* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Neuromuscular Blockers
Survey
Document related concepts
Pharmacogenomics wikipedia , lookup
History of general anesthesia wikipedia , lookup
Discovery and development of angiotensin receptor blockers wikipedia , lookup
Drug interaction wikipedia , lookup
Neuropharmacology wikipedia , lookup
Psychopharmacology wikipedia , lookup
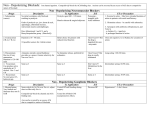
Transcript
Neuromuscular Blocking Agents • Dr. Ahmed Haki Ismael Neuromuscular Blockers • Competitive Antagonists of the Nicotinic Receptor e.g. curare (d-tubocurarine), vecuronium, pancuronium, atracurium, etc… • Depolarizing Blockers e.g. succinylcholine, decamethonium Key Concepts •Muscle relaxation does not ensure unconsciousness, amnesia, or analgesia •Neuromuscular blocking agents are used to improve conditions for tracheal intubation, to provide immobility during surgery, and to facilitate mechanical ventilation. •Depolarizing muscle relaxants act as acetylcholine (ACh) receptor agonists, whereas nondepolarizing muscle relaxants function as competitive antagonists. •Depolarizing muscle relaxants are not metabolized by acetylcholinesterase, they diffuse away from the neuromuscular junction and are hydrolyzed in the plasma and liver by another enzyme, pseudocholinesterase (nonspecific cholinesterase, plasma cholinesterase, or butyrylcholinesterase). •With the exception of mivacurium, nondepolarizing agents are not significantly metabolized by either acetylcholinesterase or pseudocholinesterase. Reversal of their blockade depends on redistribution, gradual metabolism, and excretion of the relaxant by the body, or administration of specific reversal agents (eg, cholinesterase inhibitors) that inhibit acetylcholinesterase enzyme activity. •Compared with patients with low enzyme levels or heterozygous atypical enzyme in whom blockade duration is doubled or tripled, patients with homozygous atypical enzyme will have a very long blockade (eg, 4–6 h) following succinylcholine administration. •Succinylcholine is considered contraindicated in the routine management of children and adolescents because of the risk of hyperkalemia, rhabdomyolysis, and cardiac arrest in children with undiagnosed myopathies •Normal muscle releases enough potassium during succinylcholine-induced depolarization to raise serum potassium by 0.5 mEq/L. Although this is usually insignificant in patients with normal baseline potassium levels, a life-threatening potassium elevation is possible in patients with burn injury, massive trauma, neurological disorders, and several other conditions •Doxacurium, pancuronium, vecuronium, and pipecuronium are partially excreted by the kidneys, and their action is prolonged in patients with renal failure. •Atracurium and cisatracurium undergo degradation in plasma at physiological pH and temperature by organ-independent Hofmann elimination. The resulting metabolites (a monoquaternary acrylate and laudanosine) have no intrinsic neuromuscular blocking effects •Hypertension and tachycardia may occur in patients given pancuronium. These cardiovascular effects are caused by the combination of vagal blockade and catecholamine release from adrenergic nerve endings •Long-term administration of vecuronium to patients in intensive care units has resulted in prolonged neuromuscular blockade (up to several days), possibly from accumulation of its active 3-hydroxy metabolite, changing drug clearance, or the development of a polyneuropathy •Rocuronium (0.9–1.2 mg/kg) has an onset of action that approaches succinylcholine (60–90 s), making it a suitable alternative for rapid-sequence inductions, but at the cost of a much longer duration of action. www.freelivedoctor.com Decamethonium Depolarizing Blockers Succinylcholine Vecuronium Competitive Blockers D-tubocurarine pancuronium History of neuromuscular blocking agents • Early 1800’s – curare discovered in use by South American Indians as arrow poison • 1932 – West employed curare in patients with tetanus and spastic disorders • 1942 – curare used for muscular relaxation in general anesthesia • 1949 – gallamine discovered as a substitute for curare • 1964 – more potent drug pancuronium synthesized Curares - Chondrodendron e Strychnos Strychnos toxifera West 1932 Milestones of Neuromuscular Blockade in Anesthesia • • • • • • • • • • 1942 introduction of dTc in anesthesia 1949 Succinylcholine, gallamine metocurine introduced 1958 Monitoring of NMF with nerve stimulators 1968 Pancuronium 1971 introduction of TOF 1982 Vecuronium,Pipecurium,atracurium 1992 Mivacurium 1994 Rocuronium 1996 Cisatracurium 2000 Rapacurium introduced and removed Neuromuscular blockers differ from each other in: • • • • • Mechanism of action Duration of action Speed of onset and offset of action Selectivity of action and safety margin Adverse effects Classification of Blockers Agent Pharmacological Properties Succinylcholine Ultrashort acting; Depolarizing Onset time Duration (min) (min) 1-1.5 6-8 Elimination Plasma cholinesterase D-tubocurarine Long duration; Competitive 4-6 80-120 Renal and liver Atracurium Intermediate duration; Competitive 2-4 30-40 Plasma cholinesterase Mivacurium Short duration; Competitive 2-4 12-18 Plasma cholinesterase Pancuronium Long duration; Competitive 4-6 4-6 Renal and liver Rocuronium Intermediate duration; competitive 1-2 1-2 Renal and liver Site of Action of d-Tubocurarine Nerve AP Muscle AP Left Leg Muscle Stimulation Right Leg Nerve Stimulation Right Leg Muscle Stimulation Non-depolarizing Block G: gallamine; TC: tubocurarine; NEO: neostigmine; S: succinylcholine. Depolarizing Block C10: TC: NEO: S: decamethonium tubocurarine neostigmine succinylcholine Comparison of Competitive and Depolarizing Blocking Agents Competitive Depolarizing Effect of previous dtubocurarine Additive Effect of previous decamethonium None/antagonistic May be additive Efect of cholinesterase inhibitors Reverse Effect on motor end plate Elevated Partial, persisting threshold to Ach; depolarization no depolarization Initial excitatory effect None Effect of KCl or tetatnus Transient on block reversal Antagonistic No antagonism Transient fasciculations No antagonism Dual Block by Depolarizing Agents NEO reversed the blockade by C10. C10: decamethonium; NEO: neostigmine; TC: tubocurarine Changing Nature of Neuromuscular Blockade Depolarizing Blocker Competitive Blocker Competitive Blockade Noncompetitive Blockade (desensitization) (electrogenic Na pump) (direct channel block) Sequence of Paralysis Fingers, orbit (small muscles) limbs Diaphragm Trunk neck Intercostals Recovery in Reverse Other Effects of Neuromuscular Blockers • Action at Autonomic Ganglia e.g. d-tubocurarine blocks, succinylcholine may stimulate newer agents have less ganglionic effects • Histamine Release e.g. d-tubocurarine bronchospasm, bronchial and salivary secretions Adverse Effects/Toxicity • Hypotension • Decreased tone and motility in GI tract • Depolarizing agents can cause increased K efflux in patients with burns, trauma, or denervation and lead to hyperkalemia • Prolonged apnea (many reasons, check for pseudochlinesterase genetic polymorphism) • Malignant hyperthermia (succinylcholine + halothane especially) • Sinus bradycardia/junctional rhythm (with succinylcholine) % Change in Systolic BP with d-Tubocurarine as a Function of Dose and Depth of Anesthesia Increasing Dose of d-tubocurarine 6 mg/m2 12 mg/m2 18 mg/m2 Systolic BP Increasing Depth (% Halothane) 0.25% 0.5% 0.75% Systolic BP Influence of Type of Anesthetic on Enhancement of Neuromuscular Blockade By d-Tubocurarine www.freelivedoctor.com Hemodynamic Effects of d-Tubocurarine and Pancuronium HR SVR CO MAP Drug Interactions • Cholinesterase Inhibitors (antagonize competitive and enhance depolarizing) • Inhalational Anesthetics (synergistic) • Aminoglycoside Antibiotics (synergistic) • Calcium Channel Blockers (synergistic) Therapeutic Uses • Adjuvant in surgical anesthesia • Orthopedic procedures for alignment of fractures • To facilitate intubations – use one with a short duration of action • In electroshock treatment of psychiatric disorders