* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Cardiovascular notes File
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Artificial heart valve wikipedia , lookup
Cardiac surgery wikipedia , lookup
Myocardial infarction wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
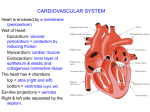
Chapter 13 – Cardiovascular System -consists of heart and blood vessels -beats over 100,000 times per day 2 closed pathways (circuits) of blood flow -pulmonary circuit – sends oxygen-poor blood to the lungs to pick up O2 and drop off CO2 - systemic circuit – sends oxygen-rich blood and nutrients to body cells and removes waste The Heart General Characteristics - located between the lungs in the thoracic cavity - 2/3 on left side, 1/3 on right side - triangular shape - apex – pointed end that touches diaphragm, points left - base – flattened superior margin of heart - size of clenched fist, 14cm x 9 cm Coverings of the Heart - pericardium – double-layered serous membrane that encloses heart and major blood vessels -outer layer called parietal pericardium or pericardial sac - 2 parts 1) thick outer fibrous layer (tough, dense connective tissue; protects heart, anchors heart to diaphragm, sternum, and major blood) vessels attached to heart 2) thin serous layer (thin, squamous epithelium underlaid by connective tissue) - inner layer is called visceral pericardium or epicardium - firmly attached to surface of heart - is both outer layer of heart wall and inner layer of pericardium - pericardial cavity – space between serous layer of parietal pericardium and epicardium -contains fluid secreted by serous cells of pericardium, which reduces friction between the membranes during heart activity -pericarditis – swollen pericardium Heart Wall -3 layers 1) epicardium – thin, protective barrier, contains fat deposits 2) myocardium – makes up most of heart wall, composed of cardiac muscle tissue; cells are arranged in spiral bundles interwoven w/ connective tissue fibers; links all parts of heart together – forms network called the fibrous skeleton 3) endocardium (endothelium) – smooth, white membrane forming inner layer of heart wall, lines internal spaces (chambers) of heart and covers valves; composed of squamous epithelium underlaid by a thin layer of connective tissue; also lines inner layers of blood vessels Heart Chambers (internal spaces) -2 superior atria (singular: atrium) -2 inferior ventricles Atria -receiving chambers for blood entering heart -push blood into ventricles, don’t really “pump” blood b/c walls are very thin w/ little myocardium -auricles – small, ear-like, hollow appendages attached to atria (increase volume slightly) -interatrial septum – divider separating left and right atria -fossa ovalis – oval depression on wall of septum facing the right atrium (what remains of an opening in fetal heart wall (foramen ovale) where blood flowed from right to left atrium to avoid lungs) -right atrium collects incoming blood from the superior vena cava (drains blood from all body regions above heart), from the inferior vena cava (drains blood from body regions below heart), and the coronary sinus (drains blood from the heart wall) -left atrium – collects blood from the pulmonary veins (drain blood from the lungs) Ventricles -provide force necessary (contraction of myocardium) to push blood out of heart, into body, into vessels -left ventricle contains thickest wall necessary to push blood through all vessels of body, except those supplying lungs -trabeculae carnae – irregular folds of muscle lined w/ endocardium, found on inner wall of each ventricle -papillary muscles – slender projections of folds attached to certain valves -interventricular septum – thick muscular divider that internally separates the left and right ventricles (groove on outer surface of heart is known as interventricular sulcus) -coronary sulcus – groove separating atria from ventricles -after ventricles receive blood from atria, right ventricle pumps blood into pulmonary trunk (carries blood to lungs) and left ventricle pumps blood into aorta (carries blood to rest of body) Heart Valves -permit flow of blood in only one direction Atrioventricular (AV) Valves – located between atria and ventricles; consists of 2 or 3 triangular flaps (cusps) that point downward into ventricle -tricuspid valve – 3 cusps, between right atrium and right ventricle -bicuspid (mitral) valve – 2 cusps, between left atrium and left ventricle -cusps of AV valves are dense connective tissue covered by endocardium -chordae tendinae – thin strands of connective tissue that anchor cusps to papillary muscles in walls of ventricles -atrium contracts pushing blood downward through opening in cusps, into ventricles -ventricle contracts, pushing blood upward against cusps, causing them to close -heart murmur – valve defect that prevents complete closure, allowing some blood to enter atrium Semilunar (SL) Valves – 2 located between ventricles and the major blood vessel each empties into -pulmonary valve – between right ventricle and pulmonary trunk -aortic valve – between the left ventricle and aorta -composed of dense connective tissue covered w/ endocardium -both SL valves consist of 3 half-moon shaped cusps that resemble bowls, convex surfaces face ventricle -when ventricle contract, blood is pushed against AV valves, closing them, pushing blood against SL valves, opening SL valves, moving blood through SL valves into vessels -when ventricles relax, the drop in pressure w/in causes SL valves to close, preventing blood from returning to ventricles -heart murmur not as common Blood Flow Through the Heart Blood enters right atrium from the superior vena cava, inferior vena cava and coronary sinus (low in O2 and high in CO2 because it has circulated through the body) Blood moves through the tricuspid valve into right ventricle, through pulmonary valve,into pulmonary trunk ( which divides into many branches) and into the lungs where blood picks up O2 and drops off CO2 Oxygenated blood enters left atrium through the 4 pulmonary veins. -Blood moves through mitral (bicuspid) valve into left ventricle, through aortic valve, into aorta and out to body (except lungs) Supply of Blood to the Heart -Coronary circulation: the flow of the blood through the vessels in the heart wall. Blood Vessels -closed system consisting of arteries, arterioles, capillaries, venules, and veins Arteries and Arterioles *Arteries – vessels that transport blood away from the heart; strong, elastic tubes that begin as major arteries of the heart (aorta, pulmonary trunk) - get thinner as they move farther away from heart and eventually are classified as arterioleshave thinner walls, average diameter of .5mm -3 layers of artery walls surrounding lumen – hollow interior 1) tunica intima – inner layer, made of endothelium surrounded by basement membrane (connective tissue) rich in elastic fibers 2) tunica media – thick smooth muscle layer w/ elastic fibers 3) tunica adventitia – outer layer – thin connective tissue layer that anchors artery to surrounding structures - tunica media provides elasticity and contractility -vasomotor fibers – nerve fibers that stimulate smooth muscles in vessels to contract -vasoconstriction – when muscles in vessels contract and lumen diameter decreases -vasodilation – when muscles in vessels are relaxed and lumen is normal size -arterioles have the same 3 layers as arteries, but thinner and smaller, eventually walls consist of only endothelium, a thin layer of smooth muscle, and an outer sheet of connective tissue Capillaries -smallest vessels in body, average diameter of .01mm (1 layer endothelium, 1 layer outer connective tissue); allows only 1 RBC to pass through at a time -permit exchange of nutrients and gases between blood and interstitial fluid b/c they are so thin -endothelium of capillary walls acts as a semipermeable membrane barrier which allows regulated movement of materials by diffusion, osmosis, facilitated diffusion, and active transport -gases, ions, and waste diffuse in and out of bloodstream -kidneys and small intestines have larger pores -blood-brain barrier has small or no pores -most capillaries have intermediate size pores which allow fluid from bloodstream to move outside cells into interstitial fluid -connect arteriole to venule -usually form branching network called capillary bed (10-100 capillaries per bed) consisting of thoroughfare channels directly connect arteriole to venule -precapillary sphincter – small band of smooth muscle that surrounds the origin of a branching group of capillaries; acts as a valve to regulate blood flow into those capillaries Venules and Veins -blood move from capillaries to venules after change of materials -venules increase in size as they merge together to form veins; walls get thicker as they get closer to the heart *Veins – transport blood toward the heart -walls of veins are thinner than artery walls and lumens are larger -less smooth muscle makes veins less elastic and contractile than arteries -veins can hold more blood b/c of larger lumen diameters (65% of body’s blood at one time) -usually only partially filled w/ blood and slightly collapsed -distensibility – walls expand (veins fill completely) – allows for variations in blood pressure -veins have one-way valves that form folds in the tunica intima (resemble SL valves of the heart) -frequent in veins of lower limbs, which must return blood to the heart against the force of gravity -varicose veins – veins w/ weakened valves causing blood to pool below them, causing vein walls to become overstretched -hemorroids – varicose veins in the anal canal -other mechanisms for moving blood through veins: 1) respiratory pump – activated when you inhale b/c pressure increases w/in abdomen, squeezing local veins pushing blood up 2) skeletal muscle pump – skeletal muscles surrounding veins contract and relax during body movement, pushing blood up -venous sinuses – veins specialized for storing blood; flattened w/ very thin walls composed of only endothelium; supported by surrounding tissue (not other tunica layers) Blood Pressure -force exerted by blood against inner walls of vessels; keep blood moving -clinically, refers to arterial pressure in major branches of aorta -BP lower in veins b/c other factors influence blood flow in veins (valves, respiratory action, and skeletal muscle activity) -BP also lower in capillaries and venules causing blood to move slower Arterial BP -blood flows from higher to lower pressure areas -highest pressure region is the aorta due to pumping action of heart, which pushes a large volume of blood through aorta -elastic walls of aorta stretch to accommodate surge of blood and pressure reaches maximum value, called systolic pressure (peak – average is 120 mm Hg) -blood leaves aorta, moves through arteries, down pressure gradient into smaller vessels -aorta walls recoil to original shape and aortic pressure drops to lowest point (70-80 mm Hg), called diastolic pressure or ventricular diastole (relaxation) -measuring BP uses a sphygmomantometer -cuff is wrapped around arm over brachial artery -air is pumped into cuff, which eventually compresses brachial artery to the point where no blood can pass -release valve is opened slightly releasing pressure in cuff and allowing small amount of blood to pass through -stethoscope detects sound when blood 1st squeezes through artery systolic pressure -more blood spurts through artery making a louder noise; no more noises are detected when blood flows normally -1st silent moment diastolic pressure -tapping noises called Korotkoff sounds and represent turbulent blood flow through artery Pulse -artery walls expand and recoil the same way that the aorta walls do -pulse – rhythmic expanding and recoiling of an arterial wall near skin surface; usually taken in radial artery in wrist or common carotid artery in neck -pulse rate = heart rate (# of pulses counted = # of heartbeats) b/c each pulse wave is generated by contraction of heart -average resting heart rate for adults is 70-90 beats per minute (bpm) -children is 80-140 bpm; higher b/c of higher metabolic rate -adult pulse over 100 bpm is called tachycardia -adult pulse rate below 60 bpm is called bradycardia Factors affecting blood pressure 1) cardiac output = heart rate x stroke volume -change in how fast the heart beats or how strongly ventricles contract (which affect how much blood enters aorta) changes BP -when increased, BP increases -when decreased, BP decreases 2) Peripheral Resistance -friction produced by blood as it contracts vessel walls, which slows blood flow -largely determined by diameter of lumen in vessel -smaller lumen= more resistance -thicker blood = more resistance -vasoconstriction – shrinks lumen diameter = more resistance -vasodilation = less resistance - increase in PR – increase in BP - deacrease in PR – decrease in BP -arteriole diameter changes account for the most important influence on BP in the body 3)Blood Volume -measure of the amount of plasma and formed elements are in cardiovascular system -healthy = 5 liters -changing amount changes BP -injury and blood loss immediately lowers BP Regulation of BP 1) Nervous system controls -achieved by adjusting cardiac output and PR -nerve impulses may speed up or slow down heart rate -vasomotor fibers constrict or relax smooth muscles in tunica media of vessel walls -baroreceptors detect changes in BP and send message to medulla oblongata in brain 2) Hormonal controls -norepinephrine (NE), epinephrine (E), atrial natriuretic factor (ANF), antidiuretic factor (ADF) -NE and E are secreted by adrenal medulla in times of stress, stimulate fight-or-flight response -E increases cardiac output by stimulating heart rate and increases PR by promoting arteriole vasoconstriction -NE also increases PR -ANF is secreted by atria of heart, reduces blood volume, which decreases BP (causes kidneys to excrete more water from body, which can cause dehydration) -ADF is produced by hypothalamus and stimulates kidneys to conserve water increasing blood volume and increasing BP 3) Kidney controls – long term BP control -use water conservation or excretion -release special chemicals -when BP drops, kidney cells release the enzyme renin, which triggers another chemical called angiotensin II, which is a strong vasoconstrictor – it also stimulates releasal of hormone aldosterone which stimulates sodium absorption by kidneys, causing more water to be absorbed