* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Module 4 - 4.05 MB
Survey
Document related concepts
Transcript
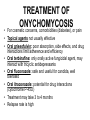
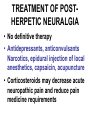
THE SKIN SHOW “Critters VS the Hide Module #4 Ed Vandenberg, MD, CMD Geriatric Section OVAMC & Section of Geriatrics 981320 UNMC Omaha, NE 68198-1320 [email protected] Web: geriatrics.unmc.edu 402-559-7512 All photos were reprinted with permission from the American Academy of Dermatology. All rights reserved. Slides adapted with permission from GRS 5th edition: Dermatologic diseases and disorders PROCESS Series of 4 modules and questions on Etiologies, Evaluation, & Management Step #1 Power point module with voice overlay Step #2 Case-based question and answer Step #3 Proceed to additional modules or take a break Objectives Upon completion the learner will be able to 1. Identify common infectious dermatologic diseases in the elderly. 2. List treatment modalities for common infectious dermatologic diseases in the elderly What’s this? Candidiasis ( intertrigonal) Intertrigonal: commonly found in the web space between the 4th and 5th toes. Moist erythema, maceration and superficial erosion is apparent. More common in older adults because of increased skin folds from decreased dermal elasticity Often associated with secondary candidal or mixed bacterial colonization TREATMENT OF INTERTRIGO • Keep area dry, open to air • Use topical antifungal powder or lotion (eg, 2% miconazole powder or 1% clotrimazole lotion) • Use mild topical corticosteroid occasionally to reduce inflammation What’s this? Answer: Candidiasis • rash may resemble intertrigonal but have peripheral satellite papules and pustules • At risk: older persons with decreased mobility, increased skin moisture or friction, poor hygiene, diabetes mellitus • Oral thrush may develop in those on corticosteroid inhalers, antibiotics, immunosuppressants, or with concomitant illness (diabetes) CANDIDIASIS • Diagnosis: KOH preparation reveals spores and pseudohyphae • Treatment: • Keep skin dry • Improve hygiene • Use topical or oral anticandidal agents (1% clotrimazole lotion, nystatin, ketoconazole) What’s wrong with the nails? Answer: Onychomycosis often yellow, thickened, and friable, with yellow-brown debris under the nail plate. Causes: dermatophytes, yeasts, and nondermatophytic molds Often preceded by or concomitant with tinea pedis Diagnose by KOH preparation or fungal culture TREATMENT OF ONYCHOMYCOSIS For cosmetic concerns, comorbidities (diabetes), or pain • • Topical agents not usually effective • Oral griseofulvin: poor absorption, side effects, and drug interactions limit adherence and efficiency • Oral terbinafine: only orally active fungicidal agent, may interact with tricyclic antidepressants • Oral fluconazole: safe and useful for candida, well tolerated • Oral itraconazole: potential for drug interactions (cytochrome P-45O) • Treatment may take 3 to 4 months • Relapse rate is high What’s this? Answer: HERPES ZOSTER • Prodrome: pain, burn, itch, dull ache • Grouped clusters of vesicles and pustules on an erythematous base involving a dermatome. • More than 2/3 of cases occur in persons aged 50 or older • Incidence is 20 to 50 times higher among immunosuppressed patients Ddx: -Herpes simplex; -Dermatitis herpetiformis -Allergic contact dermatitis HERPES ZOSTER • Most important reason for varicella zoster virus (VZV) reactivation is senescence of the cellular immune response to VZV with increasing age • Reactivation also associated with HIV, malignancy, use of immunosuppressive drugs COMPLICATIONS OF ZOSTER • Involvement of ophthalmic branch of trigeminal nerve • Requires careful ophthalmic monitoring • Hutchinson’s sign: vesicles on the tip of the nose represents involvement of nasociliary branch • Ramsay-Hunt syndrome (involvement of facial or auditory nerves) • Presents as herpes zoster of external ear or tympanic membrane • Leads to facial palsy with or without tinnitus, vertigo, and deafness • Pain can precede, co-exist, or persist after rash • Post-herpetic neuralgia: pain that persists or appears after rash has healed > 30 days after onset of rash • Occurs in 70% of those ≥ 70 • Prevention and education more effective than treatment DIAGNOSIS OF HERPES ZOSTER • Tzanck smear from base of vesicle shows multinucleated giant cells and epithelial cells containing intranuclear inclusion bodies • Smear can be sent for direct fluorescent antibody staining • Definitive diagnosis by viral culture TREATMENT OF HERPES ZOSTER • If intact immunity, herpes zoster is usually self-limited • Treatment should start within 72 hours of rash • Acyclovir 800 mg, 5x / day for 7 to 10 days • Valacyclovir ( Valtrex) 500 mg tid X 10 days • Famciclovir (Famvir) 500 mg tid x 7 days • Early treatment: 1)halts progression of disease, 2) increases rate of clearance of virus from vesicles, 3) decreases incidence of visceral and cutaneous dissemination, 4) decreases ocular complications when eye is involved, may decrease pain and incidence of post-herpetic neuralgia • Wet compresses(Burrow’s)/topical antibiotics can treat secondary bacterial infection TREATMENT OF POSTHERPETIC NEURALGIA • No definitive therapy • Antidepressants, anticonvulsants Narcotics, epidural injection of local anesthetics, capsaicin, acupuncture • Corticosteroids may decrease acute neuropathic pain and reduce pain medicine requirements What’s this? 77 yo male homeless with diffuse pruritus, erythematous rash with scabs. Answer; SCABIES Symptoms include severe pruritus (esp. of hands, axillae, genitalia, and periumbilical region), Signs: erythematous, crusted papules, and linear burrows • Infestation of mite Sarcoptes scabiei • Common in institutionalized older persons; epidemics occur in long-term-care facilities • Eradication can be difficult • Spread by person-to-person contact Ddx; - Lichen simplex chronicus -Atopic dermatitis -Flea or insect bites -Pruritus of systemic disease SCABIES • Diagnosis: scraping of suspected lesion (mite excreta, eggs or mite may be seen) • Treatment often initiated when clinical suspicion of infestation is strong • Treatment: • Topical permethrin 5% or lindane ( Kwell) 15 cream • Re-treat in 1 week if itching and lesions persist • Launder bed linens and clothing in hot water • May use topical corticosteroids for pruritus • Pruritus may persist for weeks to months The End of “Skin Show” Module Four Thank you for Your kind Attention !! Ed Vandenberg MD CMD Section of Geriatrics 981320 UNMC Omaha NE 68198-1320 [email protected] Web: geriatrics.unmc.edu post-test • A 74-year-old man with diabetes mellitus and hypertension has onychomycosis of most nails on each foot confirmed by potassium hydroxide (KOH) staining and fungal culture of nail scrapings. In addition to having cosmetic concerns, the patient finds that the crumbling, thickened nails are causing discomfort and difficulty in his routine foot care. His current medications are glyburide 10 mg twice daily and enalapril 5 mg daily. • What is the most appropriate therapy for this patient? What is the most appropriate therapy for this patient? A. Griseofulvin 500 mg daily B. Ketoconazole 200 mg daily C. Itraconazole 200 mg daily D. Terbinafine 250 mg daily Used with permission from: Murphy JB, et. al. Case Based Geriatrics Review: 500 Questions and Critiques from the Geriatric Review Syllabus. AGS 2002 New York, NY Answer:D. Terbinafine 250 mg daily The most appropriate treatment for this patient is terbinafine, a fungicidal agent especially useful for onychomycosis. Terbinafine is an orally active allylamine derivative with a high potency against dermatophytes. It is well absorbed from the gastrointestinal tract and metabolized in the liver. Its effect is cytochrome P-450independent. Terbinafine is generally well tolerated, with occasional gastrointestinal side effects and the rare serious skin reaction. The treatment is with one tablet daily for 6 weeks for fingernail infections and for 3 months for toenail infections. Recurrence rates are below 10%. • Itraconazole is also effective against dermatophytes and is likewise readily absorbed from the gastrointestinal tract. Daily doses of 200 mg of itraconazole for 6 to 8 weeks for fingernails and 3 to 4 months for toenail mycoses have cure rates of 80% to 90%. Recurrence rates are below 10%. Itraconazole does affect drugs metabolized by the cytochrome P-450 3A system and can cause severe hypoglycemia in patients who are taking oral hypoglycemic agents, as is the case with this patient, for whom terbinafine would thus be a better choice. • Ketoconazole, the first orally active broadspectrum antimycotic drug, has been abandoned for this indication because of idiosyncratic hepatic side effects. Griseofulvin is a safe systemic treatment for onychomycosis but has very low cure rates, about 50% to 60% for fingernails and 20% for toenails. Recurrence rates with use of griseofulvin approach 100%. end