* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Management of Non-Sustained Ventricular Tachycardia
Survey
Document related concepts
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Saturated fat and cardiovascular disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiovascular disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Transcript
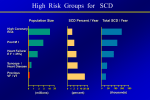
MANAGEMENT OF NONSUSTAINED VENTRICULAR TACHYCARDIA Troy Hounshell, DO Iowa Heart Center Heart Rhythm Center Disclosures • Harvard Clinical Research Institute • Medtronic • Milestone Pharmaceuticals, Inc. • St. Jude Medical • Employee-Iowa Heart Center/Mercy-Des Moines Objectives • Discuss NSVT and its relation to different clinical etiologies • To discuss NSVT risk in relation to SCD • Discuss treatment of NSVT in its presenting clinical setting Definition • There can be many different definitions • Nonsustained ventricular tachycardia (NSVT) is defined as 3 (sometimes 5) or more consecutive beats arising below the atrioventricular node with a heart rate of >100 beats/min and lasting <30 s. The Concern • In several clinical settings, NSVT is a marker of increased risk for subsequent sustained tachyarrhythmias and sudden cardiac death (SCD), whereas it may have no prognostic significance in others. Eur Heart J 2004;25:1093–9 Goal in Managing NSVT • Detect those apparently healthy individuals in whom NSVT represents a sign of occult disease, and to risk stratify patients with known disease who present with this arrhythmia to provide therapy that mitigates associated risks. NSVT with Normal Heart • How to Evaluate • History (Age/PMHx/FMHx/Medications) • 12 Lead ECG • Channelopathy (Brugada/Long QT/Early Reoplarization/ARVD/etc) • How does it respond to exercise? • Suppression with exercise is a marker of benign clinical course** • NSVT during recovery is a better predictor if increase mortality than NSVT during exercise only* • NSVT in athletes is benign and has no adverse prognostic significance (assuming a structural normal heart and channelopathies are excluded)** *N Engl J Med. 2003;348:781–90. **J Am Coll Cardiol 2002;40:446 –52 **Eur Heart J 2008;29:71– 8 **Am J Cardiol 2008;101:1792–5. J Am Coll Cardiol 2012;60:1993–2004 Idiopathic VT • Typically referred to as outflow tract tachycardia's • Benign arrhythmia • May be sustained or repetitive monomorphic NSVT • Usually a result of triggered activity from heightened intracellular calcium • Usually a LBBB (RVOT) inferior axis with transition usually occurring around V4 • Can be RBBB (LVOT) with inferior axis. Transition usually occurring around V1-V2 • Treatment aimed at symptoms and typically occurs with BB, CCB. Many times BB with Class IC antiarrhythmic are used for efficacy Idiopathic vs Arrhythmogenic Right Ventricular Dysplasia Idiopathic VT ARVD • RBBB or LBBB • QRS Lead I >120ms • Inferior Axis • Earliest-onset QRS V1 • Transition at V4 or V1-2 • QRS notching • Transition V5 or later J Am Coll Cardiol 2011;58:831– 8 JACC Vol. 58, No. 8, 2011 JACC Vol. 58, No. 8, 2011 NSVT with Hypertension and Valvular Heart Disease Hypertension Valvular Heart Disease • Burden closely correlates • High correlation between with LVH • No convincing evidence to suggest increased risk of SCD • Should have evaluation for IHD • Treat hypertension aggressively NSVT and VHD • NSVT marker of LV pathology • No evidence to suggest NSVT predicts SCD even after valve replacement • Treat valve disease Am J Cardiol 1992;69:913–7 Circulation 1997;96: 500–8 Am Heart J 1987;113:1298-307 N Engl J Med 1987;317:787–92 NSVT and Coronary Artery Disease NSTEMI NSTEMI Am J Cardiol 2011;108:1373–81 NSVT and Coronary Artery Disease • After the reperfusion era evidence now exists to suggest that NSVT no longer carries independent risk death in IHD once other factors like EF are taken into account* • CARISMA study showed EF <40% with NSVT (> 125 BPM >16 beats <30s) showed no association with cardiac death over 2 years after multivariable analysis** *Circulation 1997;96:1888 –92 *Circulation 1993;87:312–22 *J Am Coll Cardiol 1999;33:1895–*902 *Circulation 2001;103:2072–7 *Eur Heart J 2005;26:762–9 **Circulation 2010;122:1258–64 NSVT and Coronary Artery Disease • When to study? • MUSTT trial (EF <40%) • Evaluated in hospital vs post hospital presentation of NSVT* • Patients post surgical revascularization with NSVT showed worse outcomes when NSVT occurred late after surgery vs early* • An exception seems to be patients with early NSVT post surgery with sustained VT at EPS. These patients had poor outcomes** • Other modalities • Heart rate variability, T-Wave alternans • Not well delineated to warrant routine use *J Am Coll Cardiol 2001;38:1156–62 *J Cardiovasc Electrophysiol 2002;13:757– 63 **J Cardiovasc Electrophysiol 2002;13:342– 6 NSVT and LV Dysfunction/ Congestive Heart Failure • NSVT in this population is common and can be as high as 80% • Two studies CHF-STAT and PROMISE failed to show NSVT to predict SCD or total mortality* • Only in the recovery period of exercise does “severe ectopy” show adverse prognostic significance** • In patients with idiopathic dilated cardiomyopathy NSVT and LVEF <30% showed 8 fold increase in arrhythmia risk compared to other groups. NSVT by itself was not predictive.*** *N Engl J Med 1995;333:77– 82 *Circulation 2000;101:40–6 **J Am Coll Cardiol 2004;44:820–6 ***Circulation 2003;108:2883–91 Special Populations • HOCM • Incidence of 20-30% • Appears to be related to myocardial fibrosis as MRI delayed enhancement and echo strain relate to presence of NSVT • Associated with worse LVH and more symptomatic HCM • High risk factors • Syncope • Frequent NSVT • FMHx SCD young age • Severe LVH (Wall thickness >30mm) • Abnormal BP response to exercise • Zero to one risk factor shows ~1% risk SCD (low) • 2 or more risk factors have high SCD risk J Am Coll Cardiol 2003;42:873–9 J Am CollCardiol 2005;45:697–704 Heart 2004;90:570–575 Special Populations ARVD • A condition of fibrofatty infiltration of the myocardium classically in the right ventricle (can be left ventricle) resulting in cardiomyopathy and eventual RV dyfunction • Increased risk for SCD • Patient can present with asymptomatic NSVT and be at increased risk for SCD • NSVT may be monomorphic or Polymorphic Giant Cell Myocarditis • Usually sustained arrhythmias with high SCD risk Repaired TOF • 50% will have NSVT with 4-14% prevalence of sustained VT • Inducible Sustained VT is marker of subsequent events