* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download File
Orphan drug wikipedia , lookup
Discovery and development of neuraminidase inhibitors wikipedia , lookup
Discovery and development of non-nucleoside reverse-transcriptase inhibitors wikipedia , lookup
Drug design wikipedia , lookup
Neuropharmacology wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Psychopharmacology wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Discovery and development of ACE inhibitors wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Prescription costs wikipedia , lookup
Drug discovery wikipedia , lookup
Pharmacognosy wikipedia , lookup
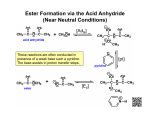
Phase II or Conjugation Reactions – Conjugation reactions link an endogenous moiety (an endocon) to the original drug (if polar functions are already present) or to the Phase I metabolite. They are catalyzed by enzymes known as transeferases. They involve a cofactor which binds to the enzyme in the close proximity of the substrate and carries the endogenous molecule or moiety to be transferred. Except for methylations and acetylations, this endocon is highly polar and its size is comparable to that of the substrate. Phase II Reactions Include: 1. Glucuronidation 2. Sulfate Conjugation 3. Acetylation 4. Amino Acids (GLYCINE) Conjugation 5. Methylation 6. Glutathione Conjugation 1. Glucuronidation The mechanism of glucuronidation is one of nucleophilic substitution with inversion of configuration, -D-glucuronic acid in UDPGA forming -D-glucuronides. OH gluconic acid OH COOH OH OH HO OH O OH COOH OH HO glucose O OH OH OH HO glucuronic acid OH Glucuronidation Pathway and Enterohepatic Recirculation The functional groups able to undergo glucuronidation are classified as O-, N-, S- and C-glucuronides. • O-Glucuronidation includes phenolic xenobiotics or metabolites generally at high doses (O-sulfation is predominating at low doses). OH R O GLU R GLU = glucuronic acid – Alcohols are another major substrates, may primary, secondary or tertiary ones. Estriol glucuronide An interesting example is that of morphine, which is conjugated on its phenolic and secondary alcohol groups to form the 3-O-glucuronide and the 6-Oglucuronide respectively. N CH 3 N 1 1 3 3 ULG O CH 3 O 3-O-glucuronide 6 OH HO O 6-O-glucuronide 6 O GLU The second important after O-Glucuronides are the N-glucuronides formed from carboxamides, sulfonamides, and various amines. N-Glucuronidation of aromatic and aliphatic amines in addition to pyridine-type nitrogens has been observed in only a R1 few cases. R1 N H R2 O O R1 S N H R1 N GLU R2 O O R1 S N GLU R2 R2 R1 N CH3 CH3 N R2 R2 GLU R R N N GLU S-Glucuronides are formed from aliphatic thiols, aromatic thiols and dithiocarboxylic acids. R SH R S GLU C-Glucuronidation is seen in humans for 1,3-dicarbonyl drugs such as sulfinpyrazone . C6H5 C6H5 N O C6H5 N N O H C6H5 HOOC CH2CH 2SC6H5 O O O HO HO OH N O CH2CH 2SC6H5 O Beside xenobiotics, a number of endogenous substrates, notably bilirubin and steroids are eliminated as glucuronide conjugates. In neonates and children, glucuronidation processes often are not fully developed. In such subjects, drugs and endogenous compounds (e.g. bilirubin) that are normally metabolized by glucuronidation may accumulate and cause serious toxicity. For example, neonatal hyperbilirubinemia and gray baby syndrome, result from accumulation of toxic levels of the free chloramphenicol. 2. Sulfate conjugation In reactions of sulfoconjugation, a sulfate molecule is transferred from the cofactor (3’phosphoadenosine 5’-phosphosulfate, PAPS) to the substrate by cytosolic enzymes known as sulfotransferases. NH2 N N R X H N O HO O2 S O P O O O N R X SO3H N + O HO OH H NH2 P N O O OH O P OH H OH OH O O P OH OH OH N N Phenols compose the main group of substrates undergoing sulfate conjugation. Thus, drugs containing phenolic moieties often susceptible to sulfate formation. O O O NHCCH 3 NHCCH 3 NHCCH 3 + OH OC6H9O6 O-Glucuronide Conjugate OSO3O-Sulfate conjugate The sulfate conjugation of N-hydroxylamines and N-hydroxyamides takes place occasionally as well. O-Sulfate conjugates of N-hydroxy compounds are of considerable toxicologic concern because they can lead to reactive intermediates that are responsible for cellular toxicity. O O O3SO HO NHCCH 3 N CCH 3 OC2H5 OC2H5 O - N CCH 3 OC2H5 3. Amino acid conjugation This is a major route for many xenobiotic acids, involving the formation of an amide bond between the xenobiotic acyl-CoA and the amino acid. O ATP PPi O OH CoASH AMP O AMP SCoA Amino acid N-acyltransferase H 2N CoASH O COOH C R N H H Amino acid conjugate COOH C R H Amino acid Glycine is the amino acid most frequently used for conjugation. The xenobiotic acids undergoing amino acid conjugation are mainly benzoic acids such as benzoic acid itself and salicylic acid, forming hippuric acid and salicyluric acid respectively. R R O O O OH Bnzoic acid, R=H Salicylic acid, R=OH NHCH2COH Hippuric acid, R=H Salicyluric acid, R=OH 4. Conjugation with glutathione (GSH) – Glutathione (GSH, -glutamylcysteinylglycine) is a thiol-containing tripeptide. – GSH conjugation is an important pathway by which chemical reactive electrophilic compounds are detoxified. – Many serious drug toxicities may be explainable also in terms of covalent interaction of metabolically generated electrophilic intermediates with cellular nucleophiles. – GSH protects vital cellular constituents against chemically reactive species by virtue of its nucleophilic sulfhydryl (SH) group. NH2 H N HS C C E S H H GSH S-Transferase N H COOH O C O C C O + Electrophilic substrate H N COOH H H E NH2 C COOH O N H COOH GSH Adduct or Conjugate GSH Amino acid (AA) Glutamyl Transpeptidase O Glutamyl AA C H3C NH E S C H CoASH C O OH Mercapturic Acid Derivative Acetyl CoA N-Acetylase E S NH2 C H Glycine E NH2 C H C C O OH S-Substituted Cysteine Derivative S Cysteinyl Glycinase O N H COOH Unlike other conjugative phase II reactions, GSH conjugation does not require the initial formation of an activated enzyme or substrate. –Two general mechanisms are known for the reaction of compounds with GSH: 1. Nucleophilic displacement at an electron-deficient carbon or heteroatom. GSH CH2 X SG R R = Alkyl, Aryl, Benzylic, Allylic X = Br, Cl, I, OSO3-, OSO2R, OPO(OR)2 CH2 R + HX 2- Nucleophilic addition to an electron-double bond. O- O C C C C C GSH C C Michael Addition + C O- O C C CH C SG SG Unsaturated system Glutathione Adducts – The major reactions of glutathione are summarized in the following scheme: OH H R O OH SG O SG H OH OH R1 H C C R2 R R1 C X X X C C H O SG CH2 R2 R X C R R C X R HNO2 ONO2 GSH R OSG SG R SG (X= halogen) R C SG X C X O C Cl X C R X X (X= CO-R2, CN, ...) X SG OH O GSSG R OH – In most instances, GSH conjugation regarded as a detoxifying pathway is – In a few cases, GSH conjugation has been implicated in causing toxicity e.g. 1,2-dichloroethane. Cl H2C CH2 Cl GSH Cl H2C CH2 Cellular S SG Macromolecule G S-(2-chloroethyl)glutathion Episulfonium ion Toxicity 5- Acetylation Reactions –The most common reactions are acetylations of xenobiotics containing a primary amino group. –The major reactions of N-acetylation summarized in the following scheme. NH2 NH-COCH3 R1 R1 N-CO-CH3 N-H R R R2 R2 R NH-NH2 R NH-NH-CO-CH3 NHOH NH-OCOCH3 R R OH N R COCH3 are O Ar NH 2 O CoA S R NH 2 R OH R + Acetyl transferase SH R O Ar N H O CH 3 CH 3 O O R N H CH 3 R S Examples: Procainamide, isoniazid, sulfanilimide, histamine N-acetyl transferase enzyme is found in many tissues, including liver CH 3 –Acetylation result in decreased water solubility. – Genetic differences exist in some animal species and in humans, where one distinguishes between slow and fast acetylators. – Examples of drugs exhibiting acetylation polymorphism is the antituberculosis drug isoniazid (INH) –The drugs metabolized by acetylation may become ineffective in fast acetylators and cause toxicity in slow acetylators.This liver toxicity may be attributed to the formation of chemically reactive acylating intermediates as shown in the following scheme: O NHNH2 O NHNHCOCH 3 O OH O Hydrolysis CH3CNHNH2 + N N N N-Oxidation Liver Damage Covalent Binding O O CH3C + CH3C Reactive intermediates Procainamide O Unchanged in Urine, 59% H2 N N H 24% Fast 17% Slow H N Unchanged in Urine, 85% N O 3% O NAPA N H N 1% 0.3% H N O O N H H N O H2 N N H H N Procainamide O H2 N N N H trace metabolite HO H N O N N H non-enzymatic O O N N H N Lupus? 6- Methylation Reactions Methylation is an important reaction in the biosynthesis of endogenous compounds such as adrenaline, and in the inactivation of biogenic amines such as catecholamines. Reactions of methylation imply the transfer of a methyl group from the onium-type cofactor Sadenosylmethionine (SAM) to the substrate by means of a methyltransferase H2N H2N CO2H H H N R X NH2 O O N N Methyltransferase R X CH3 OH N + HO HO NH2 S S H N N N H3C CO2H OH N • Methyltransferases having particular importance in the metabolism of foreign compounds include catechol-Omethyltransferase (COMT), phenol-O-methyltransferase and nonspecific N-methyltransferase and S-methyltransferase. • Examples of drugs undergoing methylation are given in the following scheme. SH OH HO 3 CH3 CH3 COOH HO NH2 NH2 N N Nicotine N N CH3 CH3 N CH3 N H 6-Mercaptopurine Norephedrine S(-)--Methyldopa N N FACTORS AFFECTING DRUG METABOLISM – Many factors may affect drug metabolism, these include: 1. AGE 2. DIET 3. STATE OF HEALTH 4. GENDER 5. GENETIC VARIATION 6. SPECIES VARIATION 7. SUBSTRATE COMPETITION 8. ENZYME INDUCTION 9. ROUTES OF DRUG ADMINISTRATION AGE Age – related differences in drug metabolism are generally quite apparent in newborn. Undeveloped or deficient oxidative and conjugative enzymes are chiefly responsible for the reduced capability. Examples: • Undeveloped glucuronidating processes in neonates and children are responsible for neonatal hyperbilirubinemia and gray baby syndrome as dissussed before. • The oxidative metabolism of tolbutamide is significantly lower in infants (t½ more than 40 hrs) compared with adults (t½ ~ 8 hrs). SPECIES VARIATION – The metabolism of many drugs and xenobiotics is often species dependent. Examples: HN OH O N H O S(-)-p-Hydroxyphenytoin (Man) OH HN O N H O Phenytoin HN O N H O R(+)-m-Hydroxyphenytoin (Dog) O Oxid. Oxid. deamination OH O Benzoic acid (Man, Rabbit, Guinea pig) NH2 Amphetamine Aromatic hydroxylation NH2 HO p-Hydroxyamphetamine (Rat) Phenylbutazone half-life is 3 h in rabbit, ~6 h in rat, guinea pig and dog and 3 days in humans. Other notable species differences include: – Dogs: deficient in N-acetyl transferase (cannot acetylate aromatic amines) – Guinea-pigs: deficient in sulfotransferase activity; no Nhydroxylation – Cats: poor UDPGlucuronosyltransferase activity (unable to glucuronidate phenols) – Rats: often very rapid metabolizers; CYP2C is the major family in the liver with significant gender differences – Cynomolgus monkeys: reported to have low CYP1A2 activity GENETIC VARIATION • Marked individual differences in the metabolism of several drugs exists in humans. • Many of these genetic or hereditary factors are responsible for the large differences seen in the rate of metabolism of these drugs. •Example: Isoniazid - N-acetyltransferase O NHNH2 O NHNHCOCH 3 O OH O Hydrolysis CH3CNHNH2 + N N N N-Oxidation Liver Damage Covalent Binding O O CH3C + CH3C Reactive intermediates • First line drug in the treatment of TB; normally given at a does of 5 mg/kg, max. 300 mg/day for period of 9 months. • Rapid and slow acetylators first seen in TB patients; t1/2 for fast is 70 min; t1/2 for slow is 180 min. • N-acetyltransferase (NAT2 isoform) is in liver, gut • Peripheral neuropathy (about 2% patients; higher doses produce effects in 10-20%) seen in slow acetylators. • Hepatotoxicity also seen, esp. in older patients. Genetic Polymorphisms in Drug Metabolizing Enzymes GENDER • Male Rats metabolize many drugs faster than females through oxidative pathways, glucuronide and GSH conjugation of certain substances, • In Humans this difference also existed, though very limited and usually clinically not important. • e.g.The clearance of benzodiazepines eliminated by metabolic conjugation is significantly smaller in women than in man. ENZYME INDUCTION • Certain drug substrates of CYP, upon repeated administration, “induce” or elevate the amounts of specific forms of the enzyme. • Induction results in accelerated metabolism of the drug inducer and any other drugs metabolized by the induced enzyme. Classic Enzyme Inducers • • • • • Chronic ethanol Phenobarbital Tobacco (benzo[a]pyrene) PCBs (Poly chlorinated biphenyls), dioxin (environmental) Glucocorticoids ENZYME INHIBITION • Some drugs are capable of inhibiting metabolizing enzymes. • This is usually only important if a patient on a stable drug regimen starts taking a second drug metabolized by the same enzyme. • Examples: cimetidine, ethanol Drugs that Inhibit Drug Metabolism by Forming Complexes with CYPs Amphetamine Cimetidine Dapsone 2,5-Dimethoxy-4methylamphetamine Diphenylhydramine Erythromycin Fenfluramine Itraconazole Ketoconazole Methadone Methamphetamin eNortriptyline SKF 525A Sulfanilamide Non-nitrogenous Substances that Effect Drug Metabolism by Forming Complexes with CYPs • Grapefruit juice - CYP 3A4 inhibitor; highly variable effects; unknown constituents • Isosafrole, safrole - CYP1A1, CYP1A2 inhibitor; found in root pear, perfume • Piperonyl butoxide & alcohol -CYP1A1, CYP1A2 inducer; insecticide constituent Effect of Grapefruit Juice on Felodipine Plasma Concentration Cl H CH 3 O 2 C CH 3 N H Cl CO 2 CH 3 CH 3 Cl 3A4 Cl CO 2 CH 3 CH 3 O 2 C CH 3 N CH 3 5mg tablet with juice without STATE OF HEALTH • • • • Liver disease Kidney disease Endocrine diseases Reduced blood flow Sample biotransformation problem H N O C OCH 3 CH3 N O O C C A. O OCH 3 CH3 H3C N O O B. C C cocaine OCH3 O C. O CH3 N O O C CH3 N OCH3 D. OH O C OCH 3 O A……………………………….. B………………………………... C………………………………… D…………………………………. C C CH3 O Optimising Pharmacokinetic Properties 7. Designing Prodrugs and Bioprecursors Prodrug is any compound that undergoes biotransformation prior to exhibiting its pharmacological effects. Prodrugs can be divided into two classes: 7.1. The Carrier-prodrugs : Result from a temporary linkage of the active molecule with a transport moiety that is frequently of lipophilic nature. Prodrugs to mask toxicity and side effects • Mask groups responsible for toxicity/side effects • Used when groups are important for activity Example: Aspirin for salicylic acid O OH H3C CO2H O CO2H Salicylic acid Aspirin • Analgesic, but causes stomach ulcers due to phenol group • • Phenol masked by ester Hydrolysed in body Drug Barrier to delivery of drug Pro-moiety Drug Barrier to delivery of drug Pro-moiety Drug Biotransformation Pro-moiety Non-toxic & rapidly excreted + + Drug Efficacy 7.1.1 Practical applications of carrier-prodrug design 1. Improvement of the lipophilicity OH O O O CH3 NH2 OH Esterase HO Cl Cl O CH3 NH2 + OH HO Epinephrine HCl Dipivefrin HCl O Pivalic acid Candoxatril for Candoxatrilat (protease inhibitor) OMe OMe O O H N HO O O Candoxatrilat • • O CO2H O Candoxatril 5-indanyl group Varying the ester varies the rate of hydrolysis Electron withdrawing groups increase rate of hydrolysis (e.g. 5-indanyl) • H N O Leaving group (5-indanol) is non toxic CO2H 2. Enhancement of water solubility Prodrugs to increase water solubility • • • Often used for i.v. drugs Allows higher concentration and smaller dose volume May decrease pain at site of injection Example: Succinate ester of chloramphenicol (antibiotic) HO O Succinate ester O O H H N H O2N O OH OH H H N Cl Cl Esterase H Cl Cl O OH O2N Chloramphenicol Prodrugs to increase water solubility Example: Phosphate ester of clindamycin (antibacterial) CH3CH2CH2 Me N H H O C Cl H C CH3 N C H O H HO OH H H SCH3 H • H OPO32- Less painful on injection Prodrugs to increase water solubility Example: Lysine ester of oestrone Me H NH2 H O H H H H2N O O Prodrug • • • • Me H2N H NH2 H H + O Lysine O OH HO Oestrone Lysine ester of oestrone is better absorbed orally than oestrone Increased water solubility prevents formation of fat globules in gut Better interaction with the gut wall Hydrolysis in blood releases oestrone and a non toxic amino acid 3. Prodrugs to prolong activity Add hydrophobic groups Increase the duration of Pharmacological effects Example: Hydrophobic esters of fluphenazine (antipsychotic) fatty ester N N (CH2)8CH3 O O H N CF3 S • • • • Given by intramuscular injection Concentrated in fatty tissue Slowly released into the blood supply Rapidly hydrolysed in the blood supply Mask polar groups • Reduces rate of excretion Example: Azathioprine for 6-mercaptopurine O2N N SH S N N Me N N N N N H N N H 6-Mercaptopurine Azathioprine (suppresses immune response) • Short lifetime - eliminated too quickly • • Slow conversion to 6-mercaptopurine Longer lifetime 4. Improvement of patient acceptance – Used to reduce solubility of foul tasting orally active drugs – Less soluble on tongue – Less revolting taste Example: Palmitate ester of chloramphenicol (antibiotic) OH NHCOCHCl2 O 2N CH CH CH2 O CO(CH2)14CH3 Palmitate ester O O H H N H O2N O OH OH H H N Cl Esterase Cl H Cl Cl O OH O2N Chloramphenicol 5. Prodrugs used to target drugs Example: Hexamine N N N N • • • • Stable and inactive at pH>5 Stable at blood pH Used for urinary infections where pH<5 Degrades at pH<5 to form formaldehyde (antibacterial agent) 6. Increased site-specificity. Two targeting possibilities can be considered: 6.1. Site-directed drug delivery OH CO2H H H O N DRUG (CH2)n O H H OH H Bile acids for liver specific targeting 6.2. Site-specific drug release HO NH2 HO2C O HO N N S NH N azoreductase Amino Salicylic acid + O HO2C O Sulfasalazine H2N N S NH O Sulfapyridine Chemical Delivery Systems: Pharmacologically inactive molecules that require several steps of chemical and/or enzymatic conversion to the active drug and enhance drug delivery to particular organs or sites. Example: Brain-specific chemical delivery system 7.2. The Bioprecursors : Result from a molecular modification of the active principle itself. This modification generates a new compound, able to be a substrate for the metabolizing enzymes (often, oxidation and reduction). The metabolite being the expected active principle. Example for bioprecursor design based on oxidative bioactivation is the cytotoxic agent cyclophosphamid. Cyclophosphoramide for phosphoramide mustard (anticancer agent) NH O Phosphoramidase Cl (liver) H2N HO N Cl P P O O N Cl Cl Cyclophosphoramide Phosphoramide mustard • • • Non toxic Orally active Alkylating agent Sulindac (NSAID) is a representative example for bioprecursor bioactivated by reduction. CO2H CO2H F F CH3 CH3 In vivo Reduction O S S CH3 CH3 Inactive Active Soft Drugs Biologically active, therapeutically useful chemical molecules (drugs) characterized by a predictable and controllable in vivo deactivation, after achieving the therapeutic objective, to nontoxic, inactive compounds. Soft Drugs Examples: O O Cl N O OH Acetylcholine Estrase + N HO OH O N Cl O Succinylcholine Chloride O Succinic acid Choline Chloride Cl Hard drugs: these can be defined as drugs that are biologically active and non metabolizable in vivo eg: enalaprilat, lisinopril, DDT Insecticide DDT chlorophenyl)ethane) (1,1,1-trichloro-2,2-bis(p-