* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download duodenum
Survey
Document related concepts
Transcript
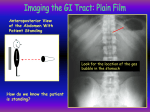
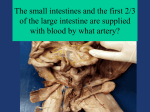
ABDOMEN Ⅳ [email protected] Objects 1 2 3 • Go over the stomach and the liver • The arteries and ligaments of stomach and liver • Bile circulation • Pancreas • Small intestine • Large intestine • •Dissection Greater omentum & Lesser omentum Hepatogastric ligament Hepatoduodenal ligament Gastrophrenic ligament Gastrosplenic ligament Gastrocolic ligament Visceral surface of liver left lobe right lobe caudate lobe quadrate lobe Caudate lobe left lobe Quadrate lobe Right lobe 4 Liver Porta hepatis 5 cm long, transversely across the “H”, ★ transverse fissure -- – Contents • Right and left hepatic ducts • Left and right branches of proper hepatic artery • Left and right branches of hepatic portal vein • Nerves and lymphatic vessels – These structures are surrounded by connective tissue and is called “hepatic pedicle” 4 types vessels of liver • Blood supply of liver: 1. proper hepatic artery( ← hepatic A← celiac trunk ← aorta) 2. hepatic portal vein A dual BLOOD supply: the portal vein supply for75%(dominant) , The arterial supply account for 25%(lesser) 1. Proper hepatic artery Celiac trunk → common hepatic A →proper hepatic A → right & left branches → 2. Hepatic portal vein General features • the union of superior mesenteric vein SMV and splenic vein • passing through the lesser omentum to the porta hepatis, divides into right and left branches • Has no valves in hepatic portal system • Drains blood from GI tract(capillaries) to hepatic sinusoid(capillaries) : the lower end of esophagus to the upper end of anal canal, pancreas, gall bladder, bile ducts and spleen 2. Hepatic portal vein Tributaries of hepatic portal v. 1. Superior mesenteric v. SMV 2. Inferior mesenteric v. IMV 3. Splenic v. 4. Left gastric v. 5. Right gastric v. 6. Cystic v. 7. Paraumbilical v. Portal- Caval venous anastomoses 1. Site at the esophagus left gastric vein → esophageal venous plexus → esophageal vein → hemiazygos vein → superior vena cava Esophageal varices,---bleeding 2. At rectum splenic vein → inferior mesenteric vein → superior rectal vein → rectal venous plexus → inferior rectal and anal veins → internal iliac vein → inferior vena cava • Hemorroid --- Hemorrage Portal hypertension Portal- Caval venous anastomoses 3. At paraumbilical venous rete paraumbilical vein→periumbilical venous rete→ thoracoepigastric and superior epigastric vein →intercostal vein--superior vena cava Caput medusa 4.retroperitoneal anastomosis the retroperitoneal branches of the colic veins pancreaticoduodenal veins -----the lumbar veins, twigs of colic veins (portal) anastomosing with systemic retroperitoneal veins Intestinal bleeding pancreaticoduodenal veins 3 Intrahepatic bile duct 4 hepatic veins The segments of the liver – bases upon the principal divisions of the proper hepatic artery and accompanying hepatic ducts and hepatic portal vein- “Glisson system” . – The hepatic vein do not follow the same pattern and vary: their main tributaries run rather intersegmental. Couinaud segments 8 by controversial ★ Biliary duct and gallbladder • ★ Consists of – – – – Gallbladder, Left and right hepatic ducts Common hepatic duct Common bile duct Enters the wall of descending part of duodenum obliquely where joins the main pancreatic duct to form the hepatopancreatic ampulla • Opens at the major duodenal papilla ★ Gallbladder • ★ Position – Lies in fossa for gallbladder on visceral surface of liver • ★ Four parts 1. Fundus of gallbladder protrude below the inferior margin of the liver, behind the point where the lateral margin of the right rectus abdominis meets the costal arch (Murphy’ point) 2.Body of gallbladder 3.Neck of gallbladder 4. Cystic duct • Function: stores and concentrates bile ★ Biliary duct system • Left and right hepatic ducts unite outside of liver to form common hepatic duct • common hepatic duct • Cystic duct joins common hepatic duct to form common bile duct ★ Biliary duct system • Hepatopancreatic ampulla (Vater) – Common bile duct and pancreatic duct run obliquely through the wall of the descending part of duodenum ,unite to form the hepatopancreatic ampulla --- rounded by sphincter of hepatopancreatic ampulla (Oddi), has sphincteric muscle for regulating flow, opens at the major duodenal papilla Obstruction of the biliary system results in the clinic condition of jaundice (yellow skin) . Cystohepatic triangle Calot’s Triangle • Boundaries – Common hepatic duct on the left – Cystic duct on the right – Liver superiorly • Content: cystic artery Divisions of common bile duct Divisions 4 • • • • Supraduodenal segment Retroduodenal segment Pancreatic segment Intraduodenal segment • Hepatogastric ligament • Hepatoduodenal ligament ★ Bile circulation Bile is secreted by the liver cells Common hepatic duct Right and left hepatic ducts Biliary ductuli Gallbladder (store, concentrate) Cystic duct When fat enters small intestine, gallbladder contracts, sphincter of hepatopancreatic ampulla relax Common bile duct Main Pancreatic duct the hepatopancreatic ampulla Major duodenal papilla Duodenal cavity Magnetic resonance cholangiopancreatography. Pancreas • Function – The pancreas is both an exocrine and an endocrine gland – The exocrine portion of the gland produces a secretion that contains enzymes that are capable of hydrolyzing proteins, fats, and carbohydrates – The endocrine portion of the gland, the pancreatic islet, produces the hormones insulin and glucagons , play a key role in carbohydrate metabolism Pancreas • Shape – A soft yellowish gland • Position – Lies in epigastric and left hypochondriac regions, behind the peritoneum on the posterior abdominal wall, roughly at the level of of L1~L2 Pancreas • Four parts – Head--Lies within the C-shaped curvature of duodenum. • Uncinate process A projection to the left from the lower part of the head behind the superior mesenteric vessels. – Neck--narrow part, overlies the superior mesenteric vessels and beginning of the portal vein – Body--triangular in cross section, passes upward ang to the left across the midline – Tail--extends to the hilum of spleen in the splenorenal ligament Pancreas • Pancreatic duct – Main Pancreatic duct • Begins at tail and throughout gland • Joins common bile duct before entering descending part of duodenum at major duodenal papilla – Accessory pancreatic duct • When present, drains head of pancreas separately • Opens 2cm above main duct at lesser duodenal papilla Blood supply of pancreas Arteries 1.Mainly from splenic A 2.Superior pancreaticoduodenal a.(from gastroduodenal A) – Inferior pancreaticoduodenal a.(from SMA) Veins- draining into superior mesenteric and splenic veins –potal vein. CT scan of pancreas. spleen • lies posterolaterally against the diaphragm and ribs 9 to 11 on the left side of the body. • Usually it is palpable only when enlarged. • Diaphragmatic surface • Visceral surface – Anteriorly-fundus of stomach – Posteriorly-left suprarenal gland and kidney – Inferiorly-tail of pancreas and left colic flexure Ligaments of spleen 1.Gastrosplenic ligament -connects the fundus of stomach to hilum of spleen. the short gastric and left gastroepiploic vessels pass through it. 2. Splenorenal ligament -extends between the hilum of spleen and left kidney. The splenic artery and vein pass through it 3. Phrenicosplenic ligament 4. Splenocolic ligament The Small Intestine • About 6m long, • Divided into – Duodenum – Jejunum – Ileum Duodenum 1. The major part of chemical digestion , extends from the pylorus to the Ileum ileocecal junction . Proteins are broken down into small peptides and amino acids before absorption. 2. permanent circular folds and villi ( villus ) for absorption .Each villus has a network of capillaries (amino acids and carbohydrates)and fine lymphatic vessels called lacteals (lipids)close to its surface. jejunum duodenum Features: 1. 25cm long,the widest and fixed part of small intestine. 2. Pursue a C-shaped course around the head of pancreas. 3. 4 parts Four parts Duodenum 1.Superior part 5cm, L1 vertebrae Superior duodenal flexure 2.Descending part 7~10cm, L2~3 3. Horizontal part 6~8cm,L3 to the left 4. Ascending part – – duodenojejunal flexure Ligament of tretz duodenum 1.superior part Quadrate lobe of live Gallbladder Duodenal cap (radiography ) The beginning 2cm,intraperitoneal,mobile Site of duodenal ulcer duodenum 2. descending part 1.Major duodenal papilla(opening) hepatopancreatic ampulla (Vater ampulla)--united of the bile and pancreatic ducts 2.Minor duodenal papilla duodenum 3.horizontal part • Anteriorly – Root of mesentery – Superior mesenteric a. and v. duodenum ascending part • Right — Head of pancreas and abdominal aorta • Left — left kidney and ureter Suspensory muscle of duodenum (ligament of Treitz) composed of a skeletal muscle from diaphragm , and a fibromuscular band of smooth muscle from the duodenum. a surgical landmark, descends from the right crus of diaphragm to duodenal termination. Blood supply of duodenum • Arteries – Superior pancreaticoduodenal a. – Inferior pancreaticoduodenal a. • Veins-follow arteries, draining directly into superior mesenteric and hepatic portal veins • Lymph drainadge follow the arteries to celiac LN • Nerve innervation: superior mensenteric plexus celiac plex Jejunum and ilium The jejunum and ileum lies free in the abdomen. They are attached to the posterior abdominal wall by the mesentery . Intraperitoneal organ 42 Jejunum and ileum jejunum is shorter , emptier, more vascular (redder in vivo), more thickly walled . Jejunum and ileum Characteristic Jejunum Ileum Position Upper 2/5 Lower 3/5 caliber 2~4cm 2~3cm Wall Thicker and heavy Thin and light Circular folds Large, tall and large villi low,sparse, less abundant villi Vascularity Greater Less Colour Deeper red Paler vasas recta Arcades Fat in mensentery Long A few large loops less Short Many short loops more 44 Mesentery The mensentery - suspends the small intestine from the posterior abdominal wall -Broad and a fan-shaped; arteries and veins between the two layers of peritoneum • Root of mesentery – 15 cm long – Directly obliquely run from left side of L2 vertebra to right sacroiliac joint Middle colic a. Inf. pancreaticodudenal a. Right colic a. Ileocolic a. Appendicular a. Blood supply of small intestine-------SMA Superior Mesenteric v. Superior mesenteric a. Jejunal and ileal a. large intestine • Approximately 1.5m long, • Five parts: – Cecum – Vermiform appendix – Colon – Rectum – Anal Canal Function: absorb excess water,compact chyme into semisolid stool; store and accumulate until defecation 47 Features: Distinguished from small intestine by: 1.Teniae coli: 3 thickened longitudinal bands of smooth muscles, begin at the base of appendix,at rectosigmoid junction emerge with each other 2.haustra : sacculations of wall of the colon between the teniae 3. Omental appendices: small ,fatty, projections haustra of colon Teniae coli omental appendices 48 Hepatorenal recess Paracolic gutters are formed by the ascending and descending colons 1.beginning of large intestine, (一)Cecum 2.Blind intestinal pouch, 7.5*7.5cm 3. Lies in right iliac fossa. 4.Free and has no mensentery --- mobile cecum The ileum enters the cecum obliquely, and partly invaginates into it, forming the ileocecal valve-consists of two folds. ileocecal valve 50 The cecum Intussusception: invagination of a tubular organ or part, the telescoping of one section of the intestinal tract into a lower section, causing obstruction Human Anatomy 51 Appendix 1. a blind intestinal diverticulum, 2~20cm 2. mesoappendix: triangular mesentery 3.the base of appendix : Lies deep to a point that 1/3 of the way along the oblique line joining the right anterior superior iliac spine to the umbilicus .(Mcburney’s point) The base of the appendix lies at the point of convergence of three teniae coli 52 (二)vermiform appendix position: very variable in position, frequently lies in the retrocecal recess or extend into the lesser pelvis. Appendicitis: acute inflammation of appendix, shows abdominal pain, nausea,abdominal rigidity appendectomy appendicular perforation orifice appendix 53 colon 1、ascending colon 2、transverse colon 3、descending colon 4、sigmoid colon right colic flexure(hepatic) left colic flexure(splenic) 54 Inferior mesenteric v. Inferior mesenteric a. Left colic a. Sigmoid a. Superior rectal a. Blood supply of large intestine-----IMA Celiac trunk----- supplies the foregut SMA----supplies the midgut IMA--- hindgut Marginal artery----the first arcades of a series of anastomic arcades is continued by the ileocolic, right, middle, left and sigmoid colic arteries ,form a continuous arterial channel, so-called~ ;parallel and extends the length of the colon Sigmoid colon volvulus an abnormal twisting of the intestines causing obstruction Human Anatomy 58 The rectum 1. the pelvic part of digestive tract, at S3 vertebra 2. Not straight: lateral view “S” shape sacral flexure of the rectum anorectal flexure:(for fecal continence) Human Anatomy •Rectum Blood supply 61 anal canal 1.Teminal part of large intestine, 3 cm long, ends to anus 2.Surrounded by internal and external anal sphincters internal : involuntary sphincter, surrounding superior 2/3 external: large voluntary sphincter, forms a broad band on each side of the inferior 2/3; has subcutaneous , superficial and deep parts fecal incontinence Human Anatomy 62 Anal canal 1. Internal structure 1) anal columns ) anal valves anal sinuses 2) pectinate line pile (hemorrhoid) [examination per anus ] Human Anatomy 63 64 Coronary section through rectum 65 66 67 Name the structures 9 6 1 7 2 3 4 8 5 10