* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Interactions with Antineoplastic Agents Used in Veterinary Medicine
Survey
Document related concepts
Transcript
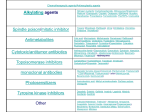
Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 1 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Interactions with Antineoplastic Agents Used in Veterinary Medicine Antineoplastic Agent Interacting Drug Comments Alkylating Agents BCNU (Carmustine) CCNU (Lomustine) Amphotericin B Increases anti-tumor effect resulting from increased cellular uptake1,7,8,9 Cimetidine Potentiates neutropenia and thrombocytopenia1-3,6,8 caused by decreased hepatic degradation7,10 Digoxin Digoxin serum concentrations decreased by agent3,7 Melphalan (intravenous) IV melphalan may reduce threshold for carmustine-induced pulmonary toxicity2 Mitomycin Concurrent use leads to damage of corneal and conjunctival epithelium caused by altered tear film quality2 Phenobarbital Decreases efficacy of agent8 because of increased hepatic clearance7 Phenytoin Phenytoin serum concentrations decreased by agent2,3 Streptozotocin May increase sensitivity of resistant tumor cells to effects of nitrosoureas by inhibiting DNA repair enzyme8 Theophylline Synergistic anti-tumor effects8 Vitamin A Increases anti-tumor effect of agent8 caused by increased cellular uptake7,8 Cimetidine Potentiates myelosuppression6,8 because of decreased hepatic degradation of agent Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 2 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Phenobarbital Streptozotocin Theophylline Chlorambucil Alkylating agents Barbiturates Cyclophosphamide Decreases anti-tumor activity because of increased hepatic metabolism of agent8 May increase sensitivity of resistant tumor cells to effects of nitrosoureas by inhibiting DNA repair enzyme8 Enhances leukopenia and thrombocytopenia and inhibits platelet function11 Concurrent use may potentiate skin rash because of cross-hypersensitivity3 Increased cytotoxicity of chlorambucil caused by increased hepatic enzyme activation7-9 Caffeine Increased cytotoxicity of agent caused by increased metabolic activation9 Epileptogenic drugs Dimethylsulfoxide or sodium thiosulfate Concurrent use may potentiate seizures, tremors3 Decreases chlorambucil efficacy caused by prevention of alkylation8 Prednisone Synergistic9 with lymphoid leukemia2,7 Radiation Allopurinol Radiosensitizer4 Enhances bone marrow suppression2,6- Amitriptyline Concurrent use increases risk of syndrome of inappropriate ADH secretion11 Increased risk of cardiotoxicity2 Anthracyclines 9,11 Anti-tumor vaccines Increase activity of anti-tumor vaccines by selective inhibition of suppressor (CD8+) T-lymphocytes8 Barbiturates Increased toxicity of agent caused by increased rate of conversion to metabolites2,4,7-9 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 3 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Chloramphenicol Decreases efficacy of agent by interfering with metabolism to active form2,3,7 Cimetidine Enhances myelosuppression of agent8 Cisplatin Corticosteroids Synergistic effects7,9 Decreases efficacy of agent initially because of decreased hepatic activation,2,8 then later increases activity of cyclophosphamide as a result of hepatic enzyme induction7,9 Digoxin Cyclophosphamide decreases oral absorption of digoxin1,3,6-8 Diuretics Concurrent use increases risk of syndrome of inappropriate ADH secretion7,11 Doxorubicin Concurrent use increases risk of cardiotoxicity1-3,7 Increased anesthetic mortality in humans7-9 Induces hepatic enzymes and increases agent toxicity,2 but decreases agent efficacy7 May increase insulin requirements in diabetes7 since it may increase or decrease blood glucose11 Enhances myelosuppression and antitumor activity of agent8 Halothane and/or nitrous oxide Imipramine Insulin Interferon Mesna (2-mercaptoethane sulfonate) Decreases risk of hemorrhagic cystitis from cyclophosphamide2,8,10 N-acetylcysteine Inactivates metabolite of agent (acrolein) to decrease hemorrhagic cystitis Decreases efficacy of agent2,7 Phenothiazine Potassium iodide Radiation Induces hepatic enzymes and increases toxicity of agent2 Radiation sensitizer4 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 4 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Succinylcholine Teniposide (VM-26) Concurrent use exaggerates effects of succinylcholine1,3,6,10 caused by cyclophosphamide decreasing pseudocholinesterase2,8,9,11 Increased cyclophosphamide effect9 Thiazide diuretics Concurrent use prolongs leukopenia3,7 Vinblastine Concurrent use increases risk of syndrome of inappropriate ADH secretion7,11 Vincristine Increases toxicity; increases agent effects9; may induce syndrome of inappropriate ADH secretion7,11 Vitamin A Decreases efficacy of agent by interfering with metabolism to active form2,7 Cyclophosphamide increases prothrombin time,3,6 potentiating hematoma formation10 Increases toxicity of DTIC because of synergistic inhibition of xanthine oxidase activity7,8 Warfarin Dacarbazine (DTIC) Ifosfamide Allopurinol Azathioprine/mercaptopurine DTIC enhances toxicity of agent as a result of inhibition of xanthine oxidase activity7 Corynebacterium parvum May prolong half-life of DTIC4 Doxorubicin Interleukin-2 Melphalan Nitrosoureas Phenobarbital Enhances DTIC effects4 Increased DTIC clearance8 Synergistic4 Enhanced DTIC effects4 Increases metabolic activation of DTIC because of hepatic enzyme induction2,7,8 and decreases agent efficacy1 Phenytoin Increases metabolic activation of DTIC because of hepatic enzyme induction2,8 and decreases agent efficacy1 Acetylcysteine Decreases hemorrhagic cystitis risk10 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 5 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Allopurinol Ascorbic acid Mechlorethamine Melphalan Increases myelosuppressive effects of ifosfamide8 Prevents bladder toxicity from agent by keeping drug in reduced state8 Cimetidine Enhances myelosuppressive effects of agent8 Cisplatin Synergistic9; concurrent use can potentiate myelosuppression, nephrotoxicity,8 and encephalopathy of agent2 Cytochrome P-450 inducers Diazepam, barbiturates can increase toxicity because of increased hepatic microsomal enzyme induction2,8 Mesna Binds metabolite of ifosfamide (acrolein) to decrease risk of hemorrhagic cystitis2,8,10 Methylene blue May reverse signs of ifosfamideinduced encephalopathy2 N-acetylcysteine Binds metabolite of ifosfamide (acrolein) to decrease risk of hemorrhagic cystitis2 Cyclophosphamide Sensitizes patients to agent resulting in pruritus, allergic dermatitis2 Pentobarbital Synergistic toxicity caused by concurrent activity at cholinergic site9 BCNU (Carmustine) IV melphalan may reduce threshold for carmustine-induced pulmonary toxicity2 Cimetidine Reduces oral melphalan bioavailability1,2,4,6 Cisplatin Decreased clearance of melphalan caused by cisplatin-induced renal impairment2 Enhances melphalan effects1,8 Corticosteroids Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 6 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Cyclosporine Hematopoietic colonystimulating factors Interferon- Procarbazine Alcohol Antihistamines Barbiturates and microsomal enzyme inducers Increases cytotoxic activity of procarbazine8 and potentiates CNS depression2,4 BCNU (Carmustine) Increased myelosuppression and antitumor effects of agent Digitalis glycosides Indirect-acting adrenergic agents (e.g., tyramine, tyramine-containing foods, sympathomimetics) Combination may decrease digoxin plasma levels1,3,6,8 May potentiate disulfiram (Antabuse) reaction (flushing, headache, nausea, hypotension) in humans1,6,8-11 Enhances risk of hypertensive crisis10 and arrhythmias caused by MAO inhibition from procarbazine causing accumulation of norepinephrine1-3,5,8,9,11 Opiates Enhanced CNS depression1-4,6,8-10 Phenothiazines Increased sedation2,4,9; combination may lead to hypertensive crisis because of procarbazine’s MAO inhibitory effects11 CCNU (Lomustine) Increased myelosuppression and antitumor effects of agent8 Potentiates hyperglycemia and diabetogenic effects1,8 Enhances toxicity of doxorubicin by prolonging half-life2 Synergistic against pancreatic tumors2 Ethanol Streptozocin Increases risk of nephrotoxicity2,6,7 Reduces melphalan-induced neutropenia8 Increased plasma elimination of melphalan with interferon-induced fever2 Disulfiram-like reaction4 Enhanced CNS depression1-4,6,8-10 Corticosteroids Doxorubicin Fluorouracil Niacinamide Nitrosoureas Concomitant administration prevents streptozocin-induced diabetes2 Increased cell sensitivity to nitrosoureas8 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 7 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Anti-tumor Antibiotics Actinomycin D (Dactinomycin, DACT) Nephrotoxins Phenytoin Potentiates renal toxicity2,3 Decreases cytotoxic effects of agent on pancreatic beta cell tumors2,8 Amphotericin B Methotrexate Increases cellular uptake7 and efficacy of actinomycin9 Increased hepatotoxicity when anesthetic administered after agent8 May increase risk of neurotoxicity and decreases efficacy of agent7,9 Decreases efficacy of actinomycin D7,9 Vincristine Decreases efficacy of actinomycin D7,9 Vaccinations Vaccinations with live viruses in patients on actinomycin D can lead to generalized disease from live virus,11 and actinomycin can inhibit efficacy of vaccine8 Actinomycin D produces recall radiation damage when given after ionizing radiation8 Synergistic effects7 possibly caused by increased cellular uptake of agent9 Decreases bleomycin excretion,10 and there is increased risk of cisplatininduced nephrotoxicity7,8; combination can induce hypomagnesemia and pulmonary toxicity2 Anesthetics Fluorouracil Radiation Bleomycin Amphotericin B Cisplatin Digoxin Methotrexate Other anti-neoplastics Oxygen Phenothiazines Phenytoin Bleomycin decreases serum levels of digoxin1,3,7 Bleomycin decreases cellular uptake of MTX and decreases MTX effect9 Pulmonary toxicities may occur at lower doses4 Enhances pulmonary toxicity4,8 Enhance bleomycin toxicity8 Phenytoin serum concentrations decreased by combination chemotherapy3,10 and phenytoin efficacy decreased1 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 8 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Radiation therapy Vinblastine Vincristine Daunorubicin Vitamins (e.g., riboflavin, ascorbic acid) Amphotericin B Synergistic effects,7,9 particularly if given 6–12 hr after bleomycin8 May inactivate bleomycin2 May increase agent cellular efflux8 Anthracyclines Increased risk of cardiotoxicity2 Iron chelators Reduces cardiotoxicity and cytotoxicity of agent8 Decreased methotrexate effect caused by decreased cellular uptake8,9 Agent increases radiation-induced toxicity4 Decreases daunorubicin clearance8 Methotrexate Radiation Verapamil Doxorubicin Enhances bleomycin pulmonary toxicity 8; increases radiation side effects4 Raynaud’s phenomenon in humans2,7 Acetaminophen Actinomycin D Adenosine ADR-529 (Dexrazoxane) Allopurinol Decreases glutathione pool and sensitizes liver to free radical damage4,7 Combination increases risk of acute recall pneumonitis in radiation patients2 Reduces cardiotoxicity of doxorubicin by enhancing coronary blood flow8 Decreases doxorubicin cardiotoxicity; may reduce anti-tumor effectiveness10 and increases myelosuppression Increases anti-tumor effects by inhibition of aglycone formation by xanthine oxidase inhibition8 Amphotericin B Increases cellular uptake of agent7,9 and reduces cell resistance to doxorubicin8 Ascorbate Reduces doxorubicin toxicity by blocking lipid peroxidation8 Increases total plasma clearance of agent2-4,7 caused by microsomal enzyme induction8 Decreases glutathione pool and sensitizes liver to free radical damage4,7 Barbiturates BCNU (Carmustine) Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 9 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Caffeine Blocks agent cytotoxicity8 Calcium-channel blockers Increases risk of cardiotoxicity2 Carnitine Decreases doxorubicin toxicity by enhancing cellular energy8 Decreases clearance of doxorubicin because of blocking doxorubicin breakdown8 Reduces doxorubicin cardiotoxicity8 Cimetidine Co-enzyme Q Daunorubicin Increases cardiotoxicity risk2,8 and risk of cyclophosphamide-induced cystitis2,3,7 Decreases doxorubicin clearance by inhibiting p-glycoprotein efflux pump8; prolongs hematologic toxicity2; seizures2,6 Increases cardiotoxicity risk7 Dexrazoxane Increased risk of myelosuppression2 Digoxin Decreased serum levels of digoxin3,7,10 reduce agent cardiotoxicity because of blocked tissue uptake8 Increases aglycones in cerebrospinal fluid caused by altering the blood–brain barrier8 Cyclophosphamide Cyclosporine Dimethylsulfoxide (IV) Gentamicin Antagonizes bactericidal activity of gentamicin8 Insulin Enhances agent anti-tumor effects by reversed nutritional toxicity8 Interferon-alpha Interleukin-1 Synergistic cytotoxicity8 Reduces agent hematologic toxicity8 Iron chelators Reduces cardiotoxicity and cytotoxicity of agent8 Increases risk of mercaptopurineinduced hepatotoxicity3,7 Reduces cardiotoxicity of agent because of NADPH depletion8 Mercaptopurine Methylene blue Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 10 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Morphine Decreases doxorubicin clearance4 N-acetylcysteine Paclitaxel Reduces cardiotoxicity of agent8 Cremophor EL in paclitaxel decreases biliary excretion of agent4 Reverses multi-drug resistance due to binding p-glycoprotein8 Phenothiazines Phenytoin Decreased serum levels of phenytoin with doxorubicin2 Progesterone Exacerbates doxorubicin-induced neutropenia and thrombocytopenia2 Propranolol Potentiated cardiotoxicity caused by inhibition of co-enzyme Q8 Radiation Doxorubicin increases radiationinduced toxicity4 to the myocardium, mucosa, skin, and liver3 Enhances erythrotoxicity8 Inhibits hepatic metabolism of doxorubicin2 and increases toxicity of agent8 Modulates agent resistance caused by inhibition of p-glycoprotein8 Ranitidine Streptozotocin Tamoxifen Verapamil Vincristine Vitamin E (alpha tocopherol) Vitamin K3 (Menadione) Warfarin Epirubicin Idarubicin Calcium channel blockers Reverses agent resistance, increases doxorubicin exposure,6 enhances lethality of agent8 Seizures with concomitant administration2 Reduces cardiotoxicity8 Reduces cardiotoxicity of agent caused by anti-oxidant effects8 Inhibits anti-tumor effect of agent8 Cimetidine May precipitate congestive heart failure2 Increases epirubicin concentrations2 Microsomal enzyme inducers Increases cytotoxic activity2 Anthracyclines Prior therapy with other anthracyclines increases risk of cardiotoxicity2 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 11 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Mitomycin C Dextran sulfate Teniposide (VM-26) Urokinase Vinblastine Vincristine Enhanced anti-tumor effects8,9 Enhanced cytotoxic effect9 Enhanced anti-tumor effect8,9 Acute pneumonitis3,6,10 Enhanced cytotoxicity of agent9; can potentiate acute bronchospasm in patients with prior exposure to mitomycin3; synergistic8 Mitoxantrone Cytosine arabinoside Doxorubicin Synergistic effects1,4,8; nausea, alopecia, vomiting, stomatitis, mucositis, myelosuppression7 Increased risk of cardiotoxicity2 Radiation Enhanced radiation effects4 ACE inhibitors Adrenergics Severe leukopenia7 Agent inhibits cAMP phosphodiesterase, altering effects of adrenergics8 Agent metabolized to mercaptopurine in alkaline pH4 Prior treatment with alkylators can predispose to cancer induction2 Increases azathioprine toxicity6 by blocking primary pathway for detoxification2,9,11; recommend decreased azathioprine dose to 25%– 33% dose2-4,7,8 Concurrent use may allow decrease in dose of corticosteroids2 Anti-metabolites Azathioprine Alkaline solutions Alkylating agents Allopurinol Corticosteroids Mercaptopurine Muscle relaxants (tubocurarine and Pancuronium) Succinylcholine Warfarin Pre-treatment with mercaptopurine results in paradoxical enhanced antibody response2 Azathioprine reverses neuromuscular blockade of non-depolarizing8 and depolarizing3 muscle relaxants Enhanced neuromuscular blockade8 Agent inhibits hypoprothrombinemic response6 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 12 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Cytosine arabinoside (Cytarabine) Aminoglycosides (gentamicin) BCNU (Carmustine) Cisplatin Cyclophosphamide Digoxin Etoposide Flucytosine GM-CSF Hydroxyurea L-asparaginase Methotrexate Nephrotoxins Fluorouracil Actinomycin D Allopurinol Amphotericin B Cimetidine Cisplatin Hematopoietic growth factors (G-CSF, GM-CSF) Interferon- Leucovorin Methotrexate Decreases efficacy against Klebsiella pneumonia1,2,7 Synergistic4 Synergistic if cytarabine given before cisplatin4 Increased risk of cardiomyopathyinduced death3; synergistic4 Decreased oral absorption of digoxin13,7 Synergistic4 Agent antagonizes anti-infective activity of flucytosine2,7 Enhances toxicity of agent, especially leukemia cells in marrow4,8 Increases agent toxicity4,8 Synergistic7,9 Simultaneous administration enhances therapeutic effect of agent4,7,9; methotrexate uptake is decreased by agent8,9 Increased neurotoxicity of agent10 Decreases efficacy of agent9 and may increase risk of neurotoxicity7 Decreases agent efficacy4,8,10 and reduces toxicity of agent11 Increases efficacy of agent8,9 and increases risk of neurotoxicity7 Increases systemic exposure to agent and increases bioavailability of fluorouracil7,10 Synergistic4; neurotoxicity of agent potentiated7 May reduce myelosuppressive effects of agent4 Enhanced toxicity of agent10 Enhanced toxicity of agent,1,3,4,8,10 particularly GI toxicity2 Enhanced toxicity of agent6,10; synergistic if methotrexate given before agent, antagonistic if given after4,8,9 and incompatible7 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 13 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Metronidazole Enhances toxicity of agent without increasing its efficacy4 Paclitaxel Radiation Antagonistic effects4 Enhanced cell killing with concurrent use4 Antagonizes effects of fluorouracil 8 Tamoxifen Teniposide (VM-26) Thymidine Vincristine Warfarin Gemcitabine Cisplatin Radiation Mercaptopurine Corticosteroids Increases oral bioavailability of agent10; increases myelosuppression,6,9 so need to decrease 6-MP dosage to 25%–33% of dose2-4,7,8,11 Synergistic anti-tumor effects2 Doxorubicin Increased risk of hepatotoxicity7,8 Hepatotoxic drugs Increases risk of hepatic dysfunction and clearance of agent2 Decreases efficacy of agent7-9 Decreases neuromuscular blockade10 Allopurinol Methotrexate Non-depolarizing muscle relaxants (tubocurarine, pancuronium) Thioguanine Trimethoprimsulfamethoxazole Warfarin Methotrexate Synergism9 Synergistic anti-tumor effects4 Increases cytotoxicity7,9 Synergism9; concurrent use may enhance effects of warfarin on prothrombin time6,10 Increased non-hematologic toxicity in patients with concurrent use2 Agent has strong radiosensitization effects4 Allopurinol Mercaptopurine is cross-resistant with thioguanine1 Enhanced bone marrow suppression3,7 Agent can both potentiate and diminish1,6,8,9 anti-coagulant effects of warfarin2 Decreased agent effect when allopurinol given 1 hr prior to agent8 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 14 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Aminoglycosides (oral) May decrease the absorption of oral methotrexate concurrently3 Amphotericin B Increases cellular uptake and cytotoxicity of agent7 May increase clotting times because of agent causing hepatic dysfunction9 Decreases renal excretion of agent11 and increases toxicity10 Decreases cellular uptake of agent7,9 Decreases cellular uptake of agent7,9; enhanced toxicity of methotrexate when cephalothin given 48 hr before agent8 Lowers plasma levels of methotrexate, decreasing its efficacy3 Anticoagulants Aspirin Bleomycin Cephalothin Charcoal Chloramphenicol Displaces from protein binding and increases toxicity2,7,8 Cholestyramine Binds agent in gut and reduces agent concentrations6 Cisplatin Corticosteroids Cyclophosphamide Cyclosporine Cytarabine Daunorubicin Ethanol Etoposide Etretinate Synergistic2; enhanced nephrotoxicity and reduced clearance of cisplatin7,8 Synergistic effects3,8 Decreased cyclophosphamide activation when given 15 hr after agent8 Increases toxicity of agent6 Enhances cytotoxicity4,9 if cytarabine given 1–6 hr after agent; may enhance agent efficacy and toxicity when cytarabine given 48 hr prior to agent7,8 Increases effect of agent9 Can increase methotrexate-induced liver injury6 Decreased cellular efflux of agent when given concurrently8 Increased risk of hepatotoxicity3,6,7 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 15 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Fluorouracil Folic acid preparations (including vitamins) Food Hepatotoxic drugs (retinoids, azathioprine, sulfasalazine) Hydrocortisone sodium succinate Hydroxyurea Enhanced cytotoxicity when fluorouracil given 4–9 hr after agent; decreased cytotoxicity when fluorouracil given 0–24 hr prior to agent7-9 May decrease efficacy of agent2,3,7 Delays absorption of agent if given orally3 Increased risk of hepatotoxicity2 Decreases cellular uptake of agent7,9 and decreases efficacy of agent8 Decreases cellular uptake of agent7,9 Kanamycin Cellular uptake decreased by agent7,9 L-asparaginase Decreased toxicity when asparaginase given 3–24 hr after methotrexate7,8; antagonistic effects9 when asparaginase given before methotrexate4 Leucovorin Decreases methotrexate cytotoxicity3,10 Mercaptopurine Concurrent administration increases mercaptopurine levels and toxicity of mercaptopurine8; mercaptopurine decreases cellular uptake of agent9 Decreased cellular uptake of agent7,9 Methylprednisolone Neomycin Non-steroidal antiinflammatory agents Omeprazole Penicillins Decreased agent effect because of decreased cellular uptake9; decreased oral absorption of agent6 Ketoprofen, naproxen, indomethacin concurrently may be fatal2,3; others— increased hematologic, renal, and gastrointestinal toxicity2,6,7,10 caused by decreased agent elimination2,8 May increase serum levels of agent6 Decreased cellular uptake of agent7,9 and decreased renal secretion of agent, enhancing toxicity2,8 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 16 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Phenylbutazone Displaces agent from protein binding and increases toxicity2,6,7 Phenytoin Decreased serum concentrations of phenytoin3; increased effect and toxicity of agent2,9 when phenytoin given 24 hr prior to agent8 Delays disappearance of agent from serum because of competition for renal tubular secretion,7 thereby increasing agent toxicity3,10,11; increases agent cellular uptake8 Increased risk of nephrotoxicity with combination3,7 Probenecid Procarbazine Pyrimethamine Salicylates (including PeptoBismol) Sulfonamides (including trimethoprimsulfamethoxazole) Increases toxicity of agent2,7 Displaces agent from protein binding and increases agent toxicity2,3,6,7,9; decreases agent renal clearance4,8 Displaces agent from protein binding and increases agent toxicity2,3,6,7,9-11 Sulfonylureas Displaces agent from protein binding and increases agent toxicity2 Teniposide (VM-26) Enhanced cytotoxicity of agent9 caused by decreased cellular efflux of agent8 Displaces agent from protein binding and increases agent toxicity2,7,8 Tetracyclines Theophylline Thiazides Vaccination Vinblastine Methotrexate decreases clearance of theophylline2 Increase bone marrow suppression6 With live viruses, can increase risk of vaccinia infection; live virus vaccination not recommended2,6,11 Increased cellular uptake and agent efficacy9 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 17 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Vincristine Thioguanine Mercaptopurine Nitrosoureas Plant Alkaloids Etoposide (VP-16) Cyclosporine Synergistic anti-neoplastic effects1,2,8; prior treatment with cisplatin may impair elimination of etoposide8 Concurrent administration increases serum cyclosporine and etoposide levels caused by decreased clearance, increasing toxicity2,8 Cytarabine Ifosfamide Additive anti-tumor effects4,8 Decreases renal clearance of agent8 Levamisole Methotrexate Inhibits clearance of agent2 Etoposide decreases cellular efflux of methotrexate8 Verapamil reverses etoposide multidrug resistance and potentiates etoposide-induced DNA strand breaks8 Concurrent use increases prothrombin time1 Increases clearance and reduces paclitaxel toxicity2 Can reverse paclitaxel resistance8 Cisplatin Verapamil Warfarin Paclitaxel Enhanced therapeutic effect8,9 when vincristine given 8–48 hr after agent4; blocked agent cellular efflux or enhanced cellular uptake of agent when vincristine given up to 1 hr prior to agent7,8 Thioguanine is cross-resistant with mercaptopurine1; mercaptopurine sensitizes resistant cells to thioguanine cytotoxicity8 Thioguanine enhances efficacy of nitrosoureas8 Barbiturates Calcium-channel blockers Carboplatin Increased neutropenia when paclitaxel given before carboplatin2 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 18 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Cisplatin Cyclosporine Cyclophosphamide Diazepam Dexamethasone Doxorubicin Epirubicin Etoposide Fluorouracil H2 receptor antagonists Ketoconazole Phenobarbital May be synergistic8; increased neurotoxicity and myelosuppression1,2; increased myelosuppression when paclitaxel given after cisplatin, so recommend giving cisplatin after paclitaxel4; paclitaxel clearance reduced by 30% if cisplatin given prior to paclitaxel8; increased incidence of arthralgia/myalgia in humans2 Inhibits metabolism of paclitaxel; cyclosporine reverses paclitaxel MDR8 Increased myelosuppression when paclitaxel given after cyclophosphamide2,4 Inhibits metabolism of paclitaxel2 Inhibits metabolism of paclitaxel2 Synergistic8; increased levels of doxorubicin and increased cardiac toxicity2; increased mucositis when agent given prior to doxorubicin4 Paclitaxel decreases epirubicin clearance when agent given after epirubicin Inhibits metabolism of paclitaxel2 Decreases efficacy of agent4 May increase metabolism and clearance of agent2,4 Decreased efficacy of agent1; decreased metabolism of agent2 Increased rates of agent clearance and less paclitaxel toxicity2,4 Phenytoin Increased rates of agent clearance and less paclitaxel toxicity2,4 Quinidine Radiation Inhibits metabolism of paclitaxel2 Agent can sensitize cells to radiation4,8 Sedatives (including antihistamines, opioids) Potentiates CNS depression caused by alcohol in paclitaxel formulation2 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 19 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Vinblastine Teniposide Inhibits metabolism of paclitaxel2 Verapamil Inhibits metabolism of paclitaxel2 Vinblastine Vincristine Synergistic simultaneously4 Inhibits metabolism of paclitaxel2 Vinorelbine Increased risk of neuropathy2 Vitamin D Synergistic effects at high ratios of paclitaxel: vitamin D8 Increased risk of ototoxicity2 Combination increases risk of syndrome of inappropriate ADH secretion11 Aminoglycosides Amitriptyline Antifungals (itraconazole, ketoconazole) Bleomycin Cisplatin Cyclophosphamide Diuretics Erythromycin Methotrexate Microsomal enzyme inhibitors Mitomycin C Phenytoin Decreases metabolism of vinblastine, increasing risk of neurotoxicity and ileus2 Synergistic for testicular cancer if vinblastine given before bleomycin CRI8 Increased risk of ototoxicity2 Combination increases risk of syndrome of inappropriate ADH secretion11 Combination increases risk of syndrome of inappropriate ADH secretion11 Increased toxicity vinblastine caused by decreased metabolism of agent2 Cytotoxic effects of methotrexate enhanced by vinblastine1,7,9 caused by increased cellular uptake7,8 and decreased cellular efflux of methotrexate4 May decrease metabolism of vinblastine2 Acute pulmonary reactions (shortness of breath, bronchospasm)1-3,6,7 Reduces phenytoin levels3,8 by 50% in plasma, potentiating seizures1,2,4 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 20 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Vincristine Taxanes (paclitaxel, docetaxel) May decrease cytotoxicity of agent4 Vincristine Combination increases risk of syndrome of inappropriate ADH secretion11 Decreased efficacy of actinomycin D7,9 Increased risk of ototoxicity2 Concurrent use increases risk of syndrome of inappropriate ADH secretion11 Decreases metabolism of vincristine, increasing risk of neurotoxicity and ileus2 Synergistic,9 especially when administered 6–12 hr after agent7,8 Increased intracellular concentration of agent by inhibiting cellular efflux7 Actinomycin D Aminoglycosides Amitriptyline Anti-fungals (itraconazole, ketoconazole) Bleomycin Calcium channel blockers Cisplatin Increased risk of ototoxicity2 Cyclophosphamide Agent enhances cytotoxicity of cyclophosphamide7,9; combination increases risk of syndrome of inappropriate ADH secretion11 Serum levels decreased by agent1,3,7 Digoxin Diuretics Fluorouracil Combination increases risk of syndrome of inappropriate ADH secretion11 Cytotoxicity of fluorouracil enhanced7,9 Glutamic acid May prevent vincristine neurotoxicity8 L-Asparaginase L-Asparaginase Phenytoin Methotrexate Metoclopramide decreases hepatic clearance of vincristine when given before vincristine3; should give vincristine 12–24 hr prior to Lasparaginase7 to minimize toxicity2,4 Reduces phenytoin levels3 by 50% in plasma, potentiating seizures2 Agent enhances cellular uptake of methotrexate4,7-9 May reverse vincristine-induced paralytic ileus8 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 21 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Mitomycin C Acute pulmonary reactions (shortness of breath, bronchospasm)1-3; agent enhances mitomycin cytotoxicity7,9 Neurotoxins Additive neurotoxic effects of both drugs8 May decrease cytotoxicity of agent4 Taxanes (paclitaxel, docetaxel) Verapamil Vinblastine Vinorelbine Aminoglycosides Antifungals (itraconazole, ketoconazole) Cisplatin Impaired metabolism of vinorelbine2 Mitomycin C Acute pulmonary reactions (shortness of breath, bronchospasm)1,2 Increased risk of neurotoxicity2 Aminoglycosides Emetogenics Radiation Thymidine Cisplatin Decreases metabolism of vincristine, increasing risk of neurotoxicity and ileus2 Enhanced neutropenia1; increased risk of ototoxicity2 Cytochrome P450 inhibitors Paclitaxel Platinum Agents Carboplatin May increase efficacy of agent by reversing p-glycoprotein–mediated resistance8 Combination increases risk of syndrome of inappropriate ADH secretion11 Increased risk of ototoxicity2 Aminoglycosides Amphotericin B Anticonvulsants Increased nephrotoxicity and ototoxicity2,3,5,6 Potentiates emetogenic effects of carboplatin2 Increased myelosuppression4 Increases cytotoxicity and efficacy of agent8 Increased nephrotoxicity1,3,5,6,8 and ototoxicity,2,7 especially if aminoglycoside administered concurrently or within 1–2 weeks after cisplatin2 Increased risk of nephrotoxicity2 Plasma concentrations of anticonvulsants decreased1,7 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 22 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Bleomycin Cimetidine Delayed excretion of both drugs,8 increasing toxicity of bleomycin7,10; synergistic effects2 Increased cisplatin toxicity caused by decreased renal clearance of agent8 Combination cephalothingentamicin Cyclophosphamide Cytarabine Diazoxide Doxorubicin Emetogenics Increases risk of cisplatin-induced nephrotoxicity7,9 Synergistic7,9 Increased ototoxicity10 Increased nephrotoxicity6 Synergistic2 Potentiates emetogenic effect of agent3 Etoposide Synergistic8; renal clearance of etoposide impaired by agent2 Synergistic2,7 Increased risk of ototoxicity2 Fluorouracil Furosemide Ifosfamide Increased toxicity of ifosfamide with concurrent use8 and synergistic9 Interferon- Loop diuretics (ethacrynic acid, furosemide) Mesna Synergistic7 Increased risk of ototoxicity3,6,7 Methotrexate Synergistic2; enhanced nephrotoxicity and reduced clearance of cisplatin7,8 Phenytoin Reduced plasma levels of phenytoin2,3,6 Radiation Tamoxifen Thiosulfates (sodium thiosulfate) Vinca alkaloids Increased cytotoxicity4 Synergistic anti-tumor effect8 Direct inactivation of cisplatin and decreased efficacy5,8 and decreased toxicity of agent4; IV injection of sodium thiosulfate reduces nephrotoxicity of intraperitoneal cisplatin10 Synergistic2 Antimetabolites Synergistic4 Inactivates cisplatin and decreases antitumor activity of agent8 Miscellaneous Hydroxyurea Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 23 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Antiviral nucleosides Cytarabine Fluorouracil Methotrexate Radiation L-Asparaginase Cyclophosphamide Cytarabine Mercaptopurine Methotrexate Prednisone Vincristine Mitotane (o,pDDD) Anticoagulants Barbiturates Enhanced antiviral effects4 Agent increases metabolism of cytarabine to its active form, thereby increasing its efficacy8 Decreased metabolism of fluorouracil leading to increased neurotoxicity8 Decreased cellular uptake of methotrexate leading to decreased efficacy9 Enhanced cytotoxicity of radiation4 Agent interferes with cyclophosphamide activation because of effects on hepatic function2,7 Synergistic7-9 Increased hepatotoxicity of mercaptopurine2,7 Increased hepatotoxicity of methotrexate2; asparaginase may diminish methotrexate anti-tumor effects3,9 when administered concurrently or prior to methotrexate10; if enzyme administered 9–10 days prior to or shortly after methotrexate, antitumor effects of methotrexate are enhanced8,9 and GI/hematologic toxicities of methotrexate decreased4,7 Hyperglycemia2,7 caused by enzyme inhibition of insulin synthesis8; administration of agent concurrently or immediately prior to prednisone increases toxicity,3 particularly hepatotoxicity2 Agent interferes with metabolism of vincristine2; cumulative neuropathy and disturbance of erythropoiesis2; administration of enzyme after vincristine may decrease potential for toxicity3,7,8 Mitotane increases hepatic metabolism of anticoagulants and increases anticoagulant dose requirements2 Mitotane increases hepatic metabolism of barbiturates1,7,8 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 24 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) CNS depressants Corticosteroids Enhanced CNS depression2,7 Mitotane increases hepatic metabolism of corticosteroids1,3,7,8 Cyclophosphamide Mitotane increases hepatic metabolism8 Phenytoin Cholestyramine Mitotane increases hepatic metabolism of phenytoin1,8 Spironolactone blocks action of mitotane2,6,7,10 Mitotane inhibits warfarin action6; can increase warfarin metabolism1,3,8 Concurrent use decreases antihypertensive effect of ACE inhibitor as a result of piroxicam inhibition of prostaglandin synthesis2 May increase risk of GI perforation or GI bleeding2; piroxicam may displace anticoagulants from protein in blood, thereby increasing risk of bleeding; combination increases anticoagulant effects6 Concurrent use decreases piroxicam plasma levels2 Enhances piroxicam elimination6 Corticosteroids Increased risk of GI ulceration2 Diuretics Piroxicam reduces natriuretic effects of furosemide and thiazide diuretics; combination may decrease nephrotoxicity2 Piroxicam decreases renal clearance of methotrexate, increasing toxicity of methotrexate2,6 Piroxicam may displace salicylates from protein in blood, thereby increasing toxicity of salicylates2 Spironolactone Warfarin Piroxicam Angiotensin-converting enzyme (ACE) inhibitors Anticoagulants Aspirin Methotrexate Salicylates Sulfonylureas Piroxicam may displace sulfonylurea from protein in blood, thereby increasing toxicity of sulfonylureas2 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 25 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Prednisone Amphotericin B Anticoagulants Increased risk of hypokalemia2 Concurrent use may enhance or diminish anticoagulant effects2 Aspirin Prednisone decreases salicylate serum concentrations; discontinuing prednisone with concurrent high-dosage aspirin therapy can predispose to aspirin toxicity6; aspirin decreases prednisone excretion rates8 Barbiturates may reduce serum concentrations of prednisone2,6 Barbiturates Chlorambucil Cholestyramine Synergistic9 with lymphoid leukemia2,7 Cholestyramine may reduce serum concentrations of prednisone6 Cyclosporine Cyclosporine decreases plasma clearance of prednisone because of cyclosporine inhibition of hepatic microsomal enzymes2; may increase plasma concentrations of both drugs, resulting in seizures6 Increased risk of hypokalemia2 Diuretics (thiazides, furosemide) Estrogens Microsomal enzyme inducers Estrogens may potentiate effects of steroids2 Prednisone increases blood glucose concentrations, thereby increasing insulin dosage requirements6 Prednisone reduces concentrations of isoniazide2,6 Ketoconazole increases prednisone concentrations, enhancing suppression of cortisol secretion6 Enhances metabolism of prednisone2 Microsomal enzyme inhibitors Decreases metabolism of prednisone2 Mitotane Mitotane inhibits peripheral metabolism of corticosteroids8 Increased risk of GI ulceration2,6 Insulin Isoniazid (INH) Ketoconazole Non-steroidal antiinflammatories Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 26 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Vaccines Prednisone inhibits antibody response and potentiates infection with live virus; concurrent use can aggravate neurologic reactions to some vaccines2 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 27 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Physical Incompatibilities of Antineoplastics Agent Alkylating Agents BCNU (Carmustine) Cyclophosphamide Dacarbazine (DTIC) Drug Incompatibilities Allopurinol sodium12 Sodium bicarbonate solutions2,8,12 Gas evolves immediately Decomposition of drug with sodium bicarbonate or solutions with pH >6.02 Dextrose 5% in water2,12 PVC containers2,12 Inactivates agent2 Inactivates agent; recommend glass containers2 Amphotericin B cholesteryl sulfate complex12 Benzyl alcohol7,11 Increased turbidity immediately Allopurinol sodium12 Cefepime HCl12 Small particles within 1 hr Cloudy solution immediately Dextrose 5% in water12 Some degradation of drug with increased contact Drug precipitates at 25 mg/ml dacarbazine and 100 U/ml heparin; no precipitation at lower DTIC concentrations12 Heparin1,3,12 Hydrocortisone sodium succinate1,2,5,7,8,11 Lidocaine1 Light1,5 Piperacillin sodiumtazobactam sodium12 Ifosfamide Mechlorethamine Comments Decomposition of drug in contact with benzyl alcohol; avoid in vitro contact Physically incompatible2; avoid in vitro combination; immediate pink precipitate5 Physically incompatible 50% deactivation when left in room light >4 hr Drug precipitates Cefepime HCl12 Methotrexate sodium12 Acidic solutions2,8 Alkaline or neutral solutions2,3,12 Precipitates in <1 hr Precipitates in 4 hr Immediate decomposition of agent2 Agent is highly unstable in these solutions2; avoid with sodium thiosulfate or sodium bicarbonate solutions Allopurinol sodium12 Immediate precipitation Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 28 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Melphalan Procarbazine Streptozocin Cefepime HCl12 Dextrose 5% in water12 Immediate precipitation Degradation of agent Methohexital sodium9,12 Sodium chloride 0.9%12 Amphotericin B12 Physically incompatible Degradation of agent within several hours Precipitation in sodium chloride solution Chlorpromazine HCl12 Dextrose 5% in water12 Precipitation in <1 hr Degradation of agent within <2 hr Ringer’s injection, lactated12 Sodium chloride 0.9%12 Aqueous solution5 Degradation within hours Light5 Allopurinol sodium12 Aztreonam12 Cefepime HCl12 Piperacillin sodiumtazobactam sodium12 Degradation within <1 hr Degradation of agent to toxic compounds5 Inactivation Haze within 1 hr Color change within 1 hr Haze immediately and color change Particle formation within 1 hr Anti-tumor Antibiotics Actinomycin D (Dactinomycin, DACT) Bleomycin Diluents with preservatives5,8,12 Filgrastin12 Filters1,8,11,12 Precipitation Amino acids7 Aminophylline7,8,12 Ascorbic acid2,5,7-9,12 Carbenicillin8 Cefazolin8,12 Cephalothin7,8 Copper (or other ionic solutions)7,8,11 Physically incompatible 50% loss of activity in 1 week12 Loss of all activity over 1 week12 Physically incompatible 43% loss of activity in 1 week12 Physically incompatible Bleomycin chelates with divalent and trivalent anions; do not mix Dexamethasone7 Dextrose 5% in water2,12 Diazepam7,8,12 Droperidol7 Furosemide7 Hydrocortisone sodium succinate7,8,12 Physically incompatible Inactivation of agent Physically incompatible Physically incompatible Physically incompatible Loss of activity in 1 week12 Immediate precipitation Do not use filters, which remove drug from solution, particularly cellulose8,11,12 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 29 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Daunorubicin Doxorubicin Hydrogen peroxide5,9 Methotrexate7,8,12 Mitomycin C7,8,12 Nafcillin8,12 Penicillin7,8,12 Riboflavin2,7 Sulfhydryl-group containing compounds5,7,9 Terbutaline7,8,12 Aluminum12 Allopurinol12 Aztreonam12 Cefepime HCl12 Dexamethasone sodium phosphate2,5,8,9,12 Fludarabine phosphate12 Heparin1,2,4,5,8,9,11,12 Solutions with pH >8.02 Piperacillin sodiumtazobactam sodium12 Physically incompatible Loss of activity in 1 week12 Loss of activity in 1 week12 Loss of activity in 1 week12 Loss of activity in 1 week12 Physically incompatible Physically incompatible Aluminum11,12 Aluminum hubs may inactivate drug Allopurinol12 Aminophylline1,5,7-9,12 Precipitate Decomposition of agent, solution darkening12 Precipitate formation Precipitate formation Precipitate formation Inactivation of doxorubicin and ondansetron Physically incompatible Precipitate formation Amphotericin B12 Cefepime HCl12 Cephalothin5,7-9 Combination ondansetron and dacarbazine Cyclosporine1 Dexamethasone sodium phosphate1,5,7-9 Diazepam1,5,7,9,12 Fluorouracil2,5,7-9,12 Furosemide1,7,8,12 Ganciclovir sodium12 Heparin1,2,4,5,7-9,11,12 Hydrocortisone sodium phosphate9 Hydrocortisone sodium succinate5,7,9 Loss of activity in 1 week12 Results in color change Color change Haze immediately Haze immediately Gross precipitate Haze formation Precipitate Color change Turbidity immediately Immediate precipitate Color change Precipitate formation Color change Precipitate formation Precipitate formation Precipitate formation Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 30 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Doxorubicin (liposome encapsulated; Doxil) Epirubicin Idarubicin Piperacillin sodiumtazobactam sodium12 Propofol12 Streptozocin1 TPN (212-215)12 Vinblastine12 Precipitate formation Amphotericin B12 Buprenorphine HCl12 Cefoperazone sodium12 Ceftazidime12 Docetaxel12 Filters12 Precipitate within 4 hr Loss of turbidity Loss of turbidity Loss of turbidity Loss of turbidity Removes liposome; do not use filters Hydroxyzine HCl12 Mannitol12 Meperidine HCl12 Metoclopramide12 Mitoxantrone HCl12 Morphine sulfate12 Paclitaxel12 Piperacillin sodiumtazobactam sodium12 Promethazine HCl12 Sodium bicarbonate12 Alkaline solutions Combination ifosfamide and mesna12 Fluorouracil12 Acyclovir8,12 Alkaline solutions1,3 Allopurinol sodium12 Ampicillin8,12 Cefazolin8,12 Cefepime12 Ceftazidime8,12 Cilastin8 Clindamycin8,12 Precipitate in 4 hr Loss of turbidity Increase in turbidity Increase in turbidity Loss of turbidity Loss of turbidity Loss of turbidity Loss of turbidity 8,12 Dexamethasone Etoposide8,12 Furosemide8,12 Gentamicin8,12 Heparin1,2,3,8,12 Emulsion breaks Physically incompatible Physically incompatible Suspected to be incompatible Increase in turbidity Loss of turbidity Hydrolyzes agent Loss of 50% epirubicin by 7 days Precipitate within hours Precipitate within 12 min Precipitation Precipitate within 1 hr Immediate precipitate Precipitate within 1 hr Precipitate within 4 hr Haze forms within 1 hr Haze formation Immediate precipitate Immediate gas formation Immediate precipitate Immediate color change Immediate precipitate Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 31 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Mitomycin C Mitoxantrone Hydrocortisone sodium succinate8,12 Imipenim8 Lorazepam8,12 Meperidine8,12 Methotrexate8,12 Mezlocillin8 Piperacillin sodiumtazobactam sodium12 Sodium bicarbonate8,12 Teniposide (VM-26)12 Vancomycin8,12 Vincristine8,12 Acidic solutions12 Alkaline solutions12 Aztreonam12 Bleomycin sulfate12 Cefepime HCl Dextrose solutions12 Immediate precipitate Etoposide (VM-16)12 Filgrastim12 Gemcitabine12 Piperacillin sodiumtazobactam sodium12 Sagramostim12 Sodium chloride 0.9%12 Color change within 1hr Color change within 1 hr Color change within 1 hr Color change within 4 hr Vinorelbine12 Amphotericin B cholesteryl sulfate complex12 Aztreonam12 Cefepime HCl12 Doxorubicin HCl liposome injection12 Fluorouracil7 Heparin2,3,7,8 Color change in 1 hr Gross precipitate forms Immediate color change Immediate color change Immediate color change Immediate color change Immediate precipitate Immediate precipitate Immediate precipitate Immediate color change Immediate color change Immediate color change Decomposition Decomposition Color change within 4 hr Loss of activity in 1 week Color change within 1 hr Incompatible at some concentrations Precipitate in 30 min At 50 mg/L mitomycin, incompatible; however, not at other concentrations Heavy precipitate in 1 hr Haze immediately Loss of turbidity Precipitate formation Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 32 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Antimetabolites Azathioprine Cytosine arabinoside (Cytarabine) Hydrocortisone sodium phosphate12 100–200 g hydrocortisone with 50–200 mg mitoxantrone in D5W in PVC; this did not occur with same concentrations in glass container Paclitaxel12 Piperacillin sodiumtazobactam sodium12 Propofol12 TPN (212–215)12 Decreased natural haze of paclitaxel Haze immediately Particles form immediately Loss of natural turbidity Alkaline pH solutions8,11,12 Azathioprine is metabolized to mercaptopurine at alkaline pH Cysteine (or other sulfhydryl-containing compounds)12 Allopurinol sodium12 Amphotericin B cholesteryl sulfate complex12 Alkaline solutions12 Hydrolysis to mercaptopurine occurs in presence of cysteine Benzyl alcohol2 Bacteriostatic water containing benzyl alcohol should not be used for reconstitution Carbenicillin8 Cephalothin7 Fluorouracil5,7,9,11,12 Ganciclovir sodium12 Gentamicin sulfate7,8,12 Heparin7,8,12 Hydrocortisone sodium succinate7,12 Insulin, regular7,8,12 Methotrexate7,9,11 Methylprednisolone sodium succinate7,12 Particles within 4 hr Gross precipitate Increased rate of decomposition Change in spectrophotometry of cytarabine5,9,12 Turbidity within 30 min Physically incompatible, but compatible for 24 hr at 80 mg/L gentamicin and 300 mg/L cytarabine Haze formation Physically incompatible Fine precipitate formation Change in spectrophotometry of methotrexate9 At 250 mg/L MPSS and 360 mg/L cytarabine12 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 33 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Fluorouracil Nafcillin sodium8,12 Oxacillin sodium12 Heavy precipitate pH outside stability range for oxacillin Penicillin sodium7,12 TPN (#212–215)12 Amino acids7,8,11 Amphotericin B cholesteryl sulfate complex12 Carboplatin12 Cisplatin12 Cytarabine5,7,9,12 pH outside stability range for penicillin Loss of natural turbidity Dextrose solutions7 10% loss of fluorouracil in 7 hr at room temperature Precipitate Color change Immediate precipitation Precipitate within hrs Loss of fentanyl Particles in 1 hr Diazepam5,7,8,9,11,12 Doxorubicin5,8,9,11,12 Droperidol7,12 Epirubicin HCl12 Fentanyl citrate12 Filgrastim12 Insulin7,8,11 Leucovorin calcium12 Gemcitabine Methotrexate5,7,8,9,11 Metoclopramide12 Morphine sulfate12 Multivitamins7,8,11 Ondansetron12 Penicillin7,8,11 Tetracycline7,8,11 TPN (#212–215)12 Vinorelbine tartrate12 Acyclovir sodium12 Amphotericin B12 Cefoperazone sodium12 Cefotaxime sodium12 Furosemide12 Ganciclovir sodium12 Imipenem-cilastatin sodium12 Methotrexate12 Microprecipitate immediately >20% carboplatin loss in 24 hr Loss of cisplatin within 4 hr Change in spectrophotometry of cytarabine Particulate formation Change in spectrophotometry of both Loss of both drugs Precipitate Immediate precipitation Turbidity formation Precipitate immediately Precipitate immediately Precipitate immediately Precipitate immediately Haze formation Precipitate immediately Precipitate immediately Color change within 1 hr Precipitate immediately Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 34 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Mercaptopurine Methotrexate Methylprednisolone sodium succinate12 Mitomycin12 Piperacillin sodium12 Piperacillin sodiumtazobactam sodium12 Prochlorperazine edixylate12 Allopurinol sodium8,9 Allopurinol sodium in D5W5,7,9 Prednisolone sodium succinate8,9 Prednisolone sodium succinate and D5W5,7 Aluminum12 Bleomycin sulfate12 Chlorpromazine12 Cytarabine5,8,9,11 Dexamethasone sodium phosphate12 Droperidol7,12 Fluorouracil5,7,8,9,11 Gemcitabine12 Idarubicin12 Ifosfamide12 Metoclopramide7,12 Plant Alkaloids Etoposide (VP-16) Precipitate immediately Color change Cloudiness immediately Cloudiness immediately Haze immediately Physical incompatibility Physical incompatibility Orange crystal formation with aluminum needles 60% loss of bleomycin activity in 1 week Turbidity and precipitate immediately Change in spectrophotometry of methotrexate8,9 Dark precipitate in 4 hr Immediate precipitate Change in spectrophotometry of both8,9 Precipitate immediately Color change immediately Yellow precipitate in 4 hr Incompatible; if mixed, use immediately Midazolam12 Nalbuphine HCl12 Prednisolone sodium phosphate7,8,9,11 Promethazine HCl12 Propofol12 Ranitidine HCl7 TPN (#212–215)12 Vancomycin12 Yellow precipitate immediately Yellow precipitate immediately Change in spectrophotometry of both8,9 Alkaline solutions8,12 Amphotericin B12 Cefepime HCl12 Inactivates drug (hydrolysis) Precipitate with etoposide phosphate Haze formation Turbidity in 30 min Precipitate in 1 hr Loss of natural turbidity Precipitate within 4 hr Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 35 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Chlorpromazine12 Dextrose solutions7,9 Filgrastim12 Idarubicin12 Imipenem-cilastatin sodium12 Methylprednisolone sodium succinate12 Mitomycin12 Prochlorperazine edisylate12 PVC containers12 Paclitaxel Vinblastine Vincristine Precipitate with etoposide phosphate Precipitate formation9 Particles immediately Gas forms immediately Discoloration with etoposide phosphate Haze formation with etoposide phosphate Sodium chloride 0.9%7,12 Color change with etoposide phosphate Precipitate immediately with etoposide phosphate Leaches diethylhexyl phthalate (DEHP) plasticizer Precipitate Amphotericin B2,12 Aqueous solutions12 Decreased natural turbidity Unpredictable precipitate formation Chlorpromazine HCl2,12 Cisplatin12 Dextrose 5% in water12 Doxorubicin liposome injection12 Hydroxyzine HCl2,12 Methylprednisolone sodium succinate2,12 Mitoxantrone HCl2,12 PVC containers1,2,8,12 Normal paclitaxel haze decreases Subvisual particulates after 3–5 days At some concentrations Loss of natural turbidity Cefepime12 Doxorubicin12 Furosemide7,12 Heparin sodium7,12 Solutions with pH <3.5, >5.53 Alkaline solutions12 Cefepime12 Furosemide7,12 Light2,12 Idarubicin12 Sodium bicarbonate12 Normal paclitaxel haze decreases Normal paclitaxel haze decreases Normal paclitaxel haze decreases PVC can leach out plasticizer DHEP when exposed to Cremophor-containing solutions Haze immediately Questionable compatibility; assays erratic Immediate precipitation Turbidity within minutes Inactivate drug Precipitation Immediate precipitate Immediate precipitate Inactivated in light Color change immediately White precipitate Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 36 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Vinorelbine Solutions with pH <3.5, >5.53 Acyclovir sodium12 Allopurinol sodium12 Aminophylline12 Amphotericin B12 Amphotericin B cholesteryl complex12 Ampicillin sodium12 Cefazolin sodium12 Cefotetan disodium12 Ceftriaxone sodium12 Cefuroxime sodium12 Fluorouracil12 Furosemide12 Incompatible Ganciclovir sodium12 Precipitates immediately Methylprednisolone sodium succinate12 Mitomycin12 Piperacillin sodium12 Sodium bicarbonate12 Thiotepa12 Precipitates immediately Trimethoprimsulfamethoxazole12 Precipitates immediately Alkaline solutions (pH >6)12 Aluminum1,2,3,8,12 Increased degradation Precipitates immediately Precipitates immediately Light haze immediately Immediate yellow precipitate Gross precipitate Precipitates immediately Turbidity increases Precipitates immediately Precipitates immediately Turbidity increases Precipitates immediately Precipitates immediately Color change within 1 hr Increased turbidity Precipitates immediately Precipitates immediately Platinum Agents Carboplatin Amphotericin B cholesteryl sulfate complex12 Fluorouracil12 Mesna12 Sodium bicarbonate12 Sodium chloride2,5,12 Cisplatin Alkaline solutions12 Do not use aluminum needles; displaces platinum from agent2 Turbidity increases >20% carboplatin loss in 24 hr >10% carboplatin loss in 24 hrs 200-nM solution has 13% loss in 24 hr Controversial; converts carboplatin to cisplatin at rate of <10% per day12 Increased hydrolysis12 Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 37 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Aluminum1,2,12 Do not use aluminum needles; displaces platinum from agent2 Amifostine12 Amphotericin B cholesteryl sulfate complex12 Cefepime HCl12 Dextrose 5% in water5,7,8,12 Fluorouracil12 Subvisual haze in 4 hr Gross precipitate formation Light2,12 Mannitol2,5,7,8,9 Degradation of drug Time-dependent degradation of cisplatin9; can store together for less than 2–3 days8 Cisplatin not detectable after 1 hr Mesna8,12 Metoclopramide Paclitaxel12 Piperacillin sodiumtazobactam sodium12 Refrigeration12 Haze formation in 1 hr Breakdown after 2 hr in solution7 Cisplatin loss within several hours Particulate formation after 3–5 days Haze and particles in 1 hr Particle formation Sodium bicarbonate 5%2,4,5,7 Sodium bisulfite2,7,11 Sodium chloride <0.2%2 Sodium thiosulfite2,8 Thiotepa12 TPN (#212–215)12 Enhanced decomposition of agent; gold precipitate Cisplatin inactivated Decomposition of agent Inactivates agent White cloudiness in 4 hr Discoloration in 1-4 hr Filters <0.2 m12 Filters 5 m are fine12; filters bind asparaginase8 Miscellaneous L-Asparaginase Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 38 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) REFERENCES 1. Baquiran DC and Gallagher J: Lippincott’s Cancer Chemotherapy Handbook, Philadelphia, 1998, Lippincott-Raven. A handbook on general management of chemotherapy reactions in human patients, drug administration, and individual drug information including drug interactions. 2. Dorr RT and Fritz WL: Drug Interactions. In Cancer Chemotherapy Handbook. New York, 1980, Elsevier. A textbook on general chemotherapy principles in human medicine, individual chemotherapy information and drug interactions. 3. Dorr RT and Von Hoff DD: Cancer Chemotherapy Handbook, ed 2, Norwalk, 1994, Appleton & Lange. A textbook on administration of chemotherapy in human patients and individual drug information including drug interactions for each drug. 4. Henry CJ and Brewer WJ: Drug Interactions with Antineoplastic Agents. In Current Veterinary Therapy XII, Philadelphia, 1995, WB. Saunders. This chapter lists chemotherapy agents and drugs with which they interact in vivo as well as in vitro incompatibilities focusing on drugs more commonly used in veterinary medicine. 5. Hansten PD and Horn JR: Hansten and Horn’s Managing Clinically Important Drug Interactions, Vancouver, 1998, Applied Therapeutics, Inc. A manual of specific drug interactions listed by individual drug, and how to manage the toxicities and interactions, not limited to chemotherapy agents. 6. McEvoy GK(editor): Antineoplastic Agents. In American Hospital Formulary Services (AHFS) Drug Information, Bethesda, 2005, American Society of Health-System Pharmacists, Henry, 1/e, ISBN 978-1-4160-3183-3 Chapter 012 (edited file)—“Tables 12B-1 and 12B-2” 6/30/2017, Page 39 of 39, 0 Figure(s), 2 Table(s), 0 Box(es) Inc. A pharmaceutical manual providing details of individual drug information including pharmacology, use, toxicities, drug interactions, incompatibilities, stability, and chemistry of agents. 7. Olin BR (ed): Drug Interactions. In Drug Facts and Comparisons, St. Louis, 1992, Wolters Kluwer Company. A manual of pharmacologic information on drugs. 8. Fisher DS, Knobf M Tish and Durivage HJ: Drug Interactions with Antineoplastic Agents. In The Cancer Chemotherapy Handbook, ed 4, St. Louis, 1993, Mosby. A manual on chemotherapy principles, administration, and drug interactions. 9. Griffin JP and D’arcy PF: Antineoplastic Agents. A Manual of Adverse Drug Interactions, ed 3, Bristol, 1984, Wright. A textbook on drug interactions not limited to chemotherapy. 10. Chabner BA and Longo DL: Cancer Chemotherapy and Biotherapy: Principles and Practice, ed 3. Philadelphia, 2001, Lippincott Williams & Wilkins. A textbook on principles of chemotherapy and chemotherapy drug information. 11. Dorr RT: Incompatibilities with Parenteral Anticancer Drugs. In the American Journal of Intravenous Therapy. 6(2):44, 1979. A review of in vitro chemotherapy drug interactions. 12. Trissel LA: Handbook on Injectable Drugs, ed 11, Bethesda, 2001, American Society of Health-System Pharmacists, Inc. A textbook providing detailed information regarding in vitro drug interactions, stability, and pharmacology of individual drugs based on in vitro studies.