* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download a brief review of the walking time bomb
Dual consciousness wikipedia , lookup
Cortical stimulation mapping wikipedia , lookup
Hereditary hemorrhagic telangiectasia wikipedia , lookup
Neuropsychopharmacology wikipedia , lookup
Expressive aphasia wikipedia , lookup
Brain damage wikipedia , lookup
Vertebral artery dissection wikipedia , lookup
A BRIEF REVIEW OF THE
WALKING TIME BOMB-STROKE
© June 18, 2009, by
Scott Neff, MSIV DC DE IDE IME
CFE DABFE ISPS FFABS FAABT
FFAAJTS –Certified Manipulation
under Anesthesia
STROKE: A MINI REVIEW
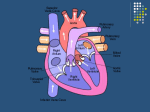
Cerebrovascular diseases include some of the most
common devastating disorders; ischemic stroke,
hemorrhagic stroke, and Cerebrovascular anomalies
such as intracranial aneurysms and arteriovenous
malformations. They cause approximately 200,000
deaths each year in the US and are a major cause of
disability. Stroke is the second most frequent cause of
death in Japan and China and the most common cause
of death worldwide.
The incidence of Cerebrovascular disease increases
with age, and the number of strokes is projected to
increase as the elderly population grows, with a doubling
of stroke deaths in the US by 2030.
STROKE CONTINUED:
Definition: The sudden death of some brain
cells due to lack of oxygen when the blood flow
to the brain is impaired by blockage or rupture of
an artery to the brain. A CVA is also referred to
as a stroke. They are caused by Ischemia (TIA),
Infarction (85%) or Hemorrhage (15%).
Originally the term "stroke" came from the
ancient Greeks and Romans belief that
someone suffering a stroke (or any sudden
incapacity) had been “struck” down by the gods.
Ischemic strokes are classified as thrombotic,
embolic, vasoconstrictive, or veno-occlusive in
etiology. Most hemorrhagic strokes are
hypertensive in etiology. The brain is exquisitely
sensitive to interruptions in blood flow because
neurons have no energy reserve due to the
absence of glycogen, so energy failure is rapid.
Neurologic symptoms begin to develop in as
little as 10 seconds after blood flow is
compromised.
General Clinical Presentation
Symptoms of a stroke depend on the area of the
brain affected. Yet when blood flow is quickly
restored, brain tissue can recover fully and the
patient’s symptoms are only transient; which is
called a transient ischemic attack or TIA.
Typically the neurologic signs and symptoms
of a TIA last for 5 to 15 min but, by definition,
must last < 24 hours. If the cessation of flow
lasts for more than a few minutes, infarction
or death of brain tissue results. Thus stroke has
occurred if the neurologic signs and
symptoms last for > 24 hours.
Hemorrhage causes 15% of
strokes
Epidural
hemorrhage:
Subdural
hemorrhage
Subarachnoid
hemorrhage
Virtually always traumatic.
And usually associated with
skull fracture or stroke.
Tear of dural arteries, most
frequently middle meningeal
artery.
Leads to cerebral herniation
(subfalcine) if not promptly
evacuated.
Lucid interval before loss of
consciousness (“talk and
die syndrome”).
Often traumatic/A Vs A,
CBS - stroke.
Caused by rupture of
bridging veins.
Predisposing conditions:
brain atrophy and abnormal
hemostasis.
Headache, drowsiness,
focal neurological deficits,
and sometimes dementia is
found.
Recurs frequently.
Most frequent cause is
ruptured berry aneurysms.
Less frequent causes;
extension of an
intracerebral or subdural
hematoma, vascular
malformations, trauma,
abnormal hemostasis, and
tumors.
Sudden (“thunderclap”)
headache, nuchal rigidity,
neurological deficits on one
side and stupor.
In depth view of Stroke causation
As noted above, an artery to the brain may be blocked by a clot
(thrombosis) which typically occurs in a blood vessel that has
previously been narrowed due to atherosclerosis ("hardening of the
artery"). When a blood clot or a piece of an atherosclerotic plaque (a
cholesterol and calcium deposit on the wall of the artery) breaks
loose, it can travel through the circulation and lodge in an artery of
the brain, plugging it up and stopping the flow of blood; this is
referred to as an embolic stroke.
A blood clot can form in a chamber of the heart when the heart beats
irregularly, as in atrial fibrillation; such clots usually stay attached to
the inner lining of the heart but they may break off, travel through the
blood stream, form a plug (embolus) in a brain artery and cause a
stroke. A cerebral hemorrhage (bleeding in the brain), from an
aneurysm (a widening and weakening) of a blood vessel in the
brain, also causes stroke.
Diagnosis of Stroke
Involves a medical history and a physical examination.
Tests are done to search for treatable causes of a stroke and help
prevent further brain damage. A CAT scan of the brain is often done
to show bleeding into the brain; this is treated differently than a
stroke caused by lack of blood supply. A CAT scan also can rule out
some other conditions that may mimic a stroke. CT scan is
indicated in the acute stage.
A sound wave of the heart (echocardiogram) may be done to look
for a source of blood clots in the heart. Narrowing of the carotid
artery (the main artery that supplies blood to each side of the brain)
in the neck can be seen with a carotid ultrasound.
Blood tests are done to look for signs of inflammation which can
suggest inflamed arteries. Antiphospholipid antibodies, Cardiac
enzymes and certain blood proteins are tested that are relative to
increasing the chance of stroke by thickening the blood.
MRI may be used with or without contrast media. MRI is indicated
for a sub acute infarct &/or hemorrhage presentation.
Gross vs. Microscopic Changes for Cerebral Infarction
Time
Gross Δ’s
Microscopic Δ’S
0-12 hours
No lasting Δ’s
Minimal or no Δ
12-24 hours
Minimal Δ’s
Red (hypereosinophilc)
neurons with pyknotic nuclei
24-48 hours
Indistinct gray-white
Neutrophilic
infiltrate:
matter junction
2-10 days
Friable
2-3 weeks
Tissue liquefies
3 wk-month
Fluid-filled cavity
demarcated by gliotic scar
Fluid-filled cavity; reactive
astrocytes and lipid-laden
macrophages (glitter cells)
Years
Old cyst surrounded by
gliotic scar
Astrogliosis surrounding a
cyst.
tissue with
marked edema
Histiocytic
infiltrate:
Neuron’s disappear
Liquefactive necrosis;
histiocytes fill with products
of myelin breakdown
Stroke Signs and Symptoms
The most common symptom is weakness or paralysis of one side of
the body with partial or complete loss of voluntary movement or
sensation in a leg or arm. There can be speech problems and weak
face muscles, causing drooling (7th cn compression via stylomasoid
foramin or damage in its brain nucleus, results in mouth drooping
allowing saliva to drip). Numbness or tingling is very common. A
stroke involving the base of the brain can affect balance, vision,
swallowing, breathing and even unconsciousness.
A stroke is a medical emergency. Anyone suspected of having a
stroke should be taken immediately to a medical facility for diagnosis
and treatment. Pts may not seek assistance on their own because
they are rarely in pain and may lose appreciation that something is
wrong (anosagnosia)
Severe Symptoms
Most common severe symptoms are (1) pure
motor hemiparesis of face, arm, and leg (internal
capsule or pons); (2) pure sensory stroke
(ventrolateral thalamus); (3) ataxic hemiparesis
(pons); (4) dysarthria–clumsy hand (pons or
genu of internal capsule); and (5) pure motor
hemiparesis with motor (Broca's) aphasia or
broken speech (internal capsule and adjacent
corona radiata).
Wernickes aphasia vs. Broca’s
aphasia
• Wernicke’s aphasia (temporal lobe lesion/superior
temporal gyrus) aka Receptive aphasia, is a receptive
defect where the patient speaks fluently but the words do
not make sense (Broadmann area 22); sensory
dysprosody - the inability to perceive the pitch, rhythm,
and emotional tone of speech.
• Broca’s aphasia (frontal lobe lesion/inferior frontal gyrus)
aka Expressive aphasia (Broadmann areas 44 and
45) is an expressive deficit where the patient is unable to
verbalize well.
• Wernicke’s aphasia is caused by a disorder of the
posterosuperior temporal gyrus of the languagedominant hemisphere. Often alexia (loss of the ability to
read words) is also present.
• In Broca’s aphasia comprehension and ability to
conceptualize are relatively preserved, but the ability to
create words is impaired. Expressive aphasia is due to a
disorder of the posteroinferior part of the frontal lobe. It
often caused agraphia (loss of the ability to write) and
impairs oral reading.
• Finally our Wernicke’s aphasia patients speak normal words fluently,
yet with meaningless phonemes (t & d are phonemes in English
because they can be used to distinguish between two words, for
example ‘bad’ and ‘bat’ ), not knowing their meaning or
relationships. Thus the words are jumbled and termed “word salid”.
Our patient typically is simply unaware that their speech is
incomprehensible to others. Lastly a right visual field loss commonly
accompanies Werickes’ aphasia as the visual pathway is near the
affected area.
• Whereas our Broca’s aphasia patients can comprehend and
conceptualize relatively well, but their ability to form words is
impaired. Usually producing agraphia (speech production loss)
dysgraphia (writing impairment), anomia (inability to name objects)
and impaired prosody (The varying rhythm, intensity, and frequency
of speech that are interpreted as stress or intonation that aid
meaning transmission ).
Decorticate vs. Decerebrate lesion.
Decorticate lesion is a cortical lesion involving
a loss in posturing relative to (sign of
corticospinal damage) adduction of the arms
and flexion of the elbows, with wrists and
fingers flexed on the chest. The legs are
extended and internally rotated, with plantar
flexion of the feet. This posture may occur
unilaterally or bilaterally. It usually results from a
stroke or head injury.
Decerebrate lesion is a midbrain or lower lesion
involving posturing relative to upper extremity
extension; and flexion and ext rotation of legs.
Watershed and Lacunar infarcts
.
Watershed infarcts occur at border of areas supplied by
different arteries (middle cerebral artery, anterior
cerebral artery), often following prolonged hypotension.
Emboli sources such as carotid atheroma are most
common, cardiac & fat emboli, marantic
ENDOCARDITIS (metastasizing cancer cells).
Watershed infarcts generally are the cause of Transient
ischemic attack (TIA) which again, is a deficit lasting less
then or equal to 24 hours but usually less than one hour
and completely resolves.
Lacunar Syndromes- small infarct in deep white mater,
strongly associated with hypertension and atherosclerosis.
Lacunar syndromes begin with ischemic cerebral
infarction as a result of a vascular occlusion commonly
caused by atherosclerotic thrombi or emboli from cardiac
lesions. The subsequent necrotic area of brain becomes
soft and edematous soon after the injury and after a few
weeks become a cystic space surrounded by scar tissue.
These cystic cavities are called lacunas (Lacuna: Latin,
lake). Lacunar infarcts begin due to hypertensive
changes “in arterioles”. Arteriole small penetrating
branches supply the basal ganglia and deep white
matter. Then leakage of plasma components through
the endothelium and increased production of
extracellular matrix cause arteriolar wall changes. The
end process is called “hyaline arteriolosclerosis”,
which causes narrowing of the vessel lumen and
possible occlusion.
Lacunar Syndromes continued:
1.
2.
3.
4.
Lacunar infarction leads to clinical syndromes
depending on the anatomical portion of the brain
infarcted. These syndromes follow:
Dysarthria-clumsy hand syndrome-Lacunar infarct at
the base of the pons or the genu of the internal
capsule.
Pure sensory stroke-Lacunar infarct in the
ventroposterolateral or ventroposteromedial thalamus.
Pure motor hemiparesis-Lacunar infarct in the
posterior limb of the internal capsule.
Ataxia-hemiplegia syndrome-Lacunar infarct in the
base of the pons.
Treatment for Strokes
•
•
•
•
•
•
•
•
•
Early use of anticoagulants to minimize blood clotting has value in some
patients. Tissue plasminogen activator (tPA) within 3-6 hours of onset
(preferable 1 hour) for occlusive dz only. May prevent serious symptoms.
Intracranial bleeding is an absolute contraindication for tPA use!
Hypertension is the most important controllable risk factor for stroke.
Correct the underlying disorder such as blood pressure that is too high or
too low may be necessary. (Yet lowering elevated blood pressure into the
normal range is no longer recommended during the first few days following
a stroke since this may further reduce blood flow through narrowed arteries
and make the stroke worse.)
The blood sugar glucose in diabetics is often quite high after a stroke;
controlling the glucose level may minimize the size of a stroke.
In other words correct hyperlipidemia, hypertension, diabetes, valve
abnormality, coagulopathy, and atrial fibrillation
For embolic strokes we give aspirin/warfarin anticoagulation for prophylaxis.
If carotid is 70% occluded & patient has symptoms use endarterectomy.
Oxygen is given as needed. New medications that can help oxygen-starved
brain cells survive while circulation is reestablished are being developed.
Rehabilitation:
When a patient is no longer acutely ill after a
stroke, the aim turns to maximizing the patient's
functional abilities. This can be done in an
inpatient rehabilitation hospital or in a special
area of a general hospital and in a nursing
facility. The rehabilitation process can involve
speech therapy to relearn talking and
swallowing, occupational therapy for regaining
dexterity of the arms and hands, physical
therapy for improving strength and walking, etc.
The goal is for the patient to resume as many of
their pre-stroke activities as possible.
Prognosis
• 20-40% mortality at 30 days (20%
atheroemboli, 40% bleed).
• Less then 1/3 of patients achieve full
recovery of lifestyle.
• Atheroembolic strokes occur at 10% per
year.
Differential Diagnosis
Just because a person has slurred speech or weakness
on one side of the body does not necessarily mean that
person has had a stroke. There are many other nervous
system disorders that can mimic a stroke including a
brain tumor, a subdural hematoma (a collection of
blood between the brain and the skull) or a brain
abscess (a pool of pus in the brain caused by bacteria
or a fungus). Virus infection of the brain (viral
encephalitis) can cause symptoms similar to those of a
stroke, as can an overdose of certain medications.
Dehydration or an imbalance of sodium, calcium, or
glucose can cause neurological abnormalities similar to
a stroke. Even Multiple sclerosis can emulate a stroke.
Conclusion:
Clearly, stroke is a devastating disorder which plagues
mankind. However, often overlooked, is the zeal to
maintain a healthy environment to avoid stroke. Patient
education on weight control, blood pressure control,
cholesterol and fatty acid control in combination with
healthy eating, exercise, no smoking and the scheduling
of regular check-ups, is key to avoiding Cerebrovascular
disease. As physicians, it must be our goal to make
each patient their own team captain in maintaining a
healthy lifestyle. Indeed the greatest task for the quality
physician and surgeon. I hope this brief survey of stroke
will help in our continuing and never ending development
as physicians, and the guiding hand to help the public
avoid the disastrous circumstances of Cerebrovascular
disease. Good luck and G-d Bless.
REFERENCES:
•
“Is this patient having a stroke?". Goldstein L, Simel D (2005). JAMA 293 (19): 2391–402.
•
“Classification and natural history of clinically identifiable subtypes of cerebral infarction.”Bamford J, Sandercock P,
Dennis M, Burn J, Warlow C (June 1991). Lancet 337 (8756): 1521–6.
•
“The role of the clinical examination in the sub-classification of stroke.” Bamford JM (2000). "Cerebrovasc. Dis. 10
Suppl 4: 2–4.
•
“Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial
of Org 10172 in Acute Stroke Treatment” Adams HP, Bendixen BH, Kappelle LJ, et al (January 1993).
•
"Rapid ambulance protocol for acute stroke". Harbison J, Massey A, Barnett L, Hodge D, Ford GA (June 1999).
Lancet 353 (9168): 1935. .
•
"Design and retrospective analysis of the Los Angeles Prehospital Stroke Screen (LAPSS)". Kidwell CS, Saver JL,
Schubert GB, Eckstein M, Starkman S (1998). Prehosp Emerg Care 2 (4): 267–73.
•
"Cincinnati Prehospital Stroke Scale: reproducibility and validity". Kothari RU, Pancioli A, Liu T, Brott T, Broderick J
(April 1999). Ann Emerg Med 33 (4): 373–8.
•
“National Institute for Health and Clinical Excellence. Clinical guidelines 68:. London, 2008.
•
"The Recognition of Stroke in the Emergency Room (ROSIER) scale: development and validation of a stroke
recognition instrument". Nor AM, Davis J, Sen B, et al (November 2005). Lancet Neurol 4 (11): 727–34.
•
“Stroke: Hope Through Research”. National Institute of Neurological Disorders and Stroke (NINDS) (1999).
National Institutes of Health.
•
"An evidence-based causative classification system for acute ischemic stroke". Ay H; Furie KL; Singhal A; Smith
WS; Sorensen AG; Koroshetz WJ (2005). Ann Neurol 58 (5): 688–97.
•
"Diagnostic Biomarkers for Stroke: A Stroke Neurologist's Perspective". Hill M (2005). Clin Chem 51 (11): 2001–
2002.
•
“Magnetic resonance imaging and computed tomograpy in emergency assessment of patients with suspected
acute stroke: a prospective compairison” Chalela, J; Kidwell C, Nentwich L et al. (2007). Lancet 369 (9558): 293–
8.
•
“Comparison of MRI and CT for detection of acute intracerebral hemorrhage”. Kidwell, C; Chalela J, Saver J et al.
(2004). JAMA 292 (15): 1823–30.
•
"New evidence for stroke prevention: scientific review". Straus SE, Majumdar SR, McAlister FA (2002). JAMA 288
(11): 1388–95.
•
"Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke
Association Stroke Council: cosponsored by the Atherosclerotic Peripheral Vascular Disease Interdisciplinary
Working Group; Cardiovascular Nursing Council; Clinical Cardiology Council; Nutrition, Physical Activity, and
Metabolism Council; and the Quality of Care and Outcomes Research Interdisciplinary Working Group: the
American Academy of Neurology affirms the value of this guideline". Goldstein LB, Adams R, Alberts MJ, et al
(2006). Stroke 37 (6): 1583–633.
•
"Collaborative meta-analysis of randomized trials of antiplatelet therapy for prevention of death, myocardial
infarction, and stroke in high risk patients". BMJ 324 (7329): 71–86. 2002.