* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download 10- Hypertension, heart failure and regulation of blood flow
Coronary artery disease wikipedia , lookup
Heart failure wikipedia , lookup
Lutembacher's syndrome wikipedia , lookup
Myocardial infarction wikipedia , lookup
Jatene procedure wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
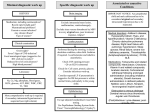
10- Hypertension, heart failure and regulation of blood flow. Hypertension: It is a sustained elevation of the systemic arterial pressure. The increased pressure leads to damage the heart and other organs because of the added stress to the blood vessels. The British Hypertension Society has defined range of blood pressure which falls within the normal range and those that indicate hypertension (table 4). Table (4): The BP in normal person and hypertension. Type SBP (mmHg) DBP (mmHg). Optimal < 120 < 80 Normal < 130 < 85 High normal 130 – 139 85 – 90 Mild hypertension 140 – 159 90 – 99 Moderate 160 – 179 100 – 109 hypertension Sever hypertension ≥ 180 ≥ 110 SBP = Systolic blood pressure. DBP = Diastolic blood pressure. There are two types of hypertension: 1- Essential hypertension: The cause of this type is unknown. More than 90 % of all cases of hypertension are essential hypertension. It has a strong hereditary tendency. 2- Secondary hypertension: The cause of this type is known. 1- Renal disease (e.g. polycystic kidney disease, glomerulonephritis, and renal artery stenosis). 2-Endocrine dysfunction (e.g. Cushing's syndrome, acromegaly). 3-Drugs (e.g. oral contraceptives, anabolic steroids, corticosteroids and sympathomimetic agents). 4- Coarctation of the aorta. Pulmonary hypertension occurs when pulmonary vascular resistance increases. Pulmonary hypertension is commonly associated with pulmonary disease. During pregnancy, many patients develop hypertension (toxemia of pregnancy), in which, there is thickening of the kidney glomerular membranes (autoimmune process), reduce rate of fluid filtration from glomeruli into renal tubules. Effect of hypertension: 1- Left ventricular failure. 2- Renal failure. 3- Rupture a major blood vessel. 4- Retinal damage. Even moderate elevation of the arterial pressure for long time leads to shortened life expectancy. In severe high pressure, a person can expect to live no more than a few more years unless appropriately treated. Treatment of essential hypertension: 1- General measurement: a- Correction of obesity & alcohol intake. b- Restricting salt intake. c- Regular physical exercise. d- Increase consumption of fruit and vegetable. e- Stop smoking and saturated fat may reduction of cardiovascular diseases risk. 2- Drugs: A- Drugs that increase renal blood flow (vasodilator drugs). B- Drugs that decrease tubular reabsorption of salt and water (diuretics). Response to an increase in arterial pressure: The baroreceptors in the carotid sinus and the aortic arch are stimulated; informations are transmitted through glossopharyngeal nerve (CN IX) and vagus nerve (CN X) to nucleus tractus solitarus of medulla (VMC). Cardiovascular center is stimulated to reduce arterial pressure back to normal; these responses include an increase in parasympathetic outflow to the heart to reduce heart rate and decrease the sympathetic outflow to the heart and blood vessels. Heart failure (HF): Pathogenesis: The heart failure (HF) is due to: 1-Chronic hypertension. 2-Myocardial infarction. 3-Arteriovenous fistula. 4- Thyrotoxicosis and thiamin deficiency. The heart fails to putout adequate amount of blood and fails to handle all the blood return to it. The ejection fraction becomes low as 20% instead normal value of 65 %. Diastolic dysfunction reduces ventricular filling in diastole, causing venous congestion. At first cardiac output is an inadequate only during exercise but later it is an inadequate at rest. The inadequate filling of the arterial system triggers baroreceptormediated to increase sympathetic activity with renal vasoconstriction and increased secretion of rennin and aldosterone. Aldosterone causes marked Na and water retention, which add to venous congested and edema. Manifestation: The manifestations of HF range from sudden death due to ventricular fibrillation or air embolism to chronic congestive HF. The terms forward and backward failure are used to refer manifestations produced by systolic and diastolic dysfunction respectively. The manifestations of heart failure are illustrated in table 5: Table (5): Summary of the signs, symptoms and pathogenesis of heart failure. Abnormality Causes Weakness Ankle and sacral edema. Forward failure, COP inadequate to perfuse muscles. Backward failure of right ventricle, increased venous pressure, increased fluid transudation. Increased venous pressure, increased resistance to portal flow. Backward failure of left ventricle, increased pulmonary venous pressure, pulmonary venous distention and transudation of fluid into air spaces. Failure of left ventricle output to rise during exercise, increased pulmonary venous pressure. Probably sudden failure of left heart output to keep up with right heart output, acute rise in pulmonary venous and capillary pressure transudation of fluid into air space. Normal pooling of blood in lung in supine position added to already congested pulmonary vascular system, increased venous return, not putout by left ventricle (relieved by sitting up, raising head of bed, lying on extra pillows. Greater ventricular end-diastolic volume. Hepatomegaly Pulmonary congestion Dyspnea on exertion Paroxysmal dyspnea, pulmonary edema Orthopnea Cardiac dilatation Treatment: 1-To improving cardiac contractility. 2- Inhibition of the production of angiotensin II with angiotensinconverting enzyme inhibitors. 3- To reduce the circulating aldosterone level. 4- Reducing venous tone with nitrates, to reduce the amount of blood return to the heart (lowering the preload). 5- Diuretics are used to reduce the fluid overload. Regulation of blood flow 1- Local mechanism (intrinsic control): Autoregulation is the capacity of tissue to regulate their own blood flow. Blood flow to an organ remains constant over a wide range of perfusion pressures. The capacity is well developed in the kidneys, but it has been observed in the mesentery, skeletal muscles, brain, liver and myocardium. A- It is probability due to in part to intrinsic contractile pressure of smooth muscle to stretch (myogenic theory) of autoregulation. As pressure rises, the blood vessels are distended and vascular smooth muscle fibers that surround the vessels contract. B- Vasodilator substances tend to accumulate in active tissue and these metabolites also contribute to autoregulation (metabolic theory). When blood flows decrease the blood vessels dilate due to accumulation of vasodilator substances. When blood flow increase, the vasodilator substances are tend to be washed away, They include decrease in O2 tension and pH which lead to relax of arterioles and precapillary sphincters. Increase in CO2 which have direct dilatation in skin and brain. Rise in temperature exerts vasodilation effect due to the increase metabolism. K+ ions have dilator activity secondary to hyperpolarization of vascular smooth muscle cells. Adenosine may play a vasodilator role in cardiac vessels but not in skeletal muscle vessels due to inhibit the release of norepiphedrin. Lactate may also contributes to dilatation. In the injured tissue histamine release from damaged cells which increase capillary permeability. Active hyperemia: Blood flow to an organ is proportional to its metabolic activity. Reactive hyperemia: It means increase in BF to an organ after a period of occlusion of blood flow. The longer period of occlusion, greater increase in blood flows. A drop in tissue temperature causes vasoconstriction and this local response to cold plays a part in temperature regulation. Injured arteries and arterioles constrict strongly. The constriction appears to be due in part the local liberation of serotonin from platelets that stick to the vessel wall in the injured area. II- Systemic mechanism (extrinsic control): 1-Nervous system: It regulates blood flow via vasomotor center (VMC) figurer 46 through: A- Sympathetic discharge to small arteries and arterioles (vasoconstriction) for changing the rate of blood flow. B- Sympathetic discharge to adrenal gland to secrete both epinephrine and Norepinephrine into circulation. These two hormones act directly on the blood vessels to cause vasoconstriction and decrease blood flow. C- Parasympathetic discharge and inhibition the tonic discharge of sympathetic nerves produce vasodilation to increase blood flow. Figure (46):Vasomotor center (VMC) 2- Humoral system: Many circulating hormones affect the vascular system: A- Vasoconstrictor agents such as Epinephrine, nor-epinephrine, angiotensin II and vasopressin (ADH). B- Vasodilator agents such as histamine, kinin, vasoactive intestinal peptide (VIP), and atrial natriuretric peptide (ANP). Endothelial cells: They play a major role in the control of blood flow in many organs. They release vasodilator substances such as bradykinin, Endotheliumderived relaxing factor that is now known nitric oxide (NO). It Also they release vasoconstriction substances such as endothelin, and prostaglandin. Endothelin-1 is the most potent vasoconstrictor agent.