* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Prognostic value of T peak-to-end Interval for risk stratification after
Remote ischemic conditioning wikipedia , lookup
Jatene procedure wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Coronary artery disease wikipedia , lookup
Electrocardiography wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Management of acute coronary syndrome wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
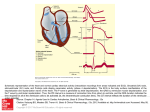
Prognostic value of T peak-to-end Interval for risk stratification after acute myocardial infarction Tarek A. Rahman,MD – Minia University Hospital – Egypt Abstract Aim: Fatal Arrhythmia is the main cause of sudden death in patients with acute myocardial infarction either during hospital admission or in post-discharge period. Our aim is to identify groups at high risk of arrhythmic mortality by using a simple bed-side test in Electrocardiogram. Background: Trans-mural dispersion of repolarization (TDR) in patients with ST elevation myocardial infarction is the main trigger of arrhythmias. The potential value of measuring the interval between the peak and end of the T wave (Tpeak-Tend, Tp-Te) as an index of spatial dispersion of repolarization is a parameter thought to be capable of reflecting dispersion of repolarization and thus may be prognostic tool for detection of arrhythmic risk. Little is known about its use for identifying risk of arrhythmias in acute myocardial infarction and this must be approached with great caution and require careful validation. Methods: A prospective analysis of data from 564 patients admitted to our CCU by acute myocardial infarction along a period of two years from January 2012 to December 2013 was done. After exclusion of valvular, congenital lesions, HOCM, IDCM, pericardial diseases, accessory pathway, any Bundle branch block, metabolic disorders and re-perfusion arrhythmia. Analysis of TpTe interval and its dispersion was done for all patients and a Holter-24h was performed after one month. Patients were then classified into two groups based on Lown grading score for arrhythmia: Group-I (441 patients) with no or minimal arrhythmias (Lown score <3), and Group-II (123) with high grade arrhythmias (Lown score ≥3). Inhospital predischarge echocardiography was done for all patients to evaluate left ventricular functions and presence of myocardial aneurysm. Signal average ECG was done to detect low amplitude signals (LAS). Pre-disharge coronary angiography was done for all patients. Results: Statistical analysis of the results revealed that, Group (II) patients carry a significantly higher numbers of obese, diabetic, and hypertensive patients. Most of patients in this group were smokers, having a higher creatinine levels, and exposed previously to cerebral insults in a significantly higher values than group (I) .Also, group (II) patients need a significantly higher doses of diuretic and ACEIs than group (I). The percentage of anterior wall infarction is significantly higher in group (II), with higher inferior wall affection in group (I). TpTe interval and dispersion between both groups revealed that, a higher TpTe interval was found in group (II) than group (I) and this was linked to occurrence of sudden death or malignant VT and deterioration in Lv functions than in group (I). Also, patients in group-II exposed to re-infarction and cardiogenic shock in a statistically significant values (p<0.01) than group (I). Strong correlation is present between prolonged TpTe and presence of late potentials in SAECG. Conclusion: TpTe was significantly and independently associated with increased odds of SCD and is linked to deterioration of Lv functions and myocardial aneurysms. It's highly correlated to presence of LAS and associate with seveity of cornary lesions. Patients with prolonged TpTe intervals and dispersions were likely to develop fatal arrhythmias. Key Indexing Terms: Tp-Te interval – Ventricular arrhythmias - sudden death - Heart failure Tarek M. AbdelRahman,MD Department of Cardiology, Faculty of Medicine, El-Minia University, El-Minia, Egypt e-mail: [email protected] Abbreviations and Acronyms AP - action potential ECG - electrocardiogram STEMI – ST elevation myocardial infarction TDR - transmural dispersion of repolarization Tp-Te - Tpeak-Tend interval VF - ventricular fibrillation VT - ventricular tachycardia EAD – early after depolarization LAS – low amplitude signals AMI – acute myocardial infarction Introduction: Amplification of spatial dispersion of repolarization, particularly transmural dispersion of repolarization (TDR), within the ventricular myocardium has been suggested to underlie arrhythmogenesis in different cardiac diseases, such as the Brugada, short QT, long QT syndromes, and Catecholaminergic Polymorphic Ventricular Tachycardia (CPVT).(1) Numerous studies (2,3) have highlighted the heterogeneity that exists among the cells that comprise ventricular myocardium, demonstrating unique electrophysiologic and pharmacologic profiles for epicardial, endocardial, and M cells in a number of species, including man. Differences in the time-course of repolarization of these three predominant ventricular myocardial cell types contribute prominently to the inscription of the electrocardiographic T wave recorded in the precordial leads V5 These differences in action potential (AP) morphology lead to the development of opposing voltage gradients on either side of the M region, which contribute to inscription of the T wave, especially those inscribed in the precordial leads (Fig. 1). The interplay between these opposing transmural forces determines the height and width of the T wave and the extent to which the T wave may be interrupted, resulting in a bifid or notched appearance.(4) Figure 1: Voltage gradients on either side of the M region are responsible for inscription of the electrocardiographic T wave Recent studies have identified TDR and other forms of spatial dispersion of repolarization as the principal substrate and early afterdepolarization (EAD)-induced extrasystoles as the most common trigger for the development of lethal arrhythmias.(5) During bradycardia or because of a repolarization-prolonging insult, the action potential of the M cells is more vulnerable to prolongation compared with the other 2 cell types,(6) likely because of larger late-sodium and sodium/calcium exchange currents and a weaker, slowly activating delayed rectifier current.(7) TpTe corresponds with transmural dispersion of repolarization in the ventricular myocardium, a period during which the epicardium has repolarized and is fully excitable, but the M cells are still in the process of repolarization and are vulnerable to the occurrence of early afterdepolarizations.(8,9) One of the challenges ahead is to identify a means to quantitate spatial dispersion of repolarization and TDR non-invasively. In this study, we discuss the potential value of the interval between the peak and end of the T wave (Tpeak-Tend, Tp-Te) as an index of spatial dispersion of repolarization in patients with ST elevation myocardial infarction and to stratify them according to the risk of ventricular arrhythmias. This parameter is thought to be capable of reflecting changes in spatial dispersion of repolarization, including TDR, and thus may be prognostic tool for detection of arrhythmic risk under a variety of conditions.(10) Little is known about its use for identifying risk of arrhythmias in acute myocardial infarction and this must be approached with great caution and require careful validation. Because of the interval from the peak of the T wave to the end of the T wave [TpTe]) is a measure of transmural dispersion of repolarization in the left ventricle, its prolongation representing a period of potential vulnerability for reentrant ventricular arrhythmias.(11) Many studies confirm that, Prolonged TpTe has been associated with increased risk of mortality in congenital and acquired long-QT syndromes, in hypertrophic cardiomyopathy with troponin I mutations, and in patients undergoing primary percutaneous coronary intervention for myocardial infarction.(10-12) There are findings from the bench that link TpTe to mechanisms of ventricular arrhythmia. Using a canine myocardial wedge preparation model, Antzelevitch and coworkers (13,14) explored the genesis of TpTe as well as the potential mechanisms that link TpTe prolongation to increased risk of ventricular arrhythmogenesis. If conditions are favorable, these early afterdepolarizations can lead to reentry and its perpetuation, resulting in polymorphic ventricular tachycardia or ventricular fibrillation. Hence, a prolonged TpTe likely corresponds to an extended vulnerable period and given the right conditions, could increase risk of ventricular arrhythmogenesis.(15) In our study, we try to detect these changes in Tp-Te interval and document its relation to occurrence of different ventricular arrhythmias among patients admitted to our CCU by St-elevation myocardial infarction STEMI. Moreover, to detect its safe and risky limits. Material and methods: Study Participants: A prospective analysis of data from 564 patients admitted to our CCU by acute myocardial infarction along a period of two years from January 2012 to December 2013 was done . Demographic data as regards Age, Sex and BMI. History and clinical examination are taken after their consent, history of co-morbidity, hypertension, diabetes, renal disease, current smoker, previous AMI, previous CABG, Killip class, prior stroke, prior PCI, HF, and shock Exclusion criteria were: valvular and congenital lesions, HOCM, IDCM, pericardial diseases, accessory pathway, any Bundle branch block, any metabolic disorders and re-perfusion arrhythmia . (1) 12-Leads surface ECG: ECG was done for all participants using ECG-machine Fukuda Denshi Climax machine.(filter range 0.5 Hz to 150 Hz, AC filter 60 Hz, 25 mm/s, 10 mm/mV), Measurements of TpTe intervals and its dispersion were conducted manually using digital onscreen software at a pre-discharge day and in a stable clinical conditions. A 12-leads ECG is used and all patients were in sinus rhythm. Measurement of TpTe interval and TpTe dispersion: TpTe interval was measured from Tpeak to Tend n lead V5.(16) If V5 was not suitable, leads V4 and V6 in that order were measured.(10) The end of the T wave was defined as the intersection of the tangent to the down slope of the T wave and the isoelectric line when not followed by a U wave or if distinct from the following U wave. If a U wave followed the T wave, the T-wave offset was measured as the nadir between the T and U waves. (17) If the T-wave amplitude was<1.5 mm in a particular lead, or morphologically distorted that lead was excluded from analysis. For more confirmation we allow a third observer to measure TpTe by subtracting Qp from QT, as shown in figure (2) T-peak-to-T-end dispersion defined as the difference between the maximum and minimum Tpeak-to-T-end interval in all ECG leads. ECG readers were blinded to case status. Figure (2) : Examples of different patients for measurements of QT and TpTe intervals (2) Signal-averaging ECG: SAECG was done for all patients using a commercially available machine ( HP-Page-Writer, Hewlette-Packard, Inc.USA). ECG was recorded in sinus rhythm and signals from a number of beats were averaged to achieve a noise level less than 0.3 uV and then the signals were amplified, digitized and filtered with 40Hz High pass filter-band. The Gomes Criteria was used to identify positive late potentials if ( QRS> 114, RMS-40 uV <20, and LAS40 >38). (3) Trans-thoracic Echocardiography: Echocardiography using a commercially available GE vivid 3 echo machine equipped with 2.5 – 3.5 MHz transducer was done for all patients to examine for LV volumes including (end-diastolic EDV, end-systolic ESV) through which calculation of LVEF% is made by Simpson's Biplane method. Also, recording wall motions abnormalities, Tie index, MR severity and presence of aneurysm. (4) Coronary Angiography: Diagnostic coronary angiography (CA) was done for all patients before discharge using a flatpanel GE-imaging system. All subjects were in the fasting sedated state. CA was performed from the arterial femoral approach after local groin infiltration of 10-20 ml xylocaine 2% using modified seldinger's technique after injection of 5000 IU of Heparin, 6F JL then JR coronary catheters were used to engage the corresponding arteries. The study was conducted with a General Electric Innova 2000 angiographic unit (GE medical system Milwaukee, WI, USA). (5) Holter-24h Monitorring : The patients were seen one month after hospital discharge in the arrhythmia outpatient clinic to receive a Holter-machine. Holter-24h-monitoring and Analysis was done using cardioline Holter Scanning System (cardioline, SPA, Italy) which consisted of a recorder, analyzer, electrocardiogram writer and reporter. The recorder is a battery-operated device , which continuously records ECG signals on a magnetic tape for subsequent analysis. It permitted continuous recording of two separate ECG leads for 24 hours. Analysis of the recordings was accomplished with ECG analyzer of Cardio-line system, which allowed playback of tapes at high speed and full arrhythmia analysis after elimination of artifacts to detect any ventricular arrhythmias. The tapes were subsequently analyzed by the Marquette 8000 laser scanner run with its arrhythmia analysis program to identify and label each QRS complex. The data file was over read and corrected when appropriate by one of the investigators who was unaware of the clinical course of the patients. All episodes of nonfatal arrhythmic events, re-infarction, and revascularization procedures were carefully recorded. Information about deceased patients was obtained from family members, their general practitioners, and the hospitals they had been admitted to. Particular attention was given to the circumstances of each death. The primary end point of the study was prospectively defined as a composite end point of all-cause mortality, documented sustained VT, and resuscitated ventricular fibrillation. Secondary end points of the study were (1) all-cause mortality and (2) arrhythmic events (defined as sudden cardiac death, documented sustained VT, and resuscitated ventricular fibrillation). Sudden death was defined as instantaneous, unexpected death or death within 1 hour of symptom onset not related to circulatory failure. Sustained VT was defined as a documented tachycardia of ventricular origin at a rate of≥100 bpm and lasting for >30 seconds or resulting in hemodynamic collapse Documentation of ventricular arrhythmias is recorded and patients were classified according to Lown grading score (18) into two groups. Group-I: with Lown score less than 3 with no or minor arrhythmias and group-II with high grade arrhythmias of Lown score ≥ 3 The Lown-grading system to evaluate the ventricular premature beats as follows: grade 0= no ventricular premature beats, grade 1= lower than 30 ventricular premature beats/hr, grade 2= more than 1 ventricular premature beats/min or 30 ventricular premature beats/hr, grade 3= multiform ventricular premature beats or ventricular couplets were present, grade 4= 4A = repetitive VPBs - couplets (2 in a row) 4B = repetitive VBPs - runs of ventricular tachycardia (3 in a row) grade 5= early-cycle ventricular premature beats (R on T phenomenon) Statistical Methods: Data were collected and analyzed by Statistical Package for Social Sciences (SPSS) version 13 Data are given as mean (SD) for both numbers and percentages and compared using Chi-square and the Student t test. A probability level of p-value ≤ 0.05 was considered as statistically significant in all tests. Correlation between TpTe and both SAECG and severity of cornary lesions were made using the Pearson correlation coefficient (r). Limitations: As is the case for QTc, the difficulty in locating T-wave end when the T-wave morphology is flat or multiphasic may affect TpTe measurements. However, we overcome this by measuring the dispersion of Tp-Te interval. Readers were blinded, so any such errors would be unrelated to case status. Therefore, any bias introduced by this error would be unlikely to affect the validity of the findings. A subset of patients may be skipped from research because a high percent of SCD may be unfortunate first manifestation of their illness and are unlikely to have undergone any cardiac investigations. Finally, a large number of cases is essential to clarify a cut-off value and a percentile for which risk is inevitable. Results Patients demographic data, Co-morbidity and medications are listed in Table (I). Group (I): N= 441 (78.2%) Age (yrs) 52 ± 4 Height (cm) 167 ± 4 Weight (kg) 85 ± 2 BMI (kg/m2) 29.2 ± 4 Gender male, n (%) 361 (81%) Hypertension, n (%) 272 (61%) Diabetes mellitus, n (%) 283 (64%) Hyperlipidemia, (n %) 382 (86%) Serum creatinine (mg%) 1.3±0.2 Current smoker, n (%) 259 (58%) Previous Stroke, n (%) 6 (1.3%) Medications used during admission period ASA, n (%) 366 (83%) Clopidogrel , n (%) 106 (24%) ACEI, n (%) 194 (44%) ARB, n (%) 128 (29%) B-Blockers, n (%) 392 (89%) CCB, n (%) 71 (16%) Statin, n (%) 163 (37%) Diuretics, n (%) 53 (12%) OAD/Insulin, n (%) 283 (64%) Co-morbidity Demographic Parameter Group (II): N= 123 (21.8%) 50 ± 6 157 ± 8 88 ± 6 34.3 ± 5 98 (80%) 98 (79%) 102 (83%) 108 (87%) 1.5±0.3 90 (73%) 4 (3.2%) NS 0.02 0.06 0.01 NS 0.01 0.01 NS 0.03 0.01 0.01 99 (81%) 27 (22%) 76 (62%) 38 (31%) 107 (87%) 17 (14%) 46 (38%) 78 (64%) 102 (83%) NS NS 0.01 NS NS NS NS 0.01 0.01 P It was shown that, the group (II) carry a significantly higher numbers of obese, diabetic and hypertensive patients. Most of patients in this group were smokers, having a higher creatinine levels and exposed previously to cerebral insults in a significantly higher values than group (I). Also, group (II) patients need a significantly higher doses of diuretic and ACEI than group (I) during the admission period The site of infarction is categorized in table (2): Site of MI Group-B (N=123) 83 (68%) P value Anterior MI Group-A (N=441) 211 (47%) - extensive anterior - antero-septal - antero-lateral Inferior MI 86 (19%) 98 (22%) 27 (6%) 233 (53 %) 44 (35%) 23 (18%) 18 (15%) 40 (32%) 0.01 - localized inferior - infero-lateral - infero-posterior 174 (39%) 35 (8%) 24 (6%) 21 (17%) 11 (9%) 8 (6%) 0.01 It was found that, percentage of anterior wall infarction is significantly high in group (II) representing 68% of cases with higher inferior wall affection in group (I) 53% of cases in a statistically significant value (p 0.01). Figure (3): Localization of infarction site in group (I) and group (II) TpTe interval and dispersion between both groups revealed that, a higher TpTe interval was found in group (II) in a value of 86±16 msec than 62±14 msec in group (I). Also, increased TpTe dispersion in group (II) than group (I) in a value of (26±6 msec & 18±4 msec respectively) as shown in table(3) and figure (4). At the end of the study, we made a correlation between reported cases as sudden death or malignant VT and found all of them having Tp-Te interval more than 100 msec and a dispersion more than 30 msec. Table (3) TpTe interval and dispersion between two groups Parameter TpTe interval (msec) TpTe dispersion (msec) Group (I) N= 441 Mean SD 62 14 18 4 Group (II) N= 123 Mean SD 86 16 26 6 P 0.001 0.001 TpTe interval in both groups TpTe Dispersion in both groups 35 120 30 100 25 80 20 Group-I 60 Group-II Group-I Group-II 15 40 10 20 5 0 0 Figure (4): Tp-Te interval and Tp-Te dispersion in both groups Echocardiographic findings revealed a significant deterioration in Lv functions in group (II) versus group (I) as shown in table (4). Table (4): Echocardiographic findings in both groups Echocardiograhic Finding Lv end diastolic dimension (LVEDD) Lv end systolic dimension (LVESD) Ejection Fraction (EF %) Fractional shortening (FS %) Tei-Index MR jet area width (Cm2) Evidence of myocardial aneurysm Group-I (N=441) 47±1.2 31±1.1 61±4 26±2.1 0.52±0.13 1.5±0.4 0 Group-II (N=123) 56±2.4 45±1.6 44±1.5 16±2.1 0.64±0.68 3.1±0.2 4±0 P value 0.001 0.001 0.001 0.001 0.001 0.001 0.001 Data from admission period and one month Holter-24h monitoring revealed, documented VT in 16 patients in group II versus 9 patients in group I, resuscitated VF in 8 patients in group-II versus only 2 cases in group-I, sudden death in 4 patients in group-II versus only one case in group-I, Re-infarction occurred in 21 case of group-II versus 8 cases in group-I and cardiogenic shock in 23 patients in group-II versus 4 cases in group-I. as shown in figure (5). Arrythmias and sudden death in both groups 25 20 15 group (I) group (II) 10 5 0 Cardiogenic Shock Re-infarction Sudden Death VF VT Figure (5): Arrhythmias and events between both groups SAECG Data revealed increased QRS duration and low amplitude signals with lower RMS-40 in group-II versus group-I in a statistically significant values (p 0.001), as shown in table (5) Table (5): Comparison of SAECG results between the two groups. Parameter QRS duration (msec) RMS-40 (msec) LAS (msec) Group (I) N= 441 Mean SD 96 6 100 12 10 2 Group (II) N= 123 Mean SD 102 10 44 4 36 6 P 0.001 0.001 0.001 Coronary Angiographic results using QCA "quantitative coronary lesion assessment" revealed a severer lesions in Left main territory in group-II than group-I in a statistically significant values (p 0.001). However, group-I showed a higher affection in RCA territory than group-I but, less severe percentage of stenosis in the affected vessels as shown in table (6). Table (6): Comparison of coronary angiographic findings between the two groups. Coronary artery Left Main artery (LM) Left anterior descending A (LAD) Diagonal branch artery (DA) Left circumflex artery (LCx) Obtuse marginal artery (OM) Right coronary artery (RCA) Group (I) N= 441 Mean SD 0 0 40% 10% 50% 10% 60% 10% 50% 10% 60% 10% Group (II) N= 123 Mean SD 40% 10% 80% 15% 90% 10% 45% 5% 40% 5% 40% 10% P 0.001 0.001 0.001 0.001 0.001 0.001 Correlation between TpTe interval and number of LAS in SAECG was made and revealed a strong positive linear correlation between both parameters in (r)= 0.98 and (p) 0.001 as shown in figure (6-A) and a positive correlation between prolonged TpTe and severity of coronary lesions with (r)= 0.96 and (p) 0.001 as shown in figure (6-B). Correlation between TpTe and % of CA stenosis (fig 6-B) Correlation between TpTe and LAS fig-6-A 120 60 40 20 TpTe Interval 80 80 60 40 0 37 33 29 25 21 17 13 Low Amplitude Signals 9 5 1 20 37 33 29 25 21 17 13 9 5 1 TpTe interval Figure (6): Correlation between TpTe and LAS (A) and Percent of coronary stenosis (B) Conclusions: TpTe was significantly and independently associated with increased odds of SCD among subjects with STEMI. Also, increased TpTe interval and dispersion is linked to deterioration of Lv functions and myocardial aneurysm. Arrhythmias were very frequent in a subset of groups that having a prolonged TpTe interval and increased dispersion. TpTe is positively correlated to presence of Late-potentials in SAECG and to the perecent of coronary stenosis in angiographic findings. Measurement may extend the value of repolarization beyond the QTc, particularly in situations where QTc is either normal or not valid because of prolongation of QRSD. Prolonged TpTe has potential for enhancement of SCD and risk stratification and warrants evaluation in additional, larger populations. Discussion Arrhythmic events are likely to occur during the natural course of acute myocardial infarction which may be a direct cause of mortality or deterioration of cardiac functions in such patients. Many studies tried to demonstrate an association between an increase in Tpeak-Tend and arrhythmic risk but they are notwithstanding.(19-21) Direct validation of Tpeak-Tend measured at the body surface as an index of TDR is still lacking and guidelines for such validation have been suggested.(22) Because precordial leads view the electrical field across the ventricular wall, Tpeak-Tend would be expected to be most representative of TDR in these leads. The precordial leads are unipolar leads placed on the chest that are referenced to Wilson central terminal. The direction of these leads is radially toward the "center" of the heart, the center of the Einthoven triangle. Unlike the precordial leads, the bipolar limb leads, including leads I, II, and III, do not look across the ventricular wall. While TpeakTend intervals measured in these limb leads may provide an index of TDR, they are more likely to reflect global dispersion, including apico-basal and interventricular dispersion of repolarization.(23,24) % of Stenosis 100 100 Another important consideration is that TDR can be highly variable in different regions of the ventricular myocardium, particularly under pathophysiologic conditions. Consequently, it is important to measure Tpeak-Tend independently in each of the precordial leads and it is inadvisable to average TpeakTend among several leads.(25) So, in our study we overcome this averaging by measuring the dispersion between the longest and shortest TpTe interval. A large increase in TDR is likely to be arrhythmogenic because the dispersion of repolarization and refractoriness occurs over a very short distance (the width of the ventricular wall), creating a steep repolarization gradient.(26, 27) It is the steepness of the repolarization gradient rather than the total magnitude of dispersion that determines its arrhythmogenic potential. Apico-basal or interventricular dispersion of repolarization is less informative because it may or may not be associated with a steep repolarization gradient and thus may or may not be associated with arrhythmic risk.(26, 27) Our study conclude a direct association between Tp-Te interval prolongation and increased its dispersion to increased events of fatal arrhythmias in group-II patients more than group-I in a statically significant values which confirm increased TDR in group-II. Topilski et al.(11)found that QT, QTc and Tpeak-Tend intervals were strong predictors of Torsade de pointes, with the best single discriminator being a prolonged Tpeak-Tend. Watanabe et al.(27)demonstrated that prolonged Tpeak-Tend is associated with inducibility as well as spontaneous development of ventricular tachycardia (VT) in high risk patients with organic heart disease.(27) We found that, patients in group-II having a prolonged Tp-Te interval in a value of (78±12 msec versus 62±14 msec in group-I and this made them more prone to many arrhythmic events. Lubinski et al(28) observed that patients with CAD and inducible ventricular tachycardia had a higher TpTe (74±14 versus 63±16 ms;P<0.004). In addition he measures TpTe/QT ratio and expressed in his research that a higher percentage (21±4% versus 17±3%;P=0.02) was found in arrhythmic group than those who survived myocardial infarction without inducible ventricular tachycardia.(28) In this study, we tried to detect the value at which Tp-Te interval is risky, and found that, increased Tp-Te interval more than 102 msec and a dispersion more than 36 msec -which is the mean plus two SD- carry an ultimate risk of SD and fatal arrhythmias. In a study made by Harrmark C., et al.,(29) who studied TpTe in acute myocardial infarction. They observed that, a TpTe values >100 ms during acute myocardial infarction and >113 ms in the setting of acquired bradyarrhythmias have been described as “high risk” in the literature. In our study, the majority of subjects with a TpTe value >100 ms were at high risk. Our findings are comparable with a smaller study of patients with acute myocardial infarction that evaluated overall mortality (not SCD) in which 10 of 11 patients who died had TpTe >100 ms.(29) This fact is supported from data by Lubinski et al,(28) who reported that the mean TpTe observed in subjects with CAD and inducible ventricular tachycardia was relatively low (74±14 ms). However, further studies are needed for establishing cutoffs for patients at risk of SCD in the community. In our study, we noticed a high percentage of smokers in group-II who are linked to increased mortality and arrhythmias. This fact is confirmed nowadays by a study made by Hakan Tasolar et. Al.,(30) in 2013 who studied Tp-Te interval in 45 chronic smoker and confirm a direct relationship between smoking and prolongation of Tp-Te interval as a predictor for ventricular arrhythmias and sudden death. (30) In our study, a left ventricular aneurysm was found only in patients of group-II who are characterized by longer Tp-Te interval and increased dispersion and that is confirmed by many authors who reported a link between presence of Lv aneurysm and deterioration of Lv functions and refractory arrhythmias after myocardial infarction. (31,32) Left ventricular structural lesions result in complex electrophysiological changes, but those mainly responsible for arrhythmias are conduction slowing, changes in the refractory period, inhomogeneous activation and repolarization. We review the literature and report our personal experience of the prognostic value of TpTe interval and its dispersion added to Holter and SAECG data and found a strong correlation of prolongation of TpTe to presence of ventricular late potentials. This is supported in a study in 2007 made by Bounhoure et al., who use a programmed ventricular stimulation and succeeded to select the best candidates for defibrillator implantation and resynchronization. (33) Another study made by Chu et al., 2007, to detect the favorable impact of three month statin therapy on arrhythmias and sudden death revealed strong correlation of TpTe and late potentials as non-invasive tools to stratify arrhythmic susceptibility which –by the way- conclude that, the favorable antiarrhythmia effect of atorvastatin (10 mg/day) therapy cannot be directly reflected by analyzing these noninvasive ECG risk stratification parameters in low-risk patients with hypercholesterolemia. (34) References: 1. Antzelevitch C, Oliva A. Amplification of spatial dispersion of repolarization underlies sudden cardiac death associated with catecholaminergic polymorphic VT, long QT, short QT and Brugada syndromes. J Intern Med. 2006;259:48-58. 2. Antzelevitch C, Dumaine R. Electrical heterogeneity in the heart: physiological, pharmacological and clinical implications. In: Page E, Fozzard HA, Solaro RJ, eds. The Cardiovascular System. Volume 1, The Heart.New York: The American Physiological Society by Oxford University Press; 2002:654-692. 3. Akar FG, Yan GX, Antzelevitch C, Rosenbaum DS. Unique topographical distribution of M cells underlies reentrant mechanism of torsade de pointes in the long-QT syndrome. Circulation.2002;105:1247-1253 4. Janse MJ, Sosunov EA, Coronel R, Opthof T, Anyukhovsky EP, de Bakker JM, Plotnikov AN, Shlapakova IN, Danilo P, Jr., Tijssen JG, Rosen MR. Repolarization gradients in the canine left ventricle before and after induction of short-term cardiac memory. Circulation. 2005;112:17111718. 5. Belardinelli L, Antzelevitch C, Vos MA. Assessing predictors of drug-induced torsade de pointes.Trends Pharmacol Sci. 2003;24:619-62 6. Antzelevitch C, Sicouri S, Litovsky SH, Lukas A, Krishnan SC, Di Diego JM, Gintant GA, Liu DW. Heterogeneity within the ventricular wall. Electrophysiology and pharmacology of epicardial, endocardial, and M cells. Circ Res. 1991;69:1427–1449. 7. Antzelevitch C. Role of spatial dispersion of repolarization in inherited and acquired sudden cardiac death syndromes. Am J Physiol Heart Circ Physiol. 2007;293:H2024–H2038. 8. Gupta P, Patel C, Patel H, Narayanaswamy S, Malhotra B, Green JT, Yan GX. T(p-e)/QT ratio as an index of arrhythmogenesis. J Electrocardiol. 2008;41:567–574. 9. Liu T, Brown BS, Wu Y, Antzelevitch C, Kowey PR, Yan GX. Blinded validation of the isolated arterially perfused rabbit ventricular wedge in preclinical assessment of drug-induced proarrhythmias. Heart Rhythm. 2006;3:948 –956. 10. Castro Hevia J, Antzelevitch C, Tornes Barzaga F, Dorantes Sanchez M, Dorticos Balea F, Zayas Molina R, Quinones Perez MA, Fayad Rodriguez Y. Tpeak-Tend and Tpeak-Tend dispersion as risk factors for ventricular tachycardia/ventricular fibrillation in patients with the Brugada syndrome. J Am Coll Cardiol. 2006; 47:1828–1834. 11. Topilski I, Rogowski O, Rosso R, Justo D, Copperman Y, Glikson M, Belhassen B, Hochenberg M, Viskin S. The morphology of the QT interval predicts torsade de pointes during acquired bradyarrhythmias. J Am Coll Cardiol. 2007;49:320 –328. 12. Shimizu M, Ino H, Okeie K, Yamaguchi M, Nagata M, Hayashi K, Itoh H, Iwaki T, Oe K, Konno T, Mabuchi H. T-peak to T-end interval may be a better predictor of high-risk patients with hypertrophic cardiomyopathy associated with a cardiac troponin I mutation than QT dispersion. Clin Cardiol. 2002;25:335–339. 13. Antzelevitch C SW, Yan GX. Electrical heterogeneity and the development of arrhythmias. In Olsson SB, Yuan S, Amlie JP, eds. Dispersion of Ventricular Repolarization: State of the Art. Armonk, NY: Futura Publishing Company; 2000:3–22. 14. Sicouri S, Antzelevitch C. A subpopulation of cells with unique electrophysiological properties in the deep subepicardium of the canine ventricle. The M cell. Circ Res. 1991;68:1729 –1741. 15. Antzelevitch C, Shimizu W, Yan GX, Sicouri S, Weissenburger J, Nesterenko VV, Burashnikov A, Di Diego J, Saffitz J, Thomas GP. The M cell: its contribution to the ECG and to normal and abnormal electrical function of the heart. J Cardiovasc Electrophysiol. 1999;10:1124 –1152. 16. Antzelevitch C, Sicouri S, Di Diego JM, Burashnikov A, Viskin S, Shimizu W, Yan GX, Kowey P, Zhang L. Does Tpeak-Tend provide an index of transmural dispersion of repolarization? Heart Rhythm. 2007;4: 1114–1116. 17. Perkiomaki JS, Koistinen MJ, Yli-Mayry S, Huikuri HV. Dispersion of QT interval in patients with and without susceptibility to ventricular tachyarrhythmias after previous myocardial infarction. J Am Coll Cardiol. 1995;26:174 –179. 18. Lown B, Wolf M. Approaches to sudden death from coronary heart disease. Circulation 1971;44:130-42. 19. Emori T, Antzelevitch C. Cellular basis for complex T waves and arrhythmic activity following combined I(Kr) and I(Ks) block. J Cardiovasc Electrophysiol. 2001;12:1369–1378. 20. Watanabe N, Kobayashi Y, Tanno K, Miyoshi F, Asano T, Kawamura M, Mikami Y, Adachi T, Ryu S, Miyata A, Katagiri T. Transmural dispersion of repolarization and ventricular tachyarrhythmias. J Electrocardiol. 2004;37:191–200 21. Yan GX, Antzelevitch C. Cellular basis for the normal T wave and the electrocardiographic manifestations of the long QT syndrome. Circulation. 1998;98:1928-1936. 22. Antzelevitch C. T peak-Tend interval as an index of transmural dispersion of repolarization. Eur J Clin Invest. 2001;31:555-557. 23. Opthof T, Coronel R, Wilms-Schopman FJ, Plotnikov AN, Shlapakova IN, Danilo P, Jr., Rosen MR, Janse MJ. Dispersion of repolarization in canine ventricle and the electrocardiographic T wave: T(p-e) interval does not reflect transmural dispersion. Heart Rhythm. 2007;4:341-348. 24. Akar FG, Yan GX, Antzelevitch C, Rosenbaum DS. Unique topographical distribution of M cells underlies reentrant mechanism of torsade de pointes in the long-QT syndrome. Circulation.2002;105:1247-1253. 25. Xia Y, Liang Y, Kongstad O, Liao Q, Holm M, Olsson B, Yuan S. In vivo validation of the coincidence of the peak and end of the T wave with full repolarization of the epicardium and endocardium in swine. Heart Rhythm. 2005;2:162-169. 26. Aiba T, Shimizu W, Hidaka I, Uemura K, Noda T, Zheng C, Kamiya A, Inagaki M, Sugimachi M, Sunagawa K. Cellular basis for trigger and maintenance of ventricular fibrillation in the Brugada syndrome model: high-resolution optical mapping study. J Am Coll Cardiol. 2006;47:2074-2085. 27. Watanabe N, Kobayashi Y, Tanno K, Miyoshi F, Asano T, Kawamura M, Mikami Y, Adachi T, Ryu S, Miyata A, Katagiri T. Transmural dispersion of repolarization and ventricular tachyarrhythmias. J Electrocardiol. 2004;37:191-200. 28. Lubinski A, Kornacewicz-Jach Z, Wnuk-Wojnar AM, Adamus J,Kempa M, Krolak T, LewickaNowak E, Radomski M, Swiatecka G. The terminal portion of the T wave: a new electrocardiographic marker of risk of ventricular arrhythmias. Pacing Clin Electrophysiol. 2000;23:1957–1959. 29. Haarmark C, Hansen PR, Vedel-Larsen E, Pedersen SH, Graff C, Andersen MP, Toft E, Wang F,Struijk JJ, Kanters JK. The prognostic value of the Tpeak-Tend interval in patients undergoing primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. J Electrocardiol. 2009; 42:555–560. 30. Hakan Taşolar, Mehmet Ballı, Mustafa Çetin, Burak Altun, Musa Çakıcı, Adil Bayramoğlu, Ömür Otlu and Hasan Pekdemir. Effect of smoking on Tp-e interval, Tp-e/QT and Tp-e/QTc ratios as indices of ventricular arrhythmogenesis. J Am Coll Cardiol. 2013;62(18_S2):C140C140. doi:10.1016/j.jacc.2013.08.420 31. Szymanski D, Borggrefe M, Ulbricht L, Jehle J. Correlations between arrhythmias and left ventricular functions at rest and during stress in patients with postinfarction aneurysm. Z Kardiol. 1993 Apr;82(4):222-8. German. 32. Bigger JT Jr. Relation between left ventricular dysfunction and ventricular arrhythmias after myocardial infarction. Am J Cardiol. 1986 Jan 31;57(3):8B-14B. 33. counhoure JP, Galinier M, Boveda S and Albenque JP. Ventricular arrythmias, sudden death and heart failure. Bull Acad Natl Med. 2010;Jun; 194(6):997-1007 34. Chu CS, Lee KT, Lee ST, Lu YH, Lin TH, Voon WC. Effects of atorvastatin on ventricular late potentials and repolarization dispersion in patients with hypercholesterolemia. Kaohsiung J Med Sci. 2007 May; 23(5):217-24.