* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Pulmonary circulation
Survey
Document related concepts
Transcript
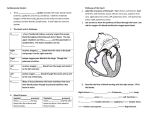
Pulmonary circulation High pressure low flow circulation: Bronchial vessels. Empties into pulmonary veins and enter left heart. Left atrium input, and left ventricle output are about 1-2% grater than that of right ventricular output. Low pressure high flow circulation: Rt. Ventricle-Pulmonary artery arterial branches alv. capill. Veins Lt. atrium Lymphatics: From supportive tissue spaces coursing to hilium of lungs and into right thoracic lymph. Duct. Helping to prevent pulmonary edema Pulmonary circulation Physiological anatomy: the Artery is 5cm thin (1/3 of aorta diameter) , while the branches are short and have more diameter so it will have a large compliance (7 ml/mmHg). pulmonary veins are thin & short. bronchial arteries originate from the systemic circulation (carry 1-2% of C.O -oxygenated blood-) then empty into pulmonary veins then to the left atrium so the left ventricle pumps 1-2% more than the right ventricle. rich lymphatic drainage to the right thoracic duct to prevent edema Pressures in the pulmonary system: 1- right ventricle: 25-1 mmHg 2- pulm. Artery: 25-8 mmHg 3- pulm. cap. : 8 mmHg 4- left atrium & major veins: 2 mmHg Blood volume of the lungs: : 450 ml ( 9% of total blood volume) 70 ml are found in the capillaries Blood volume of the lungs if the person is bleeding or blowing air out hardly the volume can reach 200 ml. if blow out air hard if the person has left heart failure or mitral valve stenosis or regurgitation the volume can reach 900 ml Blood flow Effect of alveolar [O2]: when [O2] decreases below 70% of normal alveolar epithelial cells secrete vasoconstrictors adjacent blood vessels constrict blood flows to better aerated alveoli (extreme low [O2] 5x resistance) Effect of hydrostatic pressure: in normal upright adult there’s a difference between the lowest and highest points of the lung the gradient is 23 mmHg (15 mmHg above the heart & 8 mmHg below it) Regional pulmonary blood flow : 1-Zone 1: No blood flow (capill. pr. < alveol, pr.) - Pts. Breathing against positive pr. - Sever blood loss. 2-Zone 2: Intermittent blood flow 3-Zone 3: Continuous blood flow. (capill. pr. > alveol. pr.) in normal lungs zone 1 cannot be found, zone 2 is in the apex of the lung and zone 3 represents the base. Regional pulmonary blood flow : arterial pressure in pulmonary artery is 25-8 mmHg at apex systolic 25-15= 10 mmHg during diastole 8-15 mmHg= -7? if the person is lying down or exercising only zone 3 can be seen. The effect of increasing C.O on pulmonary blood flow during exercise: blood flow increases by 4-7 folds through: 1- increasing the # of open capillaries 2- distending all the capillaries to increase the flow rate in each one of them. 3- increasing pulm. Arterial pressure normally 1 & 2 are enough to cause significant decrease in resistance 3 is not significant to conserve the energy of the right heart & to prevent edema Pulmonary capillary dynamics: 7 mmHg cap. Pressure. blood passes through the capillary in 0.8sec increasing the C.O lowers the time to 0.3sec Capillary fluid exchange dynamics: lungs Systemic cir. Capillary pressure 7 mmHg 17 mmHg Interst. Osm. Pr. 14 mmHg 8 mmHg Interst. Neg. pr. -8 mmHg -3 mmHg outward forces= 7+14+8 = 29 mmHg inward forces = 28 mmHg mean filtration pr. = 1 mmHg “handled by lymph” Pulmonary edema Alveoli are always dry except for a small amount of fluid secreted by alveolar cells on the alveolar surface. When interstitial pressure becomes (+) water will fill the alveoli Causes: 1- Left-sided heart failure ↑ venous+cap. pr 2-Damage to the pulmonary capillary membrane caused by : a- infections b- breathing chlorine gas or sulfur oxide gas. Safety factors 21 mmHg in acute states 35 mmHg in chronic cases