* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download COAGULATION AND TRANSFUSION MEDICINE Original Article
Survey
Document related concepts
Transcript
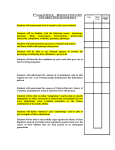
COAGULATION AND TRANSFUSION MEDICINE Original Article D e t e c t i o n Development of of the Factor V a Testing and Algorithm L e i d e n Combining Molecular M u t a t i o n a Coagulation Assay Diagnosis LINDA M. WASSERMAN, MD, 1 J. ROGER EDSON, MD, 2 NIGEL S. KEY, MB, MRCR 3 RAJNICHIBBAR, MD, 2 AND RONALD C. McGLENNEN, MD 2 The Coagulation and Molecular Diagnostic laboratories at the University of Minnesota Medical School (Minneapolis) have collaborated to develop a diagnostic algorithm to identify all factor VLeiden mutation carriers without performing unnecessary and expensive genetic testing. The algorithm uses a coagulation assay for activated protein C resistance (APCR) to determine the need for genetic testing. We report the results of our experience validating this program. We compared the sensitivity, specificity, and positive and negative predictive values of two measures of APCR, the APCR ratio and the normalized ratio. We found that the normalized ratio was the more sensitive but less Resistance to activated protein C was first described by Dahlback et al 1 and Griffin et al 2 in patients younger than 50 years with a history of v e n o u s thrombosis but no other known thrombotic risk factors. Activated protein C resistance (APCR) in these patients was defined as a relative failure to prolong their activated partial thromboplastin times (APTTs) by addition of activated protein C. Plasma-mixing experiments for patients with APCR could be corrected by all deficient plasmas except those missing factor V.3 Identification of a G to A transition mutation at codon 506 in the factor V gene quickly followed.4 The mutation acts as an autosomal dominant and renders factor Va approximately 10 times less sensitive to proteolysis by activated protein specific parameter to determine the need for genetic testing. By using the normalized ratio as the standard by which to refer patients to the Molecular Diagnostics Laboratory, all mutation carriers were identified. We found a large overlap in both measures of APCR between symptomatic patients with normal genotype and mutation carriers. Furthermore, we demonstrated that increased factor VIII levels with a normal genotype are associated with apparent APCR. In this article we also review other correlates of apparent APCR. (Key words: Factor VLeiden mutation; Activated protein C resistance; Molecular diagnosis) Am J Clin Pathol 1997;108:427-433. C. This mutation is found in as many as 96% of thrombophilic families with hereditary APCR.6 Results of several European studies suggest that the prevalence of the mutation in white populations may be as high as 5 % / Consequently, the factor V Leiden mutation is considered the most common inherited hypercoagulability defect. In the laboratory examination of the patient with thrombophilia, the diagnosis of APCR due to the presence of the factor V Leiden mutation can be made by combining coagulation assays with genetic testing. Because the coagulation assay is relatively inexpensive to perform, it is the more cost-effective test to be ordered first to evaluate APCR. Genetic testing is then indicated if an abnormal coagulation result is obtained. Appropriate parameters for defining an abnormal coagulation result must be established for theSan coagulation test. These parameters must be sensiFrom the ^Department of Medicine, University of California, tive enough to identify all patients likely to possess Diego, La jolla, California, and the Departments of ^-Laboratory Medicine and Pathology and 3Medicine, University of Minnesota Medicalthe School, mutation but specific enough to limit unnecessary Minneapolis, Minnesota. genetic testing. Since October 1994, the Coagulation Laboratory Manuscript received November 14, 1996; revision accepted February 21,1997. and the Molecular Diagnostics Laboratory in the Address reprint requests to Dr Wasserman: Molecular Genetics Department of Laboratory Medicine and Pathology Laboratory, Division of Medical Genetics, Department of Medicine, at the University of Minnesota (Minneapolis) have University of California, San Diego, La Jolla, CA 92093-0639. 427 COAGULATION AND TRANSFUSION MEDICINE Article 428 jointly p r o v i d e d evaluation of APCR d u e to the presence of the factor V L e i d e n mutation. The goal of this program has been to establish a testing algorithm in which evaluation of APCR by coagulation assay precedes and determines the need for genetic testing. We report the results of our experience, including the sensitivity and specificity of a coagulation assay as an indicant of the presence of the factor V L e i d e n mutation, a comparison of two methods to calculate APCR based on the coagulation assay results, and an analysis of correlates of apparent or a c q u i r e d APCR in a d d i t i o n to the factor V Leiden mutation. Characteristics Reference ranges for APCR were established from v a l u e s d e r i v e d from v e n o u s b l o o d collected in buffered citrate vacuum tubes from 59 healthy men and women volunteers younger than 40 years. After the exclusion of nine outliers, reference ranges for APCR, calculated as the APCR ratio and the normalized ratio, were determined. Validation of the molecular assay was based on 22 men and w o m e n , some healthy volunteers, some patients with thrombophilia, for whom APCR values based on the coagulation assay had been determined. The validation sample for the molecular diagnostic assay was chosen to have a range of normal and abnormal APCR values. Continuing validation of the coagulation assay and determination of its sensitivity and specificity was based on an additional sample of 125 individuals for whom molecular diagnostic testing and coagulation a s s a y s for APCR w e r e c o m p l e t e d . This g r o u p i n c l u d e d a c o m b i n a t i o n of h e a l t h y v o l u n t e e r s , patients with thrombophilia, and relatives of known factor V L e i d e n mutation carriers. Coagulation Assay for Protein C Resistance APCR ratio = APTT + Activated Protein C APTT Normalized Ratio = APCR Ratio of Patient APCR Ratio Standard The APCR ratio standard was determined by evaluating the APTT with and without the addition of activated protein C from aliquots of 100 mL of pooled venous blood collected from 40 volunteers with norm a l g e n o t y p e s , y o u n g e r t h a n 40 y e a r s , e q u a l l y divided between men and nonpregnant women, and not receiving medication. Factor VIII Assay METHODS Sample Calculation of APCR was performed in two ways: Factor VIII assays were performed by a one-stage assay on an (Elecktra-700, M e d i c a l L a b o r a t o r y Automation, Pleasantville, NY) using i m m u n o d e pleted factor VHI-deficient plasma (manufactured by Diagnostica Stago, Asnieres, France; purchased from American Bioproducts, Parsippany, NJ). The partial thromboplastin time reagent was prepared in the Coagulation Laboratory as described in the preceding section. The test specimens a n d s t a n d a r d plasma were each tested at dilutions of 1:10, 1:20, 1:40, and 1:80. Factor VIII activity of the unknown compared with the standard was calculated using a Microsoft Excel (Microsoft, R e d m o n d , Wash) spreadsheet. Standard plasma was a pool containing equal volumes of plasma from healthy donors with n o r m a l genotypes, 25 m e n a n d 25 w o m e n , n o n e older than 40 years. None of the women were taking oral contraceptives. Factor VIII activities higher than 100% in the experimental specimens were obtained by a d d i n g v a r i o u s a m o u n t s of an i n t e r m e d i a t e purity factor VIII concentrate (Humate-P, manufactured by Behring Werke, AG, Marburg, Germany; d i s t r i b u t e d in t h e U n i t e d S t a t e s b y A r m o u r Pharmaceutical, Kankakee, 111). DNA Activated Resistance to activated protein C was tested essentially as described by Griffin et al, 2 except that the partial thromboplastin time reagent used was prepared in the Coagulation Laboratory. It consisted of an equal-part mixture of the classic Bell and Alton 8 phospholipid reagent and a 0.075% suspension of a finely divided aluminum silicate powder obtained from Sigma Chemical(St Louis, Mo). Extraction High-molecular-weight DNA was extracted from peripheral blood lymphocytes anticoagulated with buffered citrate (acid-citrate-dextrose) or EDTA using the Puregene DNA Isolation Kit (Gentra Systems, Research Triangle Park, NC) according to the manufacturer's directions. Quantification of the purified DNA was determined by measuring the optical density at 260 um with a spectrophotometer (Beckman DU-64, Allendale, NJ). AJCP> lober 1997 WASSERMAN ET AL Testing for Activated Protein C Resistance 429 values was obtained were referred to the Molecular Diagnostic Laboratory for genetic testing. Polymerase Chain Reaction A 100-uL mixture including 500 ng genomic DNA, 1.5 m m o l / L m a g n e s i u m c h l o r i d e , 200 u m o l / L deoxynucleoside triphosphate, 600 nmol/L oligonucleotide p r i m e r s , a n d 1 U A m p l i t a q (Promega, Madison, Wis) was used to amplify a 267-base pair fragment according to the methods of Bertina et al. 4 The parameters for thermocycling include the following: 1 minute at 94°C, then 35 cycles of 94°C for 1 minute, 56°C for 1 minute, and 72°C for 2 minutes. The primer sequences were 5'-TGCCCAGTGCTTAACAAGACCA-3' and 5'-TGTTATCACACTGGTGCTAA-3'. Molecular Diagnosis of the Factor V Mutation The presence or absence of the G to A mutation at codon 506 of the factor V gene was evaluated by a combination of polymerase chain reaction and slot blot hybridization with 3 2 P-labeled allele-specific TABLE 1. APCR RATIOS AND NORMALIZED RATIOS FOR REFERENCE AND VALIDATION SAMPLES Slot Blot Normalized Ratio APCR Ratio For slot blot hybridization, 40 uL of denatured polymerase chain reaction product was filtered onto nitrocellulose (Gibco BRL, Grand Island, NY), crosslinked with 1200 uj of UV light, and hybridized for 1 h o u r at 42°C w i t h 3 2 P-labeled sequence-specific oligonucleotides (5'-TGGACAGGCgAGGAATAC-3' for the normal allele, 5'-TGGACAGGCaAGGAATAC3' for the mutated allele). After hybridization, blots were washed at room temperature for 1 to 2 minutes and then for 10 minutes in 2x SSPE/0.1% sodium dodecyl sulfate at 52°C for the normal allele and 49°C for the mutated allele. Overnight autoradiography with intensifying screens was performed with medical x-ray film (Fuji, Greenwood, SC). Sample Reference Validation G/G G/A A/A Number Mean SD Mean SD 50 2.06 0.24 1.09 0.12 63 58 4 1.74 1.36 1.02 0.26 0.14 0.28 0.90 0.70 0.52 0.14 0.065 0.02 APCR = activated protein C resistance. G/A G/G RESULTS G/G Establishment of Reference Ranges ofAPCR G/G The reference ranges for the two m e a s u r e s of APCR, the APCR ratio and the normalized ratio, were established from APTT values o b t a i n e d using a reagent made in the Coagulation Laboratory. When using this in-house APTT reagent, the normal range of the APTT, the response to increasing concentrations of heparin, and the prolongation of the APTT associated with a number of inherited deficiencies are similar to APTT values obtained when using the Organon Teknika (Durham, NC) and Stago APTT reagents. The reference ranges of the APCR ratio and the normalized ratio are given in Table 1. An abnormal value for each parameter was defined as the mean minus 2 SD. For the APCR ratio, this value was 1.57; for the normalized ratio, 0.85. Patients examined in the Coagulation Laboratory for APCR in whom an APCR ratio or a normalized ratio near or below these G/G G/G G/A « ! • A/A H,0 FIG 1. Slot blot hybridization of normal and mutated factor V alleles. A 267-base pair amplicon was slot blotted onto nitrocellulose, hybridized for 1 hour at 42°C with 32P-labeled oligonucleotides specific for the normal or mutated sequence. Blots were washed in 2x SSPE at 49°C for the oligonucleotide bearing the G to A mutation and at 52°C for the oligonucleotide with the normal sequence and autoradiographed overnight. Vol. 108 • No. 4 430 COAGULATION AND TRANSFUSION MEDICINE Original Article oligonucleotides. The results of a representative slot blot assay are s h o w n in Figure 1. Allele-specific oligonucleotide hybridization was achieved by careful monitoring of the stringency of the hybridization and wash conditions. Overnight autoradiography was sufficient in most cases. Comparison of the APCR Ratio and the Normalized Ratio as Indicators of Factor V Genotype Quantification of APCR, as measured by the coagulation assay, and determination of factor V L e i d e n mutation status, as evaluated by molecular testing, was obtained in an additional cohort of 125 men and women. Most of the cohort members were examined because of a history of thrombosis. A minority of the cohort members were asymptomatic volunteers or relatives of known factor V L e i d e n mutation carriers. The mean APCR ratios and normalized ratios for each genotype are shown in Table 1. Because this additional cohort included many patients with thrombophilia, the mean APCR ratio and the mean normalized ratio of the sample as a whole and of those with a normal factor V genotype were lower than the values obtained from the original reference group. The relationship between genotype, the APCR ratio, and the normalized ratio are shown in Figures 2 and 3. Both figures demonstrate a gene dosage effect on the range of APCR ratio and normalized ratio values. There is also a large region of overlap, indicated by s h a d i n g in each figure, b e t w e e n the v a l u e s obtained by factor V L e i d e n mutation heterozygotes and symptomatic patients with a normal factor V genotype who have apparent APCR. The relative sensitivity, specificity, and positive and negative predictive values of the APCR ratio and the normalized ratio are given in Table 2. Based on the reference ranges established by our original group of healthy adults, the normalized ratio proved to be a more sensitive indicator of the need for genetic testing, although it had lower specificity. None of the factor V L e J d e n mutation carriers were misclassified as having a normal genotype when using the normalized ratio. In contrast, four heterozygotes would have been misclassified as having a normal genotype using the APCR ratio as the standard. Of the 63 patients ••• •• • 1.57 —-i-JT FIG 2. Relationship between activated protein C resistance (APCR) ratios and genotype for the validation sample. APCR ratios and factor V mutation status were determined for the validation sample. An APCR ratio less than or equal to 1.57 was considered abnormal. Shading indicates the region of overlap between normal genotypes (G/G) and mutation carriers (G/A). G/G G/A FIG 3. Relationship between normalized ratios and genotype for the validation sample. Values less than or equal to 0.85 were considered abnormal. Shading indicates the region of overlap between normal genotypes (G/G) and mutation carriers (G/A). AJCP • October 1997 WASSERMAN ET AL Testing for Activated Protein C Resistance with a normal genotype in the validation sample, 32 (51%) h a d a p p a r e n t APCR based on n o r m a l i z e d ratios. In contrast, 13 patients with a normal genotype were misclassified using the APCR ratio. The diagnostic algorithm jointly established by the Coagulation and Molecular Diagnostic Laboratories is depicted in Figure 4. In this schema, a patient with thrombophilia who is not receiving anticoagulant t h e r a p y is referred to the Molecular Diagnostic Laboratory for genetic testing only if the normalized ratio is 0.85 or less. Depending on the patient's family and personal history of thrombosis and the referring physician's requests, evaluation of other heritable causes of thrombophilia, including deficiencies of proteins C and S and antithrombin III, may proceed while the patient's factor V L e i d e n genotype is determined by the Molecular Diagnostic Laboratory. If the normalized ratio is greater than 0.85, the p a t i e n t does not have APCR, a n d a coagulation workup for other causes of thrombophilia continues. This w o r k u p includes platelet sizing, a D-dimer enzyme-linked immunosorbent assay (ELISA), a prothrombin fragment 1.2 ELISA, evaluation of the levels of Clauss fibrinogen, fibrinogen antigen, protein C, protein S, and plasminogen, as well as evaluation of the presence of a lupus inhibitor, fluorescent antinuclear antibody, and anticardiolipin antibody. In about one third of cases, a methionine loading test for hyperhomocysteinemia is included in the thrombophilia workup. DNA testing for the factor V L e i d e n mutation proceeds immediately in the patient receiving anticoagulation therapy who has a history of thrombosis. This algorithm is preferred to other methods of determining APCR in heparinized patients. Evaluating the APCR ratio by first absorbing plasma on an AT-3 column to remove heparin is more expensive than performing the DNA test. Use of an AT-3 column would likely introduce dilutional and other artifacts, making the APCR ratio difficult to interpret. 431 TABLE 2. COMPARISON OF THE APCR RATIO AND THE NORMALIZED RATIO AS INDICATORS OF THE PRESENCE OF THE FACTOR VLE|DEN MUTATION APCR Ratio (<1.57) Normalized Ratio (<.85) 94 79 100 51 82 93 67 100 Sensitivity (%) Specificity (%) Predictive value Positive (%) Negative (%) APCR = activated protein C resistance. Thrombophilia patient / \ Anticoagulated Refer for factor Leider,genotyping. v • v Not anticoagulated If normalized ratio • <0.85, refer for factor VLeiden genotyping. Continue evaluation of other heritable causes cause of thrombosis. If normalized ratio >0.85, continue coagulation workup for other causes of thrombosis. Patient does not have APCR. \ If patient is G/G, continue coagulation workup for other causes of thrombophilia, If patient is G/A or A/A, provide counseling re: risk factors for other thrombotic episodes; advise genetic testing for at-risk family members. FIG 4. Diagnostic algorithm for the evaluation of activated protein C resistance (APCR) in patients with thrombophilia, combining a coagulation assay with genetic testing. between increasing factor VLTJ levels and APCR as measured by the APCR ratio and the normalized ratio is shown in Table 3. As factor VIII levels increase, the APCR ratio and the normalized ratio approach values indicating APCR. Thus, patients with normal factor V genotypes but with elevated factor VIII levels could be misclassified as having APCR. Effect of Factor VIII Levels on APCR Coagulation assays for APCR reflect the combined effect of complex interactions among proteins in the coagulation and anticoagulation cascades, including factors V and VIII, thrombin, antithrombin III, plasminogen, and proteins C and S. To evaluate other correlates of APCR in addition to the factor V ^ ^ mutation, we measured the effect of increasing factor VIII levels on the APCR ratio and the normalized ratio on a sample with a normal factor V genotype. The relationship DISCUSSION The Coagulation Laboratory and the Molecular Diagnostic Laboratory at the University of Minnesota Medical School have collaboratively established a testing algorithm for evaluation of APCR as a cause of thrombophilia. The schema evaluates the diagnostic utility of using the less expensive and less time-consuming coagulation assay to determine the need for genetic testing for presence of the factor V ^ ^ mutation in patients Vol. 108 • No. 4 432 COAGULATION AND TRANSFUSION MEDICINE Original Article with thrombophilia who are not receiving anticoagulation therapy. We compared the sensitivity and specificity of two methods of quantifying APCR by the coagulation assay and found the normalized ratio, which c o m p a r e s the APCR ratio of the p a t i e n t to the APCR ratio of pooled reference plasma to be the more sensitive measure. No mutation carriers were misclassified as having a normal genotype by this measure. We favor use of the normalized ratio as the most sensitive parameter because of the lifetime risk for thrombotic episodes in mutation carriers and the need to educate them about prevention of future episodes, as well as the i m p o r t a n c e of identifying first-degree relatives w h o also may carry the mutation. However, maximizing the sensitivity of the c o a g u l a t i o n assay led to a lower specificity and positive predictive value. Using this algorithm, 32 of 125 patients referred for genetic testing h a d a n o r m a l g e n o t y p e a n d a p p a r e n t or acquired, rather than hereditary, APCR. Zehnder and Benson 9 reported a similar loss of specificity when maximizing the sensitivity of a commercially available APCR assay to identify factor V L e i d e n TABLE 3. EFFECT OF INCREASING FACTOR VIII LEVELS ON APCR Factor V11I Level (%) APCR Ratio 94 155 370 620 1.70 1.70 1.56 1.42 Normalized Ratio 0.88 0.88 0.81 0.74 APCR = activated protein C resistance. TABLE 4. CORRELATES OF APPARENT APCR WITH A NORMAL FACTOR V GENOTYPE Correlate Elevated factor VIII (> 100%) Use of oral contraceptives Female sex Age 35 years or older Reduced protein S Elevated protein C Elevated plasminogen Presence of lupus anticoagulant Presence of P2-glycoprotein I antigen-antibody complexes APCR = activated protein C resistance. Reference No. Current study, 10 10,11,13 Current study, 10-13 12 Current study, 12 Current study, 11 Current study 16 17,18 m u t a t i o n carriers. When factor V L e i d e n m u t a t i o n carriers are identified by genetic testing, they are referred for genetic counseling. They are informed a b o u t risk factors a s s o c i a t e d w i t h t h r o m b o t i c episodes, and they are counseled about the need for genetic testing of first-degree relatives, siblings, and children, who have a 50% risk of also carrying the mutation. False-positive or acquired APCR in a patient with a normal factor V genotype is known to be correlated with a variety of factors, including abnormal concentrations of procoagulant and regulatory proteins, age, female sex, oral contraceptive use, and presence of lupus anticoagulant and anticardiolipin antibody. 10-16 Reviewing with clinicians the role of these factors in causing apparent APCR in patients with a normal factor V genotype is an important function of the directors of the Coagulation and the Molecular Diagnostic Laboratories. We have found that increasing factor VIII levels decreased the APCR ratio and the normalized ratio to levels indicating APCR, a relationship noted by others. 10 We have confirmed as well the observation that an abnormal APCR ratio and normalized ratio in a patient with thrombophilia and a normal factor V genotype can be associated with abnormally elevated levels of protein C, antithrombin III, and plasminogen and with reduced levels of protein S (data not shown). 11 In our sample, 78% (28 of 32) of those with a normal factor V g e n o t y p e a n d APCR w e r e w o m e n . O t h e r s also h a v e n o t e d l o w e r APCR r a t i o s in women. 10,12 Calkins et al, 12 in validating the coagulation assay for APCR for the S c r i p p s Reference Laboratory (La Jolla, Calif), suggested use of separate reference ranges for men and women because women had, on average, lower APCR ratios. This group also f o u n d an a s s o c i a t i o n w i t h a g e ; APCR r a t i o s decreased progressively in both sexes after 35 years of age. We did not observe this age effect in our sample. The group of patients with a normal factor V genotype and apparent APCR ranged in age from 25 to 77 years. Several groups have noted that apparent APCR in women is compounded by use of oral contraceptive pills and have suggested that this effect might be mediated by the effect of hormone modulation on procoagulant and regulatory protein levels. 1 0 ' 1 1 ' 1 3 Indeed, epidemiologic studies have shown that the use of oral contraceptives by factor V L e i d e n mutation carriers is associated with an 8- to 10-fold increase in the risk of having a thrombotic episode. 14,15 AJCP • October 1997 WASSERMAN ET AL Testing for ActivaU Protein C Resistance The presence of antiphospholipid antibodies is likewise associated with acquired APCR.16"18 Potzsch et al 1 6 defined APCR as the amount of factor VIII inactivation found when adding activated protein C to plasma of patients with lupus anticoagulant. They found apparent APCR in patients with histories of thrombotic episodes and presence of a lupus anticoagulant. Matsuda et al 17 found that addition of (^"Sty" coprotein I antigen-antibody complexes to pooled normal plasma led to a dose-dependent decrease in the APCR ratio. (^-glycoprotein I is believed to represent the cofactor involved in the binding of antibodies to cardiolipin. Table 4 summarizes the various correlates of apparent or acquired APCR. We have demonstrated that a cooperative effort b e t w e e n the C o a g u l a t i o n L a b o r a t o r y a n d the Molecular Diagnostic Laboratory can provide costeffective examination of the patient with thrombophilia for the presence of APCR due to the factor ^Leiden m u t a t i o n . The use of a testing algorithm combining a less-expensive coagulation assay with m o r e - e x p e n s i v e m o l e c u l a r genetic t e s t i n g w a s developed to optimize diagnostic sensitivity while keeping overall testing costs down. When the normalized ratio as a measure of APCR was greater than the reference value, genetic testing was not necessary. Only patients in whom normalized ratio values approaching or below the reference value were obtained were referred for genetic evaluation. I m p l e m e n t a t i o n of this a l g o r i t h m identified all patients w h o had the factor V L e i d e n mutation. We anticipate that future developments to simplify the molecular testing method will provide further cost savings and diagnostic efficiency while maintaining the current level of sensitivity in identifying factor V L e i d e n mutation carriers. Whether further reduction in costs of molecular testing for the factor V L e i d e n mutation will eliminate t h e u t i l i t y of d e t e r m i n i n g APCR is d e b a t a b l e . Whereas the most common cause of APCR is the factor V L e i d e n mutation, other as yet undefined factor V or factor VIII mutations could lead to APCR. APCR remains a relatively inexpensive laboratory test to measure thrombotic risk. 433 REFERENCES 1. Dahlback B, Carlsson M, Svensson PJ. Familial thrombophilia due to a previously unrecognized mechanism characterized by poor anticoagulant response to activated protein C: prediction of a cofactor to activated protein C. Proc Natl Acad Sci USA. 1993;90:1004-1008. 2. Griffin JH, Evatt, B, Wideman, C, Fernandez JA. Anticoagulant protein C pathway defective in majority of thrombophilic patients. Blood. 1993;82:1989-1993. 3. Sun X, Evatt B, Griffin JH. Blood coagulation factor Va abnormality associated with resistance to activated protein C in venous thrombophilia. Blood. 1994;83:3120-3125. 4. Bertina RM, Koeleman BPC, Koster T, et al. Mutation in blood coagulation factor V associated with resistance to activated protein C. Nature. 1994;369:64-67. 5. Zoller, B, Dahlback B. Linkage between inherited resistance to activated protein C and factor V gene mutation in venous thrombosis. Lancet. 1994;343:1536-1538. 6. Griffin J, Heeb M, Kojima Y, et al. Activated protein C resistance: molecular mechanisms. Thromb Haemost. 1995;74:444-448. 7. Dahlback B. Inherited thrombophilia: resistance to activated protein C as a pathogenic factor of venous thromboembolism. Blood. 1995;85:607-614. 8. Bell WN, Alton HG. A brain extract as a substitute for platelet suspensions in the thromboplastin generation test. Nature. 1954;174:880-881. 9. Zehnder JL, Benson RC. Sensitivity and specificity of the APC resistance assay in detection of individuals with factor VLeiden. Am J Clin Pathol. 1996;106:107-111. 10. Henkens CMA, Bom VJJ, van der Meer J. Lowered APC-sensitivity ratio related to increased factor VHI-clotting activity. Thromb Haemost. 1995;74:1198-1199. 11. Olivieri O, Friso S, Manzato F, et al. Resistance to activated protein C in healthy women taking oral contraceptives. Br J Haematol. 1995;91:465-470. 12. Calkins T, Greengard J, Griffin JH, Bylund D. Anticoagulant response to activated protein C: method validation and assay comparison. / Clin Lab Anal. 1995;9:418^23. 13. Henkens CMA, Bom VJJ, Seinen AJ, van der Meer J. Sensitivity to activated protein C: influence of oral contraceptives and sex. Thromb Haemost. 1995;73:402-404. 14. Bloemenkamp KWM, Rosendaal FR, Helmerhorst FM, Biiller HR, Vandenbroucke JR Enhancement by factor VL iden mutation of risk of deep-vein thrombosis associated with oral contraceptives containing a third-generation progestagen. Lancet. 1995;346:1593-1596. 15. Vandenbroucke JP, Koster T, Brief E, et al. Increased risk of venous thrombosis in oral-contraceptive users who are carriers of factor VLeiden mutation. Lancet. 1994;344:1453-1457. 16. Potzsch B, Kawamura H, Preissner K, et al. Acquired protein C dysfunction but not decreased activity of thrombomodulin is a possible marker of thrombophilia in patients with lupus anticoagulant. / Lab Clin Med. 1995;125:56-65. 17. Matsuda J, Gotoh M, Gohchi K, et al. Resistance to activated protein C activity of an anti-b2-glycoprotein I antibody in the presence of B2 -glycoprotein I. Br J Haematol. 1995; 90:204-206. 18. Key NS. Toward an understanding of the pathophysiologic mechanism of thrombosis in the antiphospholipid antibody syndrome. / Lab Clin Med. 1995;125:16-17.