* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download bacterial-infection-of-vzv-treatment
Globalization and disease wikipedia , lookup
Common cold wikipedia , lookup
Hygiene hypothesis wikipedia , lookup
Childhood immunizations in the United States wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Gastroenteritis wikipedia , lookup
Urinary tract infection wikipedia , lookup
Clostridium difficile infection wikipedia , lookup
Multiple sclerosis research wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Rheumatic fever wikipedia , lookup
Sociality and disease transmission wikipedia , lookup
Onchocerciasis wikipedia , lookup
Antimicrobial peptides wikipedia , lookup
Neonatal infection wikipedia , lookup
Infection control wikipedia , lookup
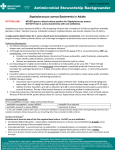
Bacterial superinfection of chicken pox: Best antibiotic to use? Joshua Burns & Megan Collins Paediatric varicella hospitalisations in France: a nationwide survey1 • 1575 patients hospitilised between March 2003 and July 2005 • From 200 paediatric wards across France • Median age was 2 years, 87.5% were <5 years, and 2.7% were neonates • Based on national surveillance network data Results • Skin/soft tissue infection was most common complication (36.5%) • Other common complications: Neurologic (8.1%), febrile seizures (6.4%), bacterial pneumonia (3.1%), ENT (2.9%), varicella pneumonia (2.4) Results (continued) • A pathogen was identified in 268 cases of skin/soft tissue superinfection - 158 were Staphylococcus Aureus (59%) - 88 were Group A Beta-haemolytic streptococci (33%) - 14 were Staph. Aureus + Group A strep (5%) • 97% cases were Staph. Aureus or Group A Strep. Strengths Weaknesses • Correct demographics (age-range, hospitilised) • Retrospective study • Sufficient sample size • Methods for how organism was determined are unclear in paper • Recorded all complications Disease manifestations and pathogenic mechanisms of Group A Streptococcus2 • Narrative review • American Society for Microbiology – Clinical Microbiology Reviews • ‘Group A Strep remains exquisitely and universally sensitive to penicillin’ • Suggests use of beta-lactam antibiotics for group A strep • Clindamycin, macrolides and cephalosporins all also appropriate Antimicrobial Activities of Ceftaroline and Comparator Agents against Bacterial Organisms Causing Bacteremia in Patients with Skin and Skin Structure Infections in U.S. Medical Centers, 2008 to 20143 • Bacteria collected as part of Assessing Worldwide Antimicrobial Resistance Evaluation (AWARE) • Skin infections that have progressed to bacteraemia • In adult population • Included 670 Staph. Aureus and 138 Beta-haemolytic Streptococci Staphylococcus Aureus (670) Antibiotic % Susceptibility Beta-haemolytic streptococci (138) Antibiotic % Susceptibility Ceftaroline 97.9 Ceftaroline 100 Ceftriaxone 49.4 Ceftriaxone 100 Oxacillin 49.4 Penicillin 100 Clindamycin 82.4 Clindamycin 84.8 Daptomycin 99.7 Daptomycin 100 Erythromycin 39.0 Erythromycin 71.0 Levofloxacin 59.0 Levofloxacin 99.3 Linezolid 99.9 Linezolid 100 Tetracycline 95.8 Tetracycline 44.9 Tigecycline 100 Tigecycline 100 Vancomycin 100 Vancomycin 100 Skin and soft tissue infections in Latin American medical centers: four-year assessment of the pathogen frequency and antimicrobial susceptibility patterns4 • Antimicrobial susceptibility of isolates collected from skin and soft tissue infections during the first 4 years (1997-2000) of the SENTRY Antimicrobial Surveillance Program • Staphylococcus Aureus in 32.8% Staphylococcus Aureus (584) Antibiotic % Susceptibility Penicillin 5.3 Co-amoxiclav 71.6 Tetracycline 71.2 Chickenpox in adults - Clinical management5 “Secondary bacterial infection with Staphylococcus aureus or Group A Streptococci is a common complication of chickenpox … treatment with appropriate antibiotics, such as flucloxacillin, co-amoxiclav or a macrolide should be considered.’’ Conclusions • Superinfected chicken pox lesions most likely to be Group A Streptococcus or Staphylococcus Aureus • Literature consensus is that Group A strep. is susceptible to penicillin antibiotics, including co-amoxiclav • Co-amoxiclav seems to be good choice for most but not all of Staph. Aureus strains References 1 Grimprel E, Levy C, de La Rocque F, Cohen R, Soubeyrand B, Caulin E, Derrough T, Lecuyer A, d'Athis P, Gaudelus J. Paediatric varicella hospitalisations in France: a nationwide survey. Clinical microbiology and infection. 2007 May 1;13(5):546-9. 2 Walker MJ, Barnett TC, McArthur JD, Cole JN, Gillen CM, Henningham A, Sriprakash KS, Sanderson-Smith ML, Nizet V. Disease manifestations and pathogenic mechanisms of group A Streptococcus. Clinical microbiology reviews. 2014 Apr 1;27(2):264-301. 3 Sader HS, Flamm RK, Mendes RE, Farrell DJ, Jones RN. Antimicrobial activity of ceftaroline and comparator agents tested against bacterial organisms causing bacteremia in patients with skin and skin structure infections in United States medical centers (2008-2014). Antimicrobial agents and chemotherapy. 2016 Feb 8:AAC-02794. 4 Sader HS, Jones RN, Silva JB, SENTRY Participants Group. Skin and soft tissue infections in Latin American medical centers: four-year assessment of the pathogen frequency and antimicrobial susceptibility patterns. Diagnostic microbiology and infectious disease. 2002 Nov 30;44(3):281-8. 5 Tunbridge AJ, Breuer J, Jeffery KJ. Chickenpox in adults–Clinical management. Journal of Infection. 2008 Aug 31;57(2):95-102.