* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Staphylococcus epi
Mitral insufficiency wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Jatene procedure wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Electrocardiography wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
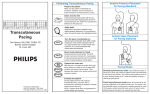
Pacemaker for beginners KITA yosuke Iizuka Hospital Objectives Review basic pacemaker terminology and function Discuss diagnosis and management of pacemaker emergencies Historical Perspective Electrical cardiac pacing for the management of brady-arrhythmias was first described in 1952 Permanent transvenous pacing devices were first introduced in the early 1960’s Pacemaker Components Pulse Generator Electronic Circuitry Lead system Pulse Generator Lithium-iodine cell is the current standard battery Advantages: life – 4 to 10 years Output voltage decreases gradually with time making sudden battery failure unlikely Long Electronic Circuitry Determines the function of the pacemaker itself Utilizes a standard nomenclature for describing pacemakers Pacemaker Nomenclature I II III IV V Chamber Paced Chamber Sensed Response to Sensing Rate Modulation, Programmability Antitachycardia Features A=Atrium A=Atrium T=Triggered P=Simple P=Pacing V=Ventricle V=Ventricle I=Inhibited M=Multiprogrammable S=Shock D=Dual D=Dual D=Dual R=Rate Adaptive D=Dual O=None O=None O=None C=Communicating O=None Lead Systems Endocardial leads which are inserted using a subclavian vein approach Actively fixed to the endocardium using screws or tines Unipolar or bipolar leads Electrocardiogram During Cardiac Pacing Pacemaker has two main functions: Sense intrinsic cardiac electrical activity Electrically stimulate the heart VVI- senses intrinsic cardiac activity in the ventricle and when a preset interval of time with no ventricular activity occurs it depolarizes the right ventricle causing ventricular contraction Pacer spike Electrocardiogram Dual chamber pacer is more complicated because the pacer has the ability to both sense and pace either the atrium or the ventricle Possible to have only atrial, only ventricular or both atrial and ventricular pacing DDD pacer is a common example of this Atrial Spike Ventricular Spike AV Pacing Ventricular Pacing Magnet Placement The EKG technician should perform a 12 lead cardiogram and then a rhythm strip with a magnet over the pacer Often a very poorly understood concept by the non-cardiologist Does not inactivate the pacer as is commonly believed Activate a lead switch present in the pacemaker which converts the pacer to a asynchronous or fixed-rate pacing mode Inhibits the sensing function of a pacemaker Class I Indications For Permanent Pacing Third degree AV block associated with: Symptomatic bradycardia Symptomatic bradycardia secondary to drugs required for dysrhythmia management Asystole > 3 seconds or escape rate < 40 After catheter ablation of the AV node Post-op AV block not expected to resolve Neuromuscular disease with AV block Indications Symptomatic bradycardia from second degree AV block Bifascicular or trifascicular block with intermittent third degree or type II second degree block Sinus node dysfunction with symptomatic bradycardia Recurrent syncope caused by carotid sinus stimulation Indications Post myocardial infarction with any of: Persistent second degree AV block with bilateral bundle branch block or third degree AV block Transient second or third degree AV block and bundle branch block Symptomatic, persistent second or third degree AV block Infections Pacemaker insertion is a surgical procedure: 1% risk for bacteremia 2% risk for wound or pocket infection Usually occur soon after pacer insertion Presence of a foreign body complicates management Infection Cellulitis or pocket infection: Tenderness and redness over the pacemaker itself Avoid performing a needle aspiration – damage the pacer Bacteremia: Staphylococcus aureus and Staphylococcus epi 60-70% of the time Empiric antibiotics should include vancomycin pending culture Infection Consult the pacemaker physician Draw blood cultures Give appropriate antibiotics Frequently the pacer and lead system need to be removed Case 1 67 year old male presents to the emergency room 12 hours after insertion of a pacemaker complaining of left sided chest pain and shortness of breath PR96, RR 33, BP 125/85, Oxygen saturation 88% RA CXR as shown Pneumothorax Occurs during cannulation of the subclavian vien Incidence - ?? Cardiologist dependent Treatment: or small – observation Symptomatic or large – tube thoracostomy Asymptomatic Notify the pacemaker physician Case 2 72 year old male presents to the emergency room after a fall, tripped over a bath mat, no LOC Shortened and rotated left leg Past history – pacemaker, hypertension Nurse does an routine pre-op CXR and EKG Septal Perforation Usually identified at the time of pacer insertion but leads can displace after insertion Can occur with transvenous pacer insertion Keys diagnosis are a RBBB pattern on EKG and a pacer lead displaced to the apex of the heart on CXR Septal Perforation Management: Notify the pacer service Pacer wire has to be removed but not emergently Small VSD which heals spontaneously Conclusions Pacemakers are becoming more common everyday We need to understand basic pacing terminology and modes to treat patients effectively. Most pacer malfunctions are due to failure to sense, failure to capture, over-sensing, or inappropriate rate Standard ACLS protocols apply to all unstable patients with pacemakers.