* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download benzodiazepines - Website of Neelay Gandhi
Survey
Document related concepts
Orphan drug wikipedia , lookup
Psychedelic therapy wikipedia , lookup
Serotonin syndrome wikipedia , lookup
Drug design wikipedia , lookup
Atypical antipsychotic wikipedia , lookup
Drug discovery wikipedia , lookup
Polysubstance dependence wikipedia , lookup
Theralizumab wikipedia , lookup
Pharmacokinetics wikipedia , lookup
Pharmaceutical industry wikipedia , lookup
Pharmacognosy wikipedia , lookup
Prescription drug prices in the United States wikipedia , lookup
Prescription costs wikipedia , lookup
Pharmacogenomics wikipedia , lookup
Neuropharmacology wikipedia , lookup
Drug interaction wikipedia , lookup
Transcript
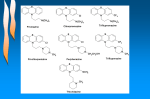
PSYCHOACTIVE, NEUROLEPTIC , ANTIDEPRESSANT DRUGS BENZODIAZEPINES MECHANISM OF ACTION -benzo’s bind to specific high affinity sites on the cell membrane adjacent to receptor for GABA ehances affinity of GABA receptors more frequent opening of chloride channels WITHDRAWAL SYNDROME USES: PROFESSIONAL USES: UNPROFESSIONAL DURATION OF ACTION ACUTE ADVERSE EFFECTS LONG TERM ADVERSE EFFECTS 1. Anxiolytic (severe): selectively inhibiting neuronal circuits in limbic system of brain 2. Sedative/Hypnotic (insomnia, night terrors, sleep walking) 3. Anticonvulsive: treat or interrupt seizures (eclampsia) 4. Central Muscle Relaxant (pre medication before general anesthesia): - relaxes spasticity of skeletal muscles; -↑ presynaptic inhibition in spinal cord 5. Symptomatic emergency treatment of withdrawal syndromes 6. Diverse emergency indications (MI, arrhythmia) 7. Co-medication w/neuroleptics, lithium, antidepressants NOT ANTIPSYCHOTIC, NOT ANTIDEPRESSANT 1. Use with caution: -Psychovegetative disorders: -irritable bowel syndrome, gastric ulcer, PMS, chronic fatigue syndrome -Social performance anxiety 2. Absolute NO-NO’s -analgesia -proper medical treatment of disease -psychosocial or psychiatric assistance Diazepam Long acting; long acting metabolites Chlordiazepoxide Intermediate-acting; long acting metabolites Oxazepam Temazepam Intermediate acting (t1/2 about 10-12 hrs) Lorazepam Clonazepam Triazolam Alprazolam Short acting Midazolam 1. CNS depression (no problem with therapeutic doses) -drowsiness, sedation -ataxia -vertigo, headache, confusion, slurred speech -decrease under continuous administration 2. Respiratory depression/Hypotension -seen w/high i.v. doses or in combo w/other sedatives -normally absent in anxiolytic-sedative-hypnotic doses -relevant in cases of predisposition 3. Amnesia: (retrograde and anterograde – more frequent w/short acting) 4. Paradoxical excitement: -hostility, aggression, disinhibition -seen w/predisposing factors (organic brain disease, central anticholinergic syndrome) 1. Addiction/dependency: **Low dose dependency: -benzo is prescribed for valid medical reasons -low dose intensity, no increase in doses -full patient compliance **Conventional dependency: -benzos may or may not be prescribed for valid medical reasons -increasing doses required, indicating tolerance -black market benzos may be used to cover demand -Alcohol is often abused as amplifier 2. Sleep disturbances (same as alcohol) -REM sleep suppressed (sleep less refreshing) -REM – rebound (nightmares) at discontinuation 3. Amotivational syndrome: -may be long term high dose exposure -less pronounced than w/cannabinoids 1 BENZO’S DURING PREGNANCY BENZO’S AND SEXUAL DYSFUNCTION DRUG INTERACTIONS PSYCHOACTIVE, NEUROLEPTIC , ANTIDEPRESSANT DRUGS 1. Teratogenic potential -generally recognized as safe -weak ass. w/cleft palate 2. Perinatal period: -floppy baby syndrome -withdrawal syndrome (presents weeks later due to long half life of benzo’s) 3. Breast feeding: -Oxazepam, Lorazepam, Alprazolam, Midazolam = limited distribution into breast milk (American Academy of Peds advise against prescribing benzo’s to nursing mothers) 1. Endocrine: slight inhibition of steroid metabolism 2. Libido: -Decreases as a usual side effect of all sedatives at normal to high doses -Performance anxiety/Psychosocial inhibition: -low to mod doses of benzo’s may restore or improve sexual dysfunction **Alcohol: acute low dose is comparable **Cocaine: CNS stimulant directly increases drive but severely inhibits sexual function Enhanced sedation, respiratory and/or cardiovascular depression occurs in combination w/other CNS depressant drugs: -alcohol -antidepressants -antiepileptics -antihistamines -general anesthetics -neuroleptics/antipsychotics -opioid analgesics -other sedatives **All except for alcohol are manageable by clinical monitoring 2 PSYCHOACTIVE, NEUROLEPTIC , ANTIDEPRESSANT DRUGS DRUG PK -i.v. -hepatic elimination -t1/2= short (<1.5 hrs) FLUMAZENILE PD -blocks many actions of: -benzo’s -zolpidem -zaleplon reversal of sedation, hypnosis, narcosis improvement of respiratory depression -ineffective w/other sedativehypnotics, opioids, general anesthetics or alcohol USES 1. To reverse CNS depression after benzo overdose 2. To hasten recovery following use of benzo’s for anesthetic and diagnostic procedures ADVERSE EFFECTS 1. Agitation 2. Confusion 3. Dizziness 4. Nausea 5. Anxiety BUSPIRONE BARBITUATES CHLORAL HYDRATE MEPROBAMATE (MILTOWN) -p.o. -short acting -(1-4 hrs) -hepatic metabolism -p.o. -high first pass -hepatic metabolism -major metabolite = α2 blocker -liver dysfunction may ↓ clearance -i.v./p.o./i.m./rectal -hepatic metabolism -hep enzyme inducer -long half lives -watch 4 accumulation -p.o./rectal -t1/2= 5-10 hrs -converted to active compound trichloroethanol -p.o. -t1/2= 6-17 hrs 2. observe possible protective effects of benzo’s in mixed (suicidal) intoxications (tricyclic antidep + benzos) 3. CI in benzo addiction severe w/drawal syndrome (including convulsions) BENZO ANTAGONIST ZOLPIDEM ZALEPLON CONTRAINDICATIONS 1. Beware of short half life, to avoid, re-sedation, repeated dosing is required -drugs bind to BZ1 (benzo agonist) -effects mostly as for benzo’s -as for benzos at equivalent/effective doses -anxiolytic w/out marked sedative or euphoric effects -unlike benzo’s -effects take > 7 days to establish -no rebound anxiety -no w/drawal syndrome -no potentiation w/sedatives -less psychomotor impairment -reversible depression of activity of all excitable tissue -CNS most sensitive -CV system least sensitive, but affected in intoxication -Compared to Benzo’s: -low selectivity -low therapeutic index -same tolerance, abuse pot. 1. Tachycardia 2. Palpitations 3. Nervousness 4. GI distress 1. Respiratory ↓ 2. Paradoxial excitement 3. After-effects (hangover) 4. Drug interactions w/centrally active drugs 5. Pain (↓pain threshold) 6. Hypersensitivity 7. Tends to accumulate: accidental o/d; intoxication 1. Bad taste 2. Hepatic damage 3. Severe withdrawal Anti-anxiety agent introduced in 50’s; widely used as nighttime sedative, high abuse potential, street drug 1. More generalized CNS depression than benzo’s, but less complete than with barbituates 3 PSYCHOACTIVE, NEUROLEPTIC , ANTIDEPRESSANT DRUGS NEUROLEPTICS: CONVENTIONAL ANTYPSYCHOTICS/NEUROLEPTICS SCHIZOPHRENIA NEUROLEPTIC DRUG INDUCED RECEPTOR BLOCKADE ANTIPSYCHOTIC ACTIONS OF NEUROLEPTICS MAJOR ADVERSE EFFECTS OF NEUROLEPTICS 1. Chlorpromazine 2. Fluphenazin PHENOTHIAZINES 3. Prochlorperazine 4. Promethazine 5. Thioridazine BUTYROPHENONES 6. Haloperidol THIOXANTHENES 7. Thiotixene 8. Clozapine ATYPICAL ANTIPSYCHOTICS, 9. Olanzapine HETEROCYCLICS 10. Quetiapine 11. Risperidone 12. Lithium Common and serious mental disorder characterized by: -loss of contact with reality (psychosis) -false perceptions (hallucinations) -false beliefs (delusions) -abnormal thinking -restricted range of emotions (flattened effect) -diminished motivation, disturbed work and social functioning Subtypes: -Paranoid -Disorganized -Catatonic -Undifferentiated Dopamine D2 block Virtually all neuroleptics Dopamine D4 block Clozapine Α-adrenergic block All neuroleptics listed especially, Phenotiazines, Thiothixene 5-HT block Atypical neuroleptics, not haloperidol Muscarinergic block All neuroleptics, except haloperidol Histamine H1 block All neuroleptics except haloperidol 1. Gradual reduction of hallucinations and delusions 2. Reduction of agitation, emotional upset 3. Reduction of spontaneous physical movement 4. Patient relieved from stressful experience, inner conflict, terror, anxiety reconciliation w/reality improvement of psychosis NO: -anxiolysis -euphoria -improvement of mood Intellectual and sensory functions intact Psychochemical straightjacket Most adverse effects occur early, antipsychotic effects take weeks severe impairment of quality of life 1. Extrapyramidal motor effects: -acute dystonias (mouth, face, eye) which the patient is fully aware of and has not control over it at all; very embarrassing to patient (responsive to anticholinergic drugs) -Parkinson-like bradykinesia, rigor, tremor (responsive to anti-cholinergic drugs) -Motor restlessness (akathisia) (responsive to anticholinergic drugs) -Tardive dyskinesia: after long term treatment, may be slowly reversible or irreversible (not responsive to anti-cholinergic drugs; may actually worsen symptoms) 2. Reduction of autonomous nervous system activity -central anticholinergic (blurred vision, dry mouth, sedation, confusion) -anticholinergic (GI, UT) -antiadrenergic (orthostatic hypotension, lightheadedness) -impairment of body temperature regulation 2. Endocrine -hyperprolactinemia -amenorrhea, galactorrhea, infertility, impotence, loss of libido 3. Blood dyskrasias: especially Clozapine 4. Seizure threshold is lowered 4 PSYCHOACTIVE, NEUROLEPTIC , ANTIDEPRESSANT DRUGS DRUG PK PD USES 1. Acute Psychosis -low potency neuroleptic drug, D1 and D2 antagonist -p.o./i.m./i.v./rectal -stimulates prolactin secretion CHLORPROMAZINE (CPZ) 2. Acute/Chronic schizophrenia 3. Manic phase of manic depression -hepatic metabolism -antiemetic, 5HT blocking -weak antihistaminic 4. Control severely disturbed, agitated/ violent behavior -sedative (subject to tolerance) 5. Intractable hiccup -t1/2= 30 hrs -plasma binding >95% 6. Adjunct tx of severe anxiety HALOPERIDOL -p.o./i.m comparable to (CPZ) 1. DOC: strong antipsychotic effect is requrd -blocks D2, D4, 5-HT & others -effective in therapy-resistant cases -anticholinergic, antiadrenergic -sedative CLOZAPINE LITHIUM -high potency neuroleptic drug -p.o. w/in 6-8 hrs -t1/2= 30 hrs -renal excretion (70% tubular reabsptn, ↑ed in hyponatremia) -↑ Li plasma levels w/ NSAIDs, diuretics, Na restriction -saline infusions facilitate elimination -dialysis: remove Li Hypothetical: competition w/sodium explains side effects 1. Mood stabilizer -prophyl of mania -prophyl of manic dep -prophyl of recurrent unipolar depression -tx of mania w/adjunct meds ADVERSE EFFECTS 1. Lesser degree of central sedation than barbiturates or benzos 2. Tolerance = fast 3. Antimuscarinergic: -mydriasis -blurred vision -dry mouth -difficulty w/peeing 4. CV: -tachycardia -EKG changes -ortho hypotension 5. CNS: -confusion -delirium -insomnia -nightmares -depression (sign of o/d) -catatonic-like states (stiff inside and out; can’t move/emotion less) -hypothermia 6. Extrapyramidal dysfunction a. Acute dystonia -muscles of face/neck/trunk -jaw clenching -oral dystonia -pharyngeal dystonia = fatal -tx: antimuscarinics, benzo Same as for CPZ More pronounced EPM syn 1. EPM: symptoms absent (pre-existing tardive dyskinesia may even improve) 2. Grandulocytopenia (1%/pt yr) 3. Convulsions (3%/pt yr) 1. Initial nausea, diarrhea, muscle wkness, dazed feeling 2. Therapeutic levels: -fine hand tremors -polyuria, polydipsia -wt gain, edema, no diuretics -skin disorders worsen -EKG changes (T depression) -hypothyroidism OTHER b. Akathisia: -mental/motor restlessness -tx: antimusc, propran, benzos c. Parkinsonism: (reversible) -rigor/tremor/akinesis -tx: antimuscarinics d. Tardive dyskinesia: -irreversible -orofacial dyskinesias -protrusion of tongue -lateral chewing -pouting of lips -tx: none; avoid antimusc -prvnt: clozapine/risperidone as antispychotics 7. Convulsions 8. Neuroleptic malignant syndrome: -hyperthermia -severe extrapyramidal sx’s -impaired consciousness -mus rigidity & sk. mus dmg -autonomic dysfunction -tx: discontinue NL, symptomatic tx CI in children due to EPM syn -prototype butyrophenone NL Related drug: Olanzapine: less blood dyskrasias -narrow margin of safety -effects delayed by 8-10 days Toxic: -hyperreflexia -severe GI symptoms -ataxia, blurred vision -tinnitus, syncope toxic psychosis, circulatory failure, coma 5 PSYCHOACTIVE, NEUROLEPTIC , ANTIDEPRESSANT DRUGS ANTI-DEPRESSANT DRUGS ANTIDEPRESSANT DRUGS: DRUG LIST COMMON CLINICAL FEATURES OF ANTIDEPRESSANTS AMINE UPTAKE BLOCKING DRUGS Α2 RECEPTOR AGONIST MAO INHIBITORS Tricyclics: -Amitriptyline Clonidine Phenelzine -Doxepin Tranycypromine -Desipramin -Imipramin -Protriptylin -Nortriptylin Heterocyclics(2nd gen) -Amoxapine -Bupropion -Trazodone -Maprotiline Heterocyclics (3rd gen) -Mirtazapine -Nefazodone -Venlafaxine 5-HT SSRI -Fluoxetine -Paroxetine -Citalopram -Sertraline 1. High rate of non-responders 2. Highly variant array of drug; receptor interactions for each drug: -very complex, mainly hypothetical mechanisms of action -non-responders to one drug in a class may respond to another drug in the same class -choice of drug requires specialist experience -complex and variant pattern of adverse effects 3. Sequential onset of effects -some adverse effects occur immediately -suppressed mental and physical activity is restored soon (w/in days) -anxiolytic & mood elevating effects (takes >2 wks to become effective) Consequences: Simplifying hypothesis of action are untenable ??? Initial antidepressant therapy aggravates the risk of suicide, since activity is restored long before anxiety and negative mood are improved 6 DRUG AMITRYPTILINE PK -p.o. -low and inconsistent BA -t1/2= 20 hrs -metabolites = 30hrs -hepatic cyt P450 mets -renal elimination 2ND AND 3RD GENERATION ANTIDEPRESSANTS Improved PK: -acclerated elimination -less interactions FLUOXETINE -slowly metabolized by P450 t1/2 = up to 10 days -active met = 3-30 days equilibrium of plasma levels after many weeks many PK interactions PHENELZINE TRANYLCYPROMINE PD -p.o. -rapidly excreted in urine -biological t1/2=1-3 wks Improved spectrum of effects: combo of some sedative, anxiolytic, or neuroleptic effects w/antidepressant qualities PSYCHOACTIVE, NEUROLEPTIC , ANTIDEPRESSANT DRUGS ADVERSE EFFECTS OTHER Precautions: 1. Sedation 2. Antimuscarinic -cardiac disease 3. Ortho hypotension -hepatic dysfunction (blockade of alpha -bipolar disease (may receptors) precipitate mania) Sx’s of intoxication: 4. Cardiovascular 1. severe major (tachycardia, AV block) -agitation, delirium depression 5. CNS -tremor, convulsions 2. neuropathic pain 6. Leukopenia -resp depression 7. Symptoms abrupt at -cardiac conduction w/drawal defects and severe CI: arrhythmia -therapy w/MAO inhib. -circulatory collapse -intox w/sedatives/OH -coma -glaucoma, prostatic Triad: Cardiotoxicity, adenoma Convulsions, Coma Improved toxicities: Frequent disadvantages -less autonomous AE -incr blood dyskrasias -less impairment of sexual -seizure threshold dysfunctions lowered USES 1. most frequently prescribed antidepressant drug -MAO-inhibitors (almost irreversible) -MAO-A -MAO-B 2. major depression 3. bulimia, anorexia, OCD 4. social anxiety d/o? 5. PMS ? -if unresponsive or allergic to 1st choice -special subypes of depression, when stimulant effect is particularly beneficial -anxiety -insomnia -wt loss, ↓ appetite, -anorexia -tremors -loss of libido/sexual dysf. -nausea NO anticholinergic effects NO ortho hypotension NO wt gain NO arrhythmia at O/D 1. Persist for wks after discontinuation 2. Cheese syndrome: Tyramine massive release of catecholamines Hypertension Arrtythmia Nausea Headache Stroke Serotonin Syndrome: Caused by combo of SSRI and MAO inhib -↑5HT stores and inhibition of reuptake massive increase of serotonin at synapses -hyperthermia -muscle rigidity -myoclonus, seizures -imparied mntl status -autonomous decompensation Tx: symptomatic, 5HT blocker (cyproheptadine) O/D: seizures, mild w/drawal syndrome 7