patients with severe disease is recommended. Left atrial size is useful in determining fluid rate. Fluid rate is of lesser concern for those patients with strictly right sided heart disease. Extreme caution should be exercised with colloid administration. Ancillary Therapy A CRI of a positive inotropic or pressor drug is often necessary. However, positive inotropic therapy should be used with caution in patients with a pressure overload state (aortic/pulmonic stenosis) and those with diastolic dysfunction. Dobutamine directly increases myocardial contractility and heart rate with a subsequent increase in cardiac output and blood pressure. Dobutamine triggers a mild vasodilation thereby decreasing ventricular afterload. Patients with diminished contractility are generally started on a CRI (5-‐15 mcg/kg/min) prior to induction. The dose is adjusted based on blood pressure and heart rate. Dobutamine is arrhythmogenic and may result in significant tachycardia especially at higher dosing. May trigger seizures in cats. Dopamine is also commonly administered as a CRI for pressor support. Dopamine triggers vasoconstriction at higher doses increasing ventricular afterload and mitral regurgitation. Specific Heart Diseases Mitral Valve Disease The predominate concern in patients with mitral valve disease is minimizing vasoconstriction. In small breeds contractility is generally well preserved, however marked deterioration of ventricular contractility is common in large breeds of dogs. Vasoconstriction increases the afterload to the left ventricle with a subsequent increase in mitral regurgitation and potential development of pulmonary edema and arrhythmias. Vasodilation and increasing contractility will directly reduce mitral regurgitation. Low dose acepromazine may be used to decrease mitral regurgitation. Include opioids for reduction of inhalant drug concentrations with the choice of opioid determined by level of expected pain. Etomidate, profol or ketamine/diazepam are all suitable induction drugs. Isoflurane or sevoflurane are appropriate for maintenance, and vasodilatory effects of the inhalants will further reduce mitral regurgitation. Dilated Cardiomyopathy (DCM) The predominate feature of DCM is severe myocardial contractile dysfunction with subsequent chamber dilation, congestive heart failure and arrhythmias. Atrial fibrillation is quite common in all affected breeds. Fatal ventricular arrhythmias are common in Dobermans and Boxer dogs. Areas of concern include maintaining contractility and prevention of arrhythmias. Intotropic support should be addressed throughout the anesthetic period. Propofol should be avoided due to its myocardial depressant effects. Induction with etomidate, ketamine/diazepam or fentanyl is recommended. A CRI of lidocaine is recommended for dogs with ventricular arrhythmias. Lidocaine may be combined with morphine/ketamine or fentanyl CRI for additional reduction of inhalant concentration. Hypertrophic Cardiomyopathy The predominate feature of HCM is diastolic dysfunction secondary to decreased myocardial relaxation and ventricular compliance. Ventricular systolic function is generally normal to enhanced. Perfusion abnormalities are common secondary to increased wall thickness and coronary artery abnormalities. The main area of concern is preventing tachycardia. Increasing the heart rate diminishes diastolic filling with a subsequent increase in atrial pressures and development of heart failure. Myocardial perfusion is also reduced with an increase in myocardial metabolism. The anesthetist should avoid medications that may increase heart rate including anticholinergics and ketamine. Congenital Heart Disease Congenital heart diseases predominately affect the heart in one of two ways, volume overload secondary to shunting (septal defect, patent ductus arteriosus) or a pressure overload secondary to a stenotic valve/artery (aortic and pulmonic stenosis). Diseases resulting in a volume overload should be handled within a similar manner as mitral valve disease. Systemic vasodilation is also beneficial for left to right shunting as it reduces the pressure gradient and subsequently the amount of shunting through the defect. Generally, contractility is preserved in patients with a left to right shunt. Patients with a right to left shunt either have severe pulmonary hypertension or pulmonic stenosis and an ASA classification of 4 or 5. The predominate concern with a pressure overload is a limited ability to compensate for vasodilation due to a restricted cardiac output. Patients with severe wall thickening will likely have diastolic dysfunction and myocardial perfusion abnormalities similar to HCM. Contractility is generally normal except in patients with advanced disease. Patients with a pressure overload should be managed similar to HCM with careful attention in maintaining heart rate and limiting vasodilation. The development of left sided congestive heart failure is rare with aortic stenosis, and hence a larger rate of fluid administration is generally safe as long as the left atrium is of normal size.