* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Done By: Lara Mazahreh Advanced Technology Lecture#20 Last
Polysubstance dependence wikipedia , lookup
Orphan drug wikipedia , lookup
Discovery and development of proton pump inhibitors wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Psychopharmacology wikipedia , lookup
Tablet (pharmacy) wikipedia , lookup
Compounding wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Plateau principle wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Theralizumab wikipedia , lookup
Pharmacognosy wikipedia , lookup
Neuropharmacology wikipedia , lookup
Prescription costs wikipedia , lookup
Drug discovery wikipedia , lookup
Drug design wikipedia , lookup
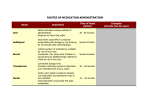
Done By: Lara Mazahreh Advanced Technology Lecture#20 Last lecture we discussed the concept of gastroretentive dosage forms, technologies to achieve the gastroretentive dosage forms, and we said that gastroretentive dosage forms are controlled release systems so that we have a system that is retained in the stomach and at the same time it's slowly releasing the drug in the aqueous gastric fluid "which undergoes rapid emptying". And we discussed that when we want to evaluate gastroretentive dosage forms, we evaluate certain parameters to know whether our drug is suitable to be used in gastroretentive dosage form or not. And the most important aspect is the 1- Absorption window of the drug; gastroretentive dosage forms are most valid for drugs with narrow absorption window. How to verify the absorption properties of the molecule? 1. Animal studies: Release the drug solution in specific areas of the GIT in animals, by incubation and study the permeability after releasing the drug into different segments of the GIT, For example, if we released the drug in our animal model in the stomach, we will get certain plasma concentration profile and extent of absorption (AUC). Then, if we released the drug after the pylorus, we won't find much difference in the AUC "absorption" of the drug, because the stomach isn't a very effective absorption area. But if we released the drug solution at the ileocecal junction “distance at the end of small intestine with the beginning of the large intestine” , we will notice significant reduction in the bioavailability which means that there's no significant absorption for the drug in the colon. If we released the drug in the ileum, and if there's reduction in the AUC that means the absorption occurs in the duodenum and not throughout the small intestine. 2. We can do clinical studies on cell lines to see what the mechanism of absorption is; either active transport or passive diffusion. Not all drugs with narrow absorption window are good candidates for gastroretentive dosage forms. For example, Metformin has a narrow absorption window, but at the same time it has a physicochemical property that allows it to naturally be retained in the proximal small intestine where it is absorbed. So we don't have to formulate it in gastroretentive form. 2- Whether there is advantage of enhanced bioavailability. For example, in riboflavin and levodopa, bioavailability will be enhanced by using those systems. But bisphosphonates are absorbed from stomach (small molecules and can permeate through the stomach membrane). We can do gastric retention in animal (rats) model, by surgical retention inside the stomach, to test whether we will get significant increase in the bioavailability or not. |Page1 Done By: Lara Mazahreh Advanced Technology Lecture#20 As conclusion, if you don’t get significant impact in terms of improvement of bioavailability, why you would go for? Especially the formulation of GR dosage forms is more complex than conventional forms in terms of development and evaluation. 3- If the drug is subject to first pass metabolism. By using gastroretentive dosage form, the drug is introduced to the liver in small amounts, less saturation to the receptors in the liver, so more drug will undergo first pass metabolism, which also will decrease the bioavailability. 4- If the absorption of the drug occurs in regions of proximal small intestine with low number of P-glycoprotein (P-gp), in this case the drug will reach that region gradually and absorption will occur without efflux. 5- Reduced frequency of dosing. All controlled release formulations reduce the frequency of dosing (either gastroretentive or non-gastroretentive). If the drug has short biological half-life, using gastroretentive formulations will result in the development of flip-flop kinetics (absorption rate constant<elimination rate constant and absorption half-life>elimination half-life), Gastroretentive formulation will reduce the value of absorption rate constant when the absorption is the rate limiting step, and will increase the biological half-life, And this will improve the patient compliance. (This is the result of the controlled release aspect of the formulation rather than gastroretentive aspect). Pharmacodynamic aspects of gastroretentive formulations: 1. Reduced fluctuation of drug concentration. Associated mainly with the controlled release aspect, and will decrease the side effects that result when the drug concentration reaches its peak. 2. Improved selectivity in receptor activation. Drugs bind to different groups of receptors at high concentrations. In gastroretentive dosage forms (because of less fluctuation in concentration) we can achieve selectivity in binding to the receptor, which also will reduce the side effects of the drug. 3. Reduced counter-activity of the body. The human body has its own balance, and drug are used to change this balance into a more favourable balance, but at the same time if for example we are using a drug to lower blood pressure, the body will have counter mechanisms to cause water retention or to contract the smooth muscles in order to increase the blood pressure. Those counter mechanisms are due to rapid administration of drugs, but if the drug is administered gradually as in gastrorententive dosage forms, those counter mechanisms are minimized. 4. Extended time over critical (effective) concentration. The activity of antibiotics, like Blactam antibiotics, is not associated with Cmax but rather with the time during which the drug stays in the body above MIC “minimum inhibitory concentration”. |Page2 Done By: Lara Mazahreh Advanced Technology Lecture#20 5. Minimized adverse activity at the colon. Antibiotics, for example, are absorbed in the proximal small intestine. If those drugs arrive to the colon in high concentration will adversely affect the normal flora there or development of resistant strains. How to determine whether the drug can be formulated in gastroretentive form or not?! We have certain interactions between pharmacokinetic and pharmacodynamics parameters that will determine whether drug is candidate for gastroretentive dosage form, let’s take example: METFORMIN:Metformin is a glucose lowering agent that is absorbed mainly in the upper part of GIT. It doesn’t follow a direct relationship between plasma drug concentration and magnitude of effect, which adds complexity. Previous studies confirmed that the colonic absorption of metformin is poor and produced poor and inconsistent glucose-lowering effects. On the other hand, it was determined that most of the metformin absorption occurs in the upper parts of the gastrointestinal tract. Assessment of PK–PD rationale for CR-GRDF formulations in a rat model: metformin as a model drug In this study, two controlled release matrix based tablet formulations with different rates of metformin release in vitro were used: CR tablets I (matrix tablets) and CR tablets II (matrix tablets with ethylcellulose coating .The in vitro rate of drug release was assessed according to method described in the USP. This study was conducted to evaluate the pharmacodynamics and pharmacokinetic properties of different formulations in streptozotocin-diabetic rats (each group consisted of 5-6 rats). The studied modes were CR tablets I or II (differ in the rate of drug release) at a dosage corresponding to 450 mg/kg metformin, or the same dose of the drug administered as a bolus oral solution ”immediate release” or a constant rate intraduodenal infusion (intended to simulate gastric retention” gastroretentive dosage forms”). Then, samples were taken at time intervals to measure the amount of metformin in blood (pharmacokinetic profile) and the glucose level (phamacodynamic response of the formulations). The gastric retention of the tablets was assessed radiographically in a separate study applying radiopaque markers added to the tablet formulation. (This is a method used to evaluate gastroretentive formulations; in gastrorentive formulations we are concerned about rate of drug release and region of drug release). And this is achieved by either taking x-ray images to see were the formulation is, or using materials that emit gamma rays that is relatively not harmful to humans. This is the plasma concentration-time profile for the formulations used: |Page3 Done By: Lara Mazahreh Advanced Technology Lecture#20 We notice that: - In the controlled release tablets: drug release from CR1 is faster than CR2. - In PO (simulates immediate release in tablets) solution: Cmax is less than Cr1 which is strange phenomena!!! - Intraduodenal infusion resulted in delayed absorption, highest Cmax. What about the blood glucose? (Effect % was compared to baseline glucose in the animals) We notice that the reduction in glucose level occurred in different percentages in different modes of administration. Look at the duodenal infusion and CR2, were the last to reach the Cmax so their effect more time to develop, but maybe it will be extended for a longer period of time. If we compare PO bolus with duodenal infusion and the two controlled release formulations, we notice that there is no significant difference in effect for the PO (because we get more or less controlled release from immediate release tablets). |Page4 Done By: Lara Mazahreh Advanced Technology Lecture#20 According to those results, we notice that there is no significant benefit from formulating metformin in a gastroretentive dosage form. Why does that happen? Because metformin will be ionized a physiological pH (positive charge), and will bind to the mucin layer of the intestinal mucosa (negative charge), which will result in a mucoadhesive system (due to properties of the drug itself not properties of the dosage form), so we don’t need to modify the dosage form for metformin. If you take a glucophage XR® (methylcellulose matrix system) and put it in the dissolution vessel, you will notice that the whole dissolution process will end up over 3 hours! So we only control the release of the drug by using simple coating system (no need for gastroretentive formulations). So we have to do studies in order to see if the gastroretentive dosage forms will add significant contribution on enhancement of bioavailability over conventional forms. Bioadhesive drug delivery systems Depends mainly on the interaction of the carrier with mucous layer (glycoproteins and glycolipids) that are negatively charged, and we use bioadhesive polymers that are positively charge at physiological PH of the stomach Mucoadhesion. Examples on such polymers: methacrylic acid ester copolymers contains quaternary ammonium group and not water soluble electrostatic interactions and significant adhesion. We can use polymers that do not have positive charge, instead it will dissolve in the acidic environment of the stomach since it’s ionizable at PH of the stomach and produce positive charge. Note that bioadhesion is not only a function of charge, the presence of positive charge is additive, but actually large numbers of polymers we use either negatively charged or neutral (like MC, HPMC) this is due to the fact that mucoadhesion can be as a result of hydrogen bonding or mechanical properties of gel that would stick on the surfaces. Note here, polymers we use have bioadhesive properties, but at the same time they are dissolved in stomach! And we said before that we don’t need only gastric retention property; we also need controlled release, what we can do? Let’s take example, carbopol polymer: It’s linear carboxylic acid polymer “Not ionized at stomach fluids, therefore no electrostatic interactions with mucous layer” with high solubility, can bind to mucous layer but with no effect as controlled release, we have special grade of carbopol (Carbopol 934 P) is cross-linked with allyl sucrose this cross linking will decrease the un-folding of the polymer, decrease the hydration and solubility of the polymer the capacity is the same, it can still take water and form gel which bind to mucous layer controlled release by controlling the diffusion of drug throughout the gel matrix and reduction in the gastric emptying rate. |Page5 Done By: Lara Mazahreh Advanced Technology Lecture#20 |Page6