* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Background Information
Survey
Document related concepts
Management of acute coronary syndrome wikipedia , lookup
Heart failure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Coronary artery disease wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Transcript
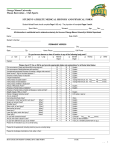
A Noninvasive, Hand-Held Device for Assessing Left Ventricular End-Diastolic Pressure Based on Finger Photoplethysmography and the Valsalva Maneuver Panagis Galiatsatos, MD Johns Hopkins Bayview Medical Center February 2nd 2013 No Disclosures Outline • • • • • • Background information Objective of the study Methods Results Conclusions Future Direction Background Information • Knowledge of left ventricular filling pressure useful in certain clinical settings. • Non-invasive tools: – Physical Exam – Chest X-ray – Daily weights – Bloodwork (pro-BNP) Background Information Valsalva Maneuver - Created by Antonio Maria Valsalva - Effects on the cardiovascular system Background Information Valsalva Maneuver Phase 1: Initial blood pressure increase Phase 2: Maintaining the strain – decrease in pressure Phase 3: Release of the strain – short decrease of arterial pressure Phase 4: Distinct overshoot of pressure “Sinusoidal Response” Background Information Valsalva Maneuver Bedside technique with sphygmomanometry Issue 1. No standardization of technique 2. Does not yield continuous measure Background Information “Finger photoplethysmography during the Valsalva maneuver reflects left ventricular filling pressure” Silber HA et al. Am J Physiol Heart Circ Physiol 2012 Photoplethysmograph (PPG) Pulse Amplitude Ratio (PAR) Objective Validate a new hand-held, batterypowered device that inputs finger PPG and expiratory pressure signals during the Valsalva maneuver, guides subject performance and calculates PAR automatically. / pressure A Mouthpiece transducer B Photoplethysmography (PPG) probe C A C User-friendly display B Methods Patients who were scheduled to undergo a cardiac catheterization including the measurement of LVEDP. Expiratory pressure during Valsalva was measured by having the subject place a tube in their mouth that was connected to a pressure transducer input into the device. Methods The subject was coached to keep the expiratory effort at about 20 mmHg during a 10-second Valsalva maneuver. The output measure of the device is the ratio of the amplitude of the PPG waveform near the end of Valsalva to the amplitude at baseline Methods Results All Patients Characteristics (N=14) + SD Age Female BMI (kg/m2) Co-Morbidities 53 + 8.5 7 (50%) 33.1 + 7.6 Hypertension (n) Hemodialysis (n) Diabetes mellitus (n) Coronary Artery Disease (n) 7 (50%) 2 (14%) 4 (29%) 8 (57%) Calcium channel blockers (n) Beta blockers (n) Thiazide diuretics (n) ACE-I / ARB (n) Loop diuretics (n) 1 (7%) 9 (64%) 1 (7%) 9 (64%) 1 (7%) Medications PAR > 0.72 was 78% sensitive and 100% specific in identifying LVEDP > 15 mmHg. Conclusions • This study represents initial testing of a handheld, battery-powered device using finger PPG during the Valsalva maneuver for assessing left ventricular filling pressure noninvasively. • The output measure of the device, Pulse Amplitude Ratio (PAR), correlated well with LVEDP obtained invasively by cardiac catheterization. Conclusions • PAR > 0.72 was 78% sensitive and 100% specific in identifying LVEDP > 15 mmHg, a clinically meaningful cutoff value in heart failure. • Further testing is warranted to explore the clinical utility of this device in heart failure management and other settings. Future Directions • Use of the device to assess adequate fluid removal from in-patient diuresis in heart failure patients. • PAR in the use of fluid removal in hemodialysis. Acknowledgements • Harry Silber, MD, PhD – Principal Investigator • Jennifer Monti, MD, MPH • Interventional Cardiologists – David Bush, MD – Jeffrey C. Trost, MD – Peter Johnston, MD • Colleen Christmas, MD Questions