* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Imaging of Stroke
Survey
Document related concepts
Transcript
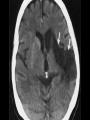
Imaging of Stroke Andrew Richards PPH Llanelli Medical interventions in ischaemic disease of the brain • • • • Primary prevention Secondary prevention Treatment of acute stroke Treatment of chronic stroke Imaging in secondary prevention • Extent of existing ischaemic disease in the brain and to exclude haemorrhage and other diseases • Extent of existing atherosclerotic disease in the head and neck vessels • To guide medical or surgical treatment CT (Angiography) • Advantages: Accessible, rapid acquisition and reconstruction, can image arteries and veins • Disadvantages: Requires iodinated contrast, limited by bone (e.g. skull base, shoulders), uses ionising radiation CT/CTA image interpretation and analysis • Overall accuracy of CT angiography (CTA) for detecting thromboses and stenoses of large intracranial and extracranial arteries is 95-99% • Comparable to conventional angiography for total and near total occlusion MRI/MRA • Advantages: Does not always require contrast agent, rapid acquisition, can image arteries or veins • Disadvantages: Inaccessible, limited by motion and artifact, implants (e.g. pacemaker) MRA Techniques • Time-of-flight (TOF) 2D and 3D techniques. Flow sensitive. Compliments U/S • Phase contrast (subtraction) method • Contrast MRA-similar to CTA, but overall accuracy slightly lower. Adequate diagnostic test before surgery Choice of technique (1) • Duplex ultrasonography (DUS)-requires institutional validation, QA and good neurological history • MRA combined with DUS similar to catheter angiography • CTA combined with DUS similar to catheter angiography Choice of technique (2) • DUS, MRA, CTA all similar (80% sensitivity, 90% specificity) • DUS operator dependent • MRA requires knowledge of technical limitations • All three combined gives overall accuracy at 94% (=catheter angiography) Imaging in the management of acute stroke • Potentially available techniques are CT and MRI • Exclusion of haemorrhage • Exclusion of other pathologies that may mimic acute stroke • Determination of the ischaemic penumbra (‘time is brain’) • Selection of patients for timely thrombolysis with rTPA NINDS Trial (1995) • Patients received intravenous thrombolysis within three hours of the onset of symptoms • Simple NECT used to exclude haemorrhage • Benefit at long term follow-up in treated group (partly offset by 10 fold increase in symptomatic haemorrhage) • rTPA subsequently received FDA approval for treatment of MCA stroke ECASS and ECASS II (1995, 1998) • Patients received intravenous thrombolysis within six hours of the onset of symptoms • Simple NECT used to exclude haemorrhage • No benefit to thrombolysis in either trial (ECASS II used lower dose of rTPA) • Better patient selection needed (no more than 1/3 of MCA territory to be affected by completed infarction) • Most patients need to be treated within three hours Non-enhanced CT (NECT) • Advantages: Accessible, rapid acquisition, high sensitivity for the detection of haemorrhage • Disadvantages: Less sensitive to hyperacute infarct than magnetic resonance diffusion weighted imaging Role of NECT • Exclude haemorrhage • Detect early signs of stroke • Exclude other causes Early signs of stroke on NECT • • • • Insular ribbon sign Lentiform nucleus obscured Subtle mass effect Hyperdense, occluded arteries (100% specific, 30% sensitive) MRI • Advantages: Diffusion weighted imaging (DWI) extremely sensitive to acute infarction, conventional sequences also useful • Disadvantages: Inaccessible, artifacts, implants Selecting patients for thrombolysis • Imaging of stroke pathophysiology required in the light of the evidence accrued • Available techniques are CT and/or MRI perfusion imaging • Both techniques based on indicatordilution method Cerebral blood volume (CBV) • Normal value is 4-5ml/100g • When reduced to <40% of normal, is likely to indicate irreversible cell death • Reflects completed infarct volume on CBV maps Cerebral blood flow (CBF) • Normal value is 50-60ml/100g/min • When reduced to <20% normal, is likely to indicate irreversible cell death • When area of reduced CBF is larger than area of reduced CBV on respective maps, is likely to indicate ischaemic penumbra or salvageable brain Indicator dilution method • Tight bolus injection of contrast agent • Wash-in, wash-out analysed continuously over time • Time-intensity curve generated Derived parameters from TIC • Mean transit time (MTT) and time to peak (TTP). Very sensitive to haemodynamic impairment • CBF and CBV. Absolute values are not accurate, but compared with normal, contralateral hemisphere. Better predict outcome of an ischaemic lesion • CBFxMTT=CBV CT Perfusion • Advantages: Widely available, rapid acquisition, accepted technique (FDA approved) • Disadvantages: Limited to MCA territory, bone artifacts, only semiquantitative, ionising radiation MR Perfusion imaging • Advantages: Covers entire brain, fast acquisition, can be performed with DWI • Disadvantages: Gadolinium contrast agents not licensed, semi-quantitative, limited access, patient motion, artifacts, implants (pacemakers) Summary • Imaging in secondary prevention here and now • Imaging in acute stroke requires investment (MRI unlikely to be available out-of-hours) • Evidence base for thrombolysis in acute stroke is thin • Only a small number of patients are likely to benefit from thrombolysis in acute stroke • An effective stroke thrombolysis service represents a significant challenge