* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Accuracy of natriuretic peptides levels in the diagnosis of left
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Echocardiography wikipedia , lookup
Heart failure wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
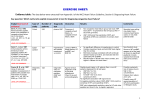
Accuracy of natriuretic peptides levels in the diagnosis of left ventricular dysfunction – Systematic review Pontes J., [email protected] Almendra R., [email protected] Carvalho J., [email protected] Moreira C., [email protected] Martins A., [email protected] Afonso A., [email protected] Leitão M. A., [email protected] Rodrigues G., [email protected] Gaspar R., [email protected] Lima S., [email protected] Martinho C., [email protected] Correia F. [email protected] Adviser: Almeida F., [email protected] Class: 11 Oporto medical faculty, 2007 Abstract Introduction Echocardiography is a common tool in the diagnosis of left ventricular dysfunction (LVD) but recent clinical and experimental studies also report the role of Brain Natriuretic Peptides in the diagnosis of this pathology. Aim To evaluate the accuracy of the brain natriuretic peptide levels in the diagnosis of systolic LVD when compared to echocardiography. Methods A standard systematic review methodology was followed. Published literature was searched through the PubMed and Cochrane Library electronic databases. Inclusion and exclusion criteria were applied. 23 articles (12,082 patients) were analyzed. Results In BNP studies, 11 of 16 had sensitivities lower than 71% and 6 of 16 studies had specificities lower than 77%. 5 of 10 NT-proBNP studies had sensitivities lower than 88% and 4 of 10 studies had specificities inferior to 68%. In 9 articles analysing BNP, with an interval of cut-offs from 19.2 to 100pg/ml, it was verified significant differences in what concerns to specificity. In a cut-off’s interval from 20 to 75pg/ml, the accuracy was inconsistent. The pooled of LR- were heterogeneous (p<0.05). Discussion Our results suggest that the diversity of cut-off points is a source of heterogeneity in the accuracy of both tests. Conclusion BNP and NT-proBNP tests appear to have high sensitivity and they might be helpful in the ruling out of systolic LVD. Key words Left Ventricular Dysfunction, Brain Natriuretic Peptide, Sensitivity and Specificity Introduction Heart failure (HF) is a pathophysiologic state in which the heart is unable to pump blood at a rate commensurate with the requirements of the metabolizing tissues [1]. Nowadays, heart failure, such as left ventricular dysfunction (LVD), is a major health problem, especially in developed countries, where it is associated with coronary artery disease, obesity and hypertension [2]. HF is the most common cause of hospitalization due to cardiovascular disease in patients over 65 years [3] and the number of HF deaths has increased steadily despite advances in treatment. The clinical diagnosis of heart failure or left ventricular dysfunction is complex, especially in the presence of other pathologies such as respiratory disease or obesity [4, 5] The echocardiography is the common test used to diagnosis LVD, but the access to . population is limited, especially in primary care [6] Its restricted availability and high costs prohibit its use as a general screening test [7]. Electrocardiogram (ECG) is an alternative method to diagnosis HF, but it is insensitive and non-specific. Most recently, a new diagnostic test has been used for LVD: the measurement of the blood levels of Brain Natriuretic Peptides (BNP) [8]. The BNP is the most relevant in the diagnosis of HF, because it’s secreted rapidly and has a longer half-time in circulation [8]. BNP is synthesized as a larger inactive molecule, the proBNP, which is cleaved in two molecules: an active hormone, BNP, and a biologically inactive Nterminal peptide fragment, NT-proBNP [9]. BNP is produced constantly by ventricular cells in response to heart normal function, but an increased myocardial wall stress induces the production of higher concentrations of BNP [10]. The aim of this study is to evaluate the accuracy of brain natriuretic peptides in the diagnosis of systolic LVD when compared to echocardiography or radionuclide ventriculography. Methods Data search We conducted a systematic review of studies on the diagnosis accuracy of BNP and NT-proBNP levels in the Cochrane Central Register of Controlled Trials (CENTRAL) at The Cochrane Library and in the Medline database. The Medline search was made in Pubmed using the MESH terms: "Ventricular Dysfunction, Left", "Heart Failure, Congestive"; "Natriuretic Peptide, Brain"; "Sensitivity and Specificity"; "ROC Curve" "clinical trials"; and the terms (as text words): "Cardiac failure"; "Cardiac dysfunction"; "Heart dysfunction"; "BNP"; "NTproBNP"; "Accuracy"; "Likelihood ratio" and "Predictive value". The search in the Cochrane Library was made using the same MESH terms and text words used in the Pubmed search. Both searches were concluded until February 2007. Inclusion and exclusion criteria – articles selection 2 In an initial phase the titles and abstracts of the articles were reviewed to identify all potential studies, without making restrictions to the time of publication. Full text versions were obtained, if considered necessarily. This task was performed by six groups of two reviewers bearing in mind the following inclusion criteria: (1) Being written in English, Portuguese, French or Spanish; (2) Publications on the accuracy or sensitivity and specificity of BNP levels in the diagnosis of systolic left ventricular dysfunction; (3) To compare the diagnostic accuracy of NTproBNP or BNP to the gold standard for diagnosing the heart failure, such as echocardiography and radionuclide ventriculography. In the second phase we performed the exclusion of studies. This task was realized by two groups of three reviewers, having read the methods section of each study and applied the exclusion criteria. These were: (A) To evaluate diastolic dysfunction; (B) To be limited to very restrictive study groups such as patients with Duchenne disease; Chagas disease or Brugada syndrome; (C) To be performed in non human population; (D) To associate the cardiac failure to congenital or hereditary diseases. The selection of the articles was only made under the overall reviewers’ approval. In case of disagreement, a third reviewer would interview. The articles which the complete text was not found were excluded. Assessment of study quality Two reviewers assessed the quality of each included trial according to the QUADAS tool [11]: (I) To compare with an independent appropriate gold standard, (II) To include patients who cover a wide patient spectrum likely to be encountered in a usual clinical practice setting, (III) To interpret the index test result without the knowledge of gold standard, and vice-versa, (IV) To prospectively recruit consecutive patients suspected to have the disease of interest. Data Extraction For each study selected, two reviewers extracted data independently. Data on year of publications, spectrum of patients, sensitivity, specificity and predictive values, diagnosis accuracy and type of assay were extracted from original articles. The information was then reunited in order to confirm the data extracted. Data aggregation and analysis 3 We used SPSS 14.0 Data Editor statistical software to calculate mean of ages, sensitivity, specificity, positive and negative predict values and scatters plots, as well as measures of dispersion for this variables and a linear regression between accuracy and patients’ age. We made SROC curves, Forest plots and calculated Likelihood ratios using Metadisc software, in order to make an aggregation of the data. Concordance test- Kappa’s test In order to calculate the agreement between reviewers in the articles’ selection, we used the Kappa’s test. This test measures the quality of the method in what concerns to objectivity and impartiality in the article’s selection. This test is useful as it allow us to understand if the criteria defined were well chosen and also if the methodology followed was the most appropriated [12]. Results Articles characteristics Of 789 potentially relevant publications, 34 met our inclusion criteria. 6 were excluded as they were not found and other 5 had missing data. So, 23 articles were included in this systematic review (Figure 1). The main characteristics of the studies selected are summarized in table 1. All publications were written in English. 14 studies were cohorts, 5 were transversals, 4 were randomized controlled trials and 1 was a prospective study. The studies ranged from 41 to 2193 patients. A total of 12,082 participants were included in our study. 4 789 Articles identified and screened for retrieval 686 Articles without all inclusion criteria 103 Articles retrieved for more detailed evaluation 69 Articles with an exclusion criteria Potentially apropriate 34 articles to be included 6 Articles not found 28 Full articles read 5 Articles excluded (missing data) Analized and extracted data from 23 included articles Figure 1 - Flow diagram for the selection of studies included in this systematic review. 14 articles used BNP test to diagnoses LVD, while 5 used NT-proBNP and 4 used both peptides. 22 studies compared the natriuretic peptides with echocardiography and 1 compared with radionuclide ventriculography. Patients’ characteristics The sum of female patients, from 21 articles of the 23 included, was 6383 (53%) and that of male patients was 4608. Patients´ mean age, of the 21 studies which provided information about their participants’ mean age, ranged from 45 to 75 years old. Among these, 4 studies had a mean age below 60 years old, which corresponds to 17% of the participants involved in these studies. In 14 studies that provided the data about the participants with HF, 1933 patients were ill and 3959 weren’t. The most common symptom was dyspnoea, diagnosed in 7 studies, affecting, in mean, 71% of the participants. Some studies addressed the prevalence of comorbilities, especially hypertension that affected 38% of the patients (19 studies), ischemic heart disease affecting 12% of the patients (5 studies), 17% of the patients had diabetes mellitus (16 studies) and 34% of patients smoked (8 studies). 5 References Nº of Nº of participants female participants Nº of Nº of Mean patients patients with age with antecedents of dyspnoea hypertension Nº of patients smokers Nº of patients with antecedents of diabetes Anguita M. et al 247 116 70 247 158 125 68 Fuat A. et al 246 104 65,7 NR NR NR NR Steg PG. et al 709 392 66,44 709 469 NR 193 Nakamura M. et al 993 513 58 NR 460 128 82 Nakamura M., Sakai T. et al 856 485 65 NR 17 NR NR Bal L. et al 41 NR NR NR NR NR NR Gustafsson F. et al 367 198 68,8 326 68 NR 7 Zaphiriou A. Et al 306 176 74 NR 168 NR 58 Nueller T. et al 251 17 73 NR 141 NR 58 Hedberg P. et al 407 205 75 NR 115 215 31 Dokainish H. et al 122 60 56 52 60 49 54 Nielsen LS. et al 345 169 65 283 NR NR NR Groenning BA. et al 672 382 68,1 219 169 237 43 Ng LL. et al 1331 579 63 NR 322 261 63 Sim V. et al 83 43 72 NR NR NR NR Vay M. et al 2193 2152 73 NR 26 42 12 Balli N. et al 167 48 53,72 NR 26 NR NR Wright SP. et al 305 198 72 149 159 NR 71 Wieczorek SG. et al 1050 NR NR NR 246 NR NR Hobds FD. et al 591 275 45 NR 232 351 68 Maisel A. et al 200 11 65,32 NR 130 NR 68 Yakamoto et al 466 210 65 NR 252 NR 70 Mcclure S. et al 134 50 67 NR 51 NR 24 NR, not reported Table 1 - Patients’ demographics of the studies included. Specificity and sensitivity The specificity ranged from 35% to 98%. In 9 articles analysing BNP with an interval from 19.2 to 100pg/ml, it was demonstrated significant differences in what concerns to specificity. 2 of them demonstrated specificity below 45%, while 3 of them presented specificity above 98%. 6 of 16 studies had specificities lowest than the mean, 77%. In more extreme values of cut-off, above 200pg/ml, the specificity was superior in comparison with lower values of cut-off (beneath 50pg/ml). The sensitivity of the BNP test decreased as the cut-off value erased in a general way. 11 of 16 BNP studies had sensitivities higher than the mean, 76%. The value of sensitivity ranged from 26% to 95%. In the NT-proBNP test, the highest value of sensitivity was 100% and the minimum was 73%. 4 of 10 NT- proBNP studies had sensitivities lowest than the mean, 88%, and 6 in 5 studies which provided the cut-off and the respective value of sensitivity, there’s no constant reason between the augment of cut-off and the sensitivity of the test. The specificity of the NT-proBNP test ranges from 35% to 92%. In 5 studies which describes the cut-off value and the associated specificity, the value of specificity increases with the augment of the cut-off, except in 1 study. 3 of 10 studies had specificities inferior to the mean, 68%. The sensitivities and specificities for both tests are described in the Table 3. Positive and negative predictive value 5 of 10 BNP studies had a negative predictive value inferior to the mean, 85%, and 2 of 8 studies had a positive predictive value inferior to the mean, 92%. 5 of 9 NTproBNP studies had a negative predictive value lowest than the mean, 54%, and 5 of 9 studies had positive predictive value lowest than the mean, 37% (Table 3). Negative predictive value Positive predictive value Specificity Sensitivity Type of peptide BNP NT-proBNP Mean N 0.75663 0.87950 16 10 Std. Deviation 0.175893 Mean N 0.099176 0.76619 0.68150 16 10 Std. Deviation 0.188721 0.193018 0.54091 11 0.37433 9 Std. Deviation 0.361079 0.343924 0.84934 10 0.92125 8 Std. Deviation 0.149808 0.121589 Mean N Mean N Table 3 - Mean of positive and negative predictive values, sensitivity, specificity and their ranges. More than one SROC curve was needed to describe the relationship between the sensitivity and the 1-specificity, because the studies values of sensitivity and specificity for the BNP test were heterogeneous (Figure 2). For the NT-proBNP test no SROC curve was adjusted to the pooling of studies, due to the data’s heterogeneity (Figure 3). 7 Sensitivity 1 SROC Curve Sensitivity 1 Symmetric SROC AUC = 0,8271 SE(AUC) = 0,0491 Q* = 0,7600 SE(Q*) = 0,0446 0,9 0,8 0,8 0,7 0,6 0,6 0,5 0,5 0,4 0,4 0,3 0,3 0,2 0,2 0,1 0,1 0 0,2 0,4 0,6 0,8 0 1 Symmetric SROC AUC = 0,5000 SE(AUC) = 0,0000 Q* = 0,5000 SE(Q*) = 0,0000 0,9 0,7 0 SROC Curve 0 0,2 1-specificity 0,4 0,6 0,8 1 1-specificity Figure 2 – SROC curve of BNP test. Figure 3 - SROC curve for NT-proBNP. Negative Likelihood ratios were heterogeneous (p<0.05), indicating that the wide range of cut-off points are a source of heterogeneity to the evaluation of the accuracy of both BNP and NT-proBNP tests in the diagnosis of LVD (Table 4). Type of Pooled LR-(CI 95%) peptide P value of Pooled LR+ (CI P value of heterogeneity* 95%) heterogeneity* NT-proBNP 0.283 (0.124 - 0.643) 0.000 2.079 (1.250 -3.458) 0.000 BNP 0.386 (0.246 – 0.606) 0.000 4.143 (1.995 – 8,604) 0.000 *p<0.05- statistically significant; CI- confidence interval; REM- random effects model; LR(-) – Negative Likelihood ratio; LR (+) – Positive Likelihood ratio Table 4 – Positive and Negative likelihood ratio of NT-proBNP and BNP tests. An asymmetrical funnel plot is described in the forest plots of both diagnostic odds ratio (DOR) for the BNP and NT-proBNP tests, which suggests the heterogeneity of this tools in the diagnosis of systolic LVD (Figures 4 and 5). Figures 4 and 5- Forest plots of the DOR for BNP and NT-proBNP tests. 8 Accuracy The accuracy of BNP test was calculated in 8 studies. The accuracy ranged from a minimum of 46% to a maximum of 92%. In a cut-off’s interval from 20 to 75pg/ml, the accuracy is inconsistent: 71% (cut-off= 20pg/ml), 46% (cut-off= 50pg/ml), 80% (cutoff=52pg/ml) and 53% (cut off= 75pg/ml). For cut-off values higher than this interval, the values for accuracy were greater and more approached (Figure 6). Figure 6- Scatter plot between accuracy and the cut-off value. Correlations When relating the aging of patients to the accuracy of BNP test, there was a slightest increase in the accuracy, however the results are relatively heterogeneous (Figure 7 and Table 5). Regression between age and accuracy R Adjusted R Std. Error of the Model R Square Square Estimate 1 a Figure 7 - Linear regression 0.500a 0.25 0.167 0.12943 -Predictors: (Constant), mean of ages of the participants Table 5 - Output data. of the relation between the increase of patients’ age and the accuracy of BNP test. 9 Degree of Concordance According to the Kappa’s test result, the degree of concordance between the reviewers ranged from 60% to 95%. In mean, the overall agreement surrounded the 78%. Discussion The diagnostic accuracy of BNP levels for systolic LVD has been recently reviewed by Jaime et al [13]. In this systematic review, based on 52 studies, no tests analyzing the accuracy of the NT-proBNP test were included, no gold standard was demanded as base of comparison for the BNP test and studies with a wide variety of settings were included, such as the emergency department. The studies included in this systematic review were divided according to their reference standard and when this was the systolic LVD, the conclusion was that the diagnostic accuracy of BNP test was poorer than that of studies of heart failure. Jaime et al attributed this to the publication bias which would be the explanation for the heterogeneity of the results and asymmetry of the funnel plots. On the other hand, our systematic review included studies analyzing the NT-proBNP test and the comparison of BNP or NT-proBNP tests to an appropriated gold standard was a criteria required for the inclusion of the study. Our results suggest that the variety of cut-off points is a source of heterogeneity in the accuracy of both tests, as the pooled of negative LR is heterogeneous (p<0.05), which is not considered in the Jaime et al review. Significant limitations of the BNP and NT-proBNP tests were found: there is a wide range of cut-off values; there are considerable differences in the specificity, sensitivity and accuracy values for the same test between studies. As only high and good quality classified studies were included in our systematic review (according to the QUADAS tool), the source of heterogeneity which might explain the variety of sensitivities and specificities for the BNP and NT-proBNP tests possibly can be in the low quality of the methodology used by these studies in points that are not criteria of quality in the QUADAS tool. We can also hypothesize that the main gold standard used, echocardiography, it has itself limitations: it’s dependent on the user, on the patient’s biotype and on the piece of equipment. However it’s worth noting that both BNP and NT-proBNP, as tools for the diagnosis of systolic LVD, appear to have high sensitivity (in mean, 76% for BNP and 88% for 10 NT-proBNP) and negative predictive values (in mean, 92% for the NT-proBNP and 84% for BNP), despite the heterogeneity. These results suggest that both natriuretic peptides might be useful in the ruling out of systolic LVD. Although the number of studies analysing the accuracy of NT-proBNP test it’s lower than those evaluating BNP, NT-proBNP seems to be more sensitive and specific than the BNP test. Our systematic review also faced difficulties: some studies didn’t present all the information necessary for our statistical analysis, making more difficult the carry on of a meta-analysis. This review represents an up-to-date and comprehensive review of primary research investigating the diagnostic accuracy of the natriuretic peptides (BNP and NTproBNP). It describes the problems associated with the conduction of studies heading the evaluation of the accuracy of BNP test in the diagnosis of LVD, when trying to synthesize primary research in this area as a result of clinical and methodological heterogeneity. Conclusion We concluded that there is no consensus in what concerns to the most appropriated value of cut-off. The degree of heterogeneity present in all but a few small sub-groups of our included studies would mean that both the BNP and the NT-proBNP test are not good diagnostic tests to the discrimination between patients with systolic LVD and patients with no systolic LVD, when compared to echocardiography and radionuclide ventriculography. However both BNP and NT-proBNP might be useful in the ruling out of systolic left ventricular dysfunction. Further studies evaluating the accuracy and limitations of brain natriuretic peptides, BNP and NT-proBNP, in the systolic LVD would be necessary to understand these tools’ usefulness in the diagnosis of systolic LVD. References [1] – Ho KK, Pinsky JK, Kannel WB, Levy D. The epidemiology of heart failure: the Framingham Study. 1993 J Am Coll Cardiol; 22: 6A-13A 11 [2] – Bonneaux, L Barendregt JJ, Meeter K, Bonsel GJ, van der Maas PJ. Estimating clinical morbidity due to ischemic heart disease and congestive heart failure: the future rise of heart failure. Am J Public Health,1994 Jan;84(1):20-8 [3] – Hobbs FD, Davis RC, Roalfe AK, Hare R, Davies MK, Reliability of N-terminal proBNP assay in diagnosis of left ventricular systolic dysfunction within representative and high risk populations. Heart. 2004 Aug;90(8):866-70 [4] – Remes J, Miettinen H, Reunanen A, Pyorala K. Validity of clinical diagnosis of heart failure in primary health care. Eur Heart J. 1991 Mar;12(3):315-21. [5] – Stevenson LW, Perloff JK. The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA. 1989 Feb 10;261(6):884-8. [6] – Senior R, Galasko G, McMurray JV, Mayet J. Screening for left ventricular dysfunction in the community: role of and held echocardiography and brain natriuretic peptides. Heart. 2003 Nov;89 Suppl 3:iii24-8 [7] – ACC/AHA/ASE 2003 Guideline Update for the Clinical Application of Echocardiography: summary article. J Am Soc Echocardiography. 2003 Oct;16(10):1091-110. [8] – Sliwa, Karen el at Heart Failure: Making a cardiac failure diagnosis as early as possible. The Medicine Journal, March 2002 [9] – Hulsmann M, Berger R, Mortl D, Gore O, Meyer B, Pacher R, Incidence of normal values of natriuretic peptides in patients with chronic heart failure and impact on survival: A direct comparison of N-terminal atrial natriuretic peptide, N-terminal brain natriuretic peptide and brain natriuretic peptide. Eur J Heart Fail, 2005 Jun;7(4):552-6 [10] – Felker GM, Petersen JW, Mark DB, Natriuretic Peptides in the diagnosis and management of heart failure, CMAJ, 2007 Feb 27;176(5):659. [11] – Whiting P, Rutjes AW, Reitsma JB, Bossuyt PM, Kleijnen J, The development of QUADAS: a tool for the quality assessment of studies of diagnostic accuracy included in systematic reviews. BMC Med Res 2003 Nov 10;3:25. [12] – Harold LK, Polansky M, Measurement of Observer Agreement, Radiology 2003;228:303-308. [13] – Latou-Perez J, Coves-Orts FJ, Abad-Terrado C, Abraira V, Zamora J, Accuracy of B-type natriuretic peptide levels in the diagnosis of left ventricular dysfunction and heart failure: A systematic review, 2005; Eur J Heart Fail, 2006 Jun;8(4):390-9. Epub 2005 Nov 21 12 [14] – Yamamoto K, Burnett JC Jr, Bermudez EA, Jougasaki M, Bailey KR, Redfield MM, Clinical criteria and biochemical markers for the detection of systolic dysfunction, J Card Fail, 2000 Sep;6(3):194-200. [15] – Wieczorek SJ, Wu AH, Christenson R, Krishnaswamy P, Gottlieb S, Rosano T et al, A rapid B-type natriuretic peptide assay accurately diagnoses left ventricular dysfunction and heart failure: a multicenter evaluation, Am Heart J, 2002 Nov;144(5):834-9. [16] – Maisel AS, Koon J, Krishnaswamy P, Kazenegra R, Clopton P, Gardetto N et al, Utility of B-natriuretic peptide as a rapid, point-of-care test for screening patients undergoing echocardiography to determine left ventricular dysfunction. Am Heart J, 2001 Mar;141(3):367-74. [17] – Wright SP, Doughty RN, Pearl A, Gamble GD, Whalley GA, Walsh HJ et al, Plasma amino-terminal pro-brain natriuretic peptide and accuracy of heart-failure diagnosis in primary care: a randomized, controlled trial. J Am Coll Cardiol, 2003 Nov 19;42(10): 1793-800. [18] – Hobbs FD, Davis RC, Roalfe AK, Hare R, Davies MK, Kenkre JE, Reliability of N-terminal pro-brain natriuretic peptide assay in diagnosis of heart failure: cohort study in representative and high risk community populations, BMJ, 2002 Jun22; 324(7352):1498. [19] – Sim V, Hampton D, Phillips C, Lo SN, Vasishta S, Davies J et al, Plasma Btype natriuretic peptide levels and risk factors for congestive heart failure in a Japanese general population. Int Heart J, 2005 May;46(3):465-75. [20] – Bal L, Thierry S, Brocas E, Van de Louw A, Pottecher J, Hours S et al, B-type natriuretic peptide (BNP) and N-terminal-proBNP for heart failure diagnosis in shock or acute respiratory distress, Acta Anaesthesiol Scand, 2006 Mar;50(3):340-7. [21] – Zaphiriou A, Robb S, Murray-Thomas T, Mendez G, Fox K, McDonagh T, The diagnostic accuracy of plasma BNP and NTproBNP in patients referred from primary care with suspected heart failure: results of the UK natriuretic peptide study, Eur J Heart Fail, 2005 Jun;7(4):537-41. [22] - Gustafsson F, Steensgaard-Hansen F, Badskjaer J, Poulsen AH, Corell P, Hildebrandt P, Diagnostic and prognostic performance of N-terminal ProBNP in primary care patients with suspected heart failure, J Card Fail, 2005 Jun;11(5 Suppl):S15-20 13 [23] - Mueller T, Gegenhuber A, Poelz W, Haltmayer M, Diagnostic accuracy of B type natriuretic peptide and amino terminal proBNP in the emergency diagnosis of heart failure, Heart, 2005 May;91(5):606-12. [24] – Hedberg P, Lonnberg I, Jonason T, Nilsson G, Pehrsson K, Ringqvist I, Electrocardiogram and B-type natriuretic peptide as screening tools for left ventricular systolic dysfunction in a population-based sample of 75-year-old men and women, Am Heart J, 2004 Sep;148(3):524-9. [25] – Dokainish H, Zoghbi WA, Lakkis NM, Quinones MA, Nagueh SF, Comparative accuracy of B-type natriuretic peptide and tissue Doppler echocardiography in the diagnosis of congestive heart failure, Am J Cardiol, 2004 May 1;93(9):1130-5. [26] – Groenning BA, Raymond I, Hildebrandt PR, Nilsson JC, Baumann M, Pedersen F, Diagnostic and prognostic evaluation of left ventricular systolic heart failure by plasma N-terminal pro-brain natriuretic peptide concentrations in a large sample of the general population. Heart, 2004 Mar;90(3):297-303. [27] – Ng LL, Loke I, Davies JE, Khunti K, Stone M, Abrams KR et al, Identification of previously undiagnosed left ventricular systolic dysfunction: community screening using natriuretic peptides and electrocardiography. Eur J Heart Fail, 2003 Dec;5(6):775-82. [28] – Vay M, Kirk V, Parner J, Hassager C, Nielsen H, Krogsgaard K, Trawinski J et al, NT-proBNP: a new diagnostic screening tool to differentiate between patients with normal and reduced left ventricular systolic function. Heart, 2003 Feb;89(2):150-4. [29] – Balli N, Georges A, Corcuff JB, Barat JL, Bordenave L, Assessment of brain natriuretic peptide in patients with suspected heart failure: comparison with radionuclide ventriculography data. Clin Chim Acta, 2001 Apr;306(1-2):19-26. [30] – Anguita M, Montes P, Jordan A, Casares G, Gomez I, Recio J et al, Utility of NT-proBNP for diagnosing heart failure in a heterogeneous population of patients with dyspnoea. Spanish multicenter study, Rev Esp Cardiol, 2006 May;59(5):465-72. [31] – Fuat A, Murphy JJ, Hungin AP, Curry J, Mehrzad AA, Hetherington A, Johnston JI et al, The diagnostic accuracy and utility of a B-type natriuretic peptide test in a community population of patients with suspected heart failure, Br J Gen Pract, 2006 May;56(526):327-33. [32] – Steg PG, Joubin L, McCord J, Abraham WT, Hollander JE, Omland T et al, Btype natriuretic peptide and echocardiographic determination of ejection fraction in the 14 diagnosis of congestive heart failure in patients with acute dyspnoea, Chest, 2005 Jul; 128(1): 21-9. [33] – Nakamura S, Naruse M, Naruse K, Kawana M, Nishikawa T, Hosoda S et al, Atrial natriuretic peptide and brain natriuretic peptide coexist in the secretory granules of human cardiac myocytes. Am J Hyperten. 1991 Nov;4(11):909-12. [34] – Nakamura M, Sakai T, Osawa M, Onoda T, Yonezawa S, Okayama A et al, Comparison of positive cases for B-type natriuretic peptide and ECG testing for identification of precursor forms of heart failure in an elderly population, Int Heart J, 2005 May;46(3):477-87 [35] – Nielsen LS, Svanegaard J, Klitgaard NA, Egeblad H. N-terminal pro-brain natriuretic peptide for discriminating between cardiac and non-cardiac dyspnoea. Eur J Heart Fail, 2004 Jan;6(1):63-70. [36] – McClure SJ, Caruana L, Davie AP, Goldthorp S, McMurray JJ, Cohort study of plasma natriuretic peptides for identifying left ventricular systolic dysfunction in primary care, BMJ, 1998 Aug 22;317(7157):516-9. 15