* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download outline25084
Urinary tract infection wikipedia , lookup
Immunosuppressive drug wikipedia , lookup
Common cold wikipedia , lookup
Gastroenteritis wikipedia , lookup
Infection control wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Neonatal infection wikipedia , lookup
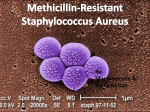
Multiple sclerosis research wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Management of multiple sclerosis wikipedia , lookup
Methicillin-resistant Staphylococcus aureus wikipedia , lookup
I. Alert on Topiramate (Topamax) A. Approved 12-96 for seizure disorders B. Unapproved: Migraine HA, weight loss, depression, bipolar disorder C. Mechanism of action is unknown D. At least 115 reported cases of acute, bilateral, secondary angle-closure glaucoma E. Onset usually within first 2 weeks of therapy F. Most common presenting symptom: blurred vision G. Exact mechanism of increased IOP is unknown H. Treatment: Stat consult with prescribing physician to begin to reduce topiramate dosage; then aqueous suppressants, oral CAI, cycloplegia (retracts ciliary body) - no miotics I. II. IOP normalizes in 1-4 days, no laser treatment indicated Orbital Pseudotumor A. Usually acute onset, unilateral, red eye B. Chemosis, lid edema and erythema C. Proptosis, EOM dysfunction - diplopia + D. Systemic association rare if unilateral III. E. VA, exophthalmometry, IOP, CT or MRI F. Treatment is oral prednisone, high dose (1mg/kg/d initially) with taper Giant Fornix Syndrome A. Hyperacute staphylococcal aureus infection without lymphadenopathy B. Disease of the AGED! C. Patients tend to have large recesses in their superior cul-de-sac D. Usually unilateral, but can be bilateral E. Treatment 1. Sweep superior fornix to remove as much coagulum as possible 2. Oral antibiotic (Augmentin, Levaquin, etc) 3. Topical antibiotic q 1-2 hrs 4. Topical steroid q 2-4 hrs 5. Nocturnal ointment hs 6. IV. Meticulous eyelid hygiene Rapid Pathogen Screening via the RPS Adeno Detector A. Convenient in-office, 10 minute immunoassay B. Designed exclusively for adenoviral pathogens C. Clinical Laboratory Improvement Amendment (CLIA) waived D. Has sensitivity and specificity around 91-92% E. Adenoviral infection is most always a clinical diagnosis F. Could be helpful for unusual cases, and for primary care physicians G. Cost: Approximately $13.50/test H. CPT-4 for 2008: 87809 QW (Medicare reimbursement $16.76) V. Mini-Tip Culturette A. Culture device for ocular infections/corneal ulcers B. High yield (sensitivity 83.3% and specificity 100%) and cost-effective C. Rayon-tipped swab with one ampule of 0.5ml of modified Stuart’s bacterial transport medium D. Avoid contamination by touching patient’s lids or lashes VI. E. Culture results identify the underlying etiology in event healing does not occur as predicted or if condition worsens. F. Becton-Dickinson Microbiology Systems or Remel, Inc. (CalgiSwab Type 1) Povidone - Iodine 5% ophthalmic solution A. Broad spectrum microbicide B. Indicated for “irrigation of the ocular surface” C. “Off label” use: Treat adenoviral keratoconjunctivitis 1. Anesthetize with proparacaine 2. Instill 1 or 2 drops of NSAID 3. Instill several drops Betadine 5% in eye(s), close eye(s) 4. Swab or rub excess over eyelid margin 5. After 1 minute, irrigate with sterile saline 6. Instill 1 or 2 drops of NSAID 7. Rx Lotemax qid x 4 days D. No reports in clinical trials of adverse reactions. E. Avoid use if patient is allergic to iodine F. Marketed as Betadine 5% ophthalmic prep solution (30 ml opaque bottle) by Alcon surgical G. CPT 99070 supply code VII. Bacterial Conjunctivitis A. Unilateral or bilateral red eye(s) with purulent or mucopurulent discharge of varying degree B. In subtle cases, carefully examine the lacrimal lake under high magnification and look for microparticulate debris which can be evidence of bacterial infection. C. Preauricular lymphadenopathy is uncommon, but can be present in hyperacute cases D. There can be some chemosis, depending upon the severity of the infection E. SPK can be present, especially if staphylococcal etiology. This is usually the result of staph exotoxin chemotoxicity, and tends to be seen mostly inferonasally because of tear film dynamics F. Concomitant staph blepharitis can be causative and, if not adequate treated, can lead to recurrences G. Common etiology: 1. Adults: Staph aureus, Staph epidermidis, Strep pneumoniae 2. Children: Streptococcus pneumoniae H. Therapy I. VIII. 1. Adults: Tobramycin, Polytrim, or Fluoroquinolone 2. Children: Polytrim or Azasite solution or Polysporin ointment Treat for five to seven days as a rule Adenoviral Infections A. Common cause of “red eyes” B. Assume adenovirus until proven otherwise C. Often have pre-auricular node D. Non-purulent watery discharge E. Usually starts in one eye and spreads to fellow eye in a few days F. Always evert lids to survey tarsal conjunctiva G. With EKC, spotty sub-epithelial infiltration in 50 to 75% IX. Methicillin Resistant Staphylococcus Aureus (MRSA) A. Infection caused by Staphylococcus aureus (“Staph”) B. Staph commonly carried on skin or in nose C. Skin infections (abscesses, boils) most common (25-30% colonized) D. MRSA is almost always spread by direct physical contact E. MRSA common in hospitals and healthcare facilities F. To prevent MRSA: G. Keep infections clean and dry H. Frequent hand washing I. X. Avoid sharing personal items MRSA Update A. 94,360 serious MRSA (invasive) in 2005 B. 85% of invasive MRSA associated with healthcare C. Incidence highest in older persons (>65), blacks, and males D. www.cdc.gov/ncidod/dhqp/ar_mrsa_prevention.html XI. E. http://www.cdc.gov/ncidod/dhqp/ar_mrsa_ca_prevention.html F. In 1974, MRSA 2% of total staph infections; in 1995, MRSA 22%; in 2004 was 63% Soothe XP (emollient lubricant) A. Meta-stable emulsion (shake before using) B. Restoryl rapidly provides a protective lipid barrier C. Reduces harmful evaporation to prevent tear loss D. Replenishes the complete tear film E. Relieves discomfort of dry eye for up to 8 hours F. 15ml opaque bottle by Bausch & Lomb G. Soothe (unit dose) contains glycerin and propylene glycols XII. Lovaza (Omega-3-acid ethyl esters) A. Dramatically reduces very high triglycerides in patients with TG > 500 mg/dl B. Available by prescription C. Contains Eicosapentaenoic acid (EPA) 465 mg and Docosahexaenoic acid (DHA) 375 mg D. Highly purified in patented process E. Monitor patients if on anticoagulants F. Pregnancy category C G. Available in 1000 mg capsules by Reliant XIII. Pharmacology of Hydroxychloroquine A. An anti-malarial drug originally B. Used to treat rheumatoid arthritis and lupus C. Mechanism of action is unknown D. Comes in 200 mg non-scored white tablets E. Usual dose is two, 200 mg. tabs per day F. Cleared via renal and hepatic tissues G. Has long tissue clearance, therefore dosing can be titrated by varying the dose on different days of the week H. Screening could be rationally stopped if physicians dosed properly! XIV. Perspective on Hydroxychloroquine (Plaquenil) A. RARE cause of maculopathy (always bilateral) B. Maculopathy results from overdose! C. Lean weight less than 135 lbs increases risk with 400 mg/d dosing D. Obesity is risk factor because drug only accumulates on lean tissue XV. E. Risk slightly increases after 5 years of exposure F. Paracentral scotomas occur before ophthalmoscopic changes Screening for Hydroxychloroquine Maculopathy A. Baseline exam should be within a few months of therapy B. Annual screening is plenty adequate in almost all cases C. Clinical exam 1. BVA 2. Dilated corneal and macular evaluation 3. Photo document any abnormal macular findings 4. 10-2 threshold perimetry (Zeiss/Humphrey is standard) D. If any questionable findings, re-evaluate in 3 months E. XVI. Maculopathy can worsen for months after cessation of drug Tamoxifen A. A nonsteroidal antiestrogenic agent B. Common medical therapy in breast cancer care C. Eye side effects rare, only seen after 1-2 years D. Macula: small, reflectile granular deposits (Fool’s gold crystals) E. XVII. Dosage usually 10-20 mg bid for 5 years Valacyclovir vs. Acyclovir for Recurrent HSV A. “One-year suppression therapy with oral valacyclovir (500-mg tablet daily) was shown to be as effective and as well-tolerated as acyclovir (400-mg tablet twice daily) in reducing the rate of recurrent ocular HSV disease.” XVIII. Zostavax A. Vaccine for prevention of shingles in adults age 60 and older B. Marketed by Merck as Zostavax and is given as a single dose by injection C. Anyone who has been infected by chicken pox (more than 90% of adults in US) is at risk for developing shingles D. Contraindicated if history of allergy to gelatin, neomycin; history of acquired immunodeficiency states; pregnancy XIX. E. In landmark Shingles Prevention Study, Zostavax reduced risk of developing shingles by 51% (4 yrs of follow-up) F. Duration of protection after vaccination unknown Adult Chlamydial Conjunctivitis A. Diagnosis can be challenging early on, but is very straight-forward after a couple of weeks B. Etiology is Chlamydia trachomatis, a common sexually transmitted genitourinary disease C. Giant follicles in lower forniceal conjunctiva D. Moderate papillae on upper tarsal conjunctiva E. Mild epithelial keratitis; possibly some infiltrates F. Treatment is azithromycin (Zithromax) four 250 mg or two 500 mg capsules/tablets (1 gm) or 1 gm oral suspension package XX. Psittacosis A. Another rare expression of Chlamydia trachomatous organisms is psittacosis. This microorganism is spread via parakeet feces and can cause a clinical picture of “Chlamydia conjunctivitis.” When you are absolutely certain of Chlamydia causation, and truly convinced of non-venereal transmission, then consider this remote possibility. XXI. Corneal Foreign Body A. Take good history to help rule out penetration B. Remove foreign body and corneal rust deposits C. Cycloplege to prevent or treat secondary iritis D. Do thorough intraocular exam with BIO E. Advise patient of likely secondary iritis F. Prophylactic antibiotic drops +/- NSAID drops G. F/U until epithelial integrity re-established XXII. Bell’s Palsy A. Abrupt onset facial (7th) nerve palsy B. Muscle tone to lower lid temporarily lost C. Vast majority of patients gain full recovery D. Key is hydration and lubrication of cornea E. Treatment F. PF artificial tears frequently by day and PF ointment (with our without lid taping hs) G. Prednisone and Acyclovir XXIII. Bell’s Palsy Update A. “Early Treatment with Prednisolone or Acyclovir in Bell’s Palsy.” New England Journal of Medicine, Oct 18, 2007 B. 496 patients with idiopathic facial paralysis randomized to Prednisolone, ACV, both, placebo C. Results: After 9 months, recovered facial function 95% Prednisolone, 81% No Prednisolone, 85% for ACV, 90% no ACV, 93% Both D. Conclusion: “In patients with Bell’s palsy, early treatment with prednisolone significantly improves the chances of complete recovery at 3 and 9 months. There is no evidence of a benefit of acyclovir given alone or an additional benefit of acyclovir in combination with prednisolone.”