* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download GI I and II
Survey
Document related concepts
Transcript
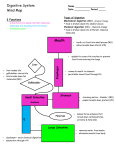
Human Physiology 11/25 - 11/26/08 Jeffrey Weiner GI I and II Objectives- Dr. Brand 1. List the types of neurons that make up the submucosal and myenteric plexuses. a. Submucosal plexus: Contains sensory neurons (chemoreceptors, mechanoreceptors), and vasodilatory neurons b. Myenteric plexus: 2/3 motor neurons - stimulate or inhibit smooth muscle & secretion directly or via interneurons. 1/3 sensory - mechanoreceptors sense stretch or friction. 2. Describe the effects on GI tract function of stimulation by the parasympathetic and sympathetic nervous systems as given in class. a. Increased parasympathetic activity: i. Depolarizes GI smooth muscle cells ii. Increases amplitude & frequency of phasic contractions iii. Decreases tonic contractions of sphincters iv. Stimulates secretion and blood flow (via vasodilatory neurons in the submucosal plexus) b. Increased sympathetic activity: i. Inhibits enteric secretomotor neurons ii. Constricts blood vessels iii. Stimulates sphincters 3. Describe the laryngeal and esophageal phases of the swallowing reflex. a. Pharyngeal Phase: A bolus of chewed food passes into the upper esophagus. The nasopharynx & lungs are protected so food does not enter i. Soft palate moves up to protect the nasopharynx. Vocal chords close, larynx moves up against the epiglottis to protect the lungs. ii. Upper esophageal sphincter (UES) relaxes- gravity and contraction of pharynx move food into esophagus iii. Primary peristaltic wave starts in pharynx and moves to the esophagus b. Esophageal Phase: Bolus of food passes to the stomach i. UES closes to prevent food from moving backward. ii. Primary peristaltic wave moves bolus down esophagus (10 sec) & the lower esophageal sphincter relaxes so food passes into the stomach. 1. Secondary peristaltic wave may occur 4. Describe the function of the fundus, body & antrum of the stomach in gastric motility. a. Fundus and Body- The fundus and the body relax when food enters the stomach. They exhibit weak contractions and are compliant (can accept about 1500 ml with a minimal change in pressure) b. Antrum- Exhibits strong contractions, mixing food and breaking it down into small particles 5. Describe the effects of increased vagal and sympathetic activity, and of gastrin, on the motility of the antrum. a. Increased sympathetic activity, decreased vagal/parasympathetic activity, and increase gastrin will lower antral contraction and raise pyloric contraction 6. Make a diagram showing the endocrine regulation of gastric emptying. Include the effects of fat, acidity, hyperosmolality and peptides and amino acids on the rate of gastric emptying. The diagram should include the receptors, hormonal mediators and effects on antral and pyloric sphincter function. 7. Make a diagram similar to the diagram for objective #6, only showing neural regulation of gastric emptying. 8. Make a diagram of an enterocyte showing how Na, Glucose, K, Cl, HCO 3, and H2O are absorbed in the small intestine (See the slide entitled “Small intestine: mature enterocytes absorb NaCl, water & nutrients”) 9. Make a diagram showing the cellular mechanism of Cl- secretion by immature enterocytes in the crypts of the small intestine. ******** For the past four objectives, see flow charts in the notes********* 10. Name the ionic currents that cause depolarization, plateau phase, and repolarization of a slow wave, and the action potential that occur in GI smooth muscle. a. Slow Wave: i. Depolarization- due to opening of of a nonspecific cation channel, ii. Plateau- due to Ca activated K channels opening iii. Repolarization- calcium channel closes, K channels remain open b. Action Potential: i. Occur in the antrum, small intestine, and large intestine. The up-shoot is due to opening of an L-type Ca channel Human Physiology 11/25 - 11/26/08 Jeffrey Weiner 11. Explain the effect of changes in amplitude and duration of slow waves on the phasic contractions of the GI smooth muscle. a. Increased amplitude of slow wave --> increased force of contraction b. Increased duration of plateau phase --> prolonged contraction 12. Describe the effect of action potentials (spike potentials) on the force of contraction of GI smooth muscle. a. Action potentials usually occur in the antrum and small intestine and increase the force of contractions during ingestion. 13. Describe the effects of parasympathetic and sympathetic stimulation on slow waves, action potentials and force of contraction of GI smooth muscle. a. Parasympathetic stimulation- increase amplitude and duration of slow wave, and force of contraction b. Sympathetic stimulation- opposite 14. Name two major functions of saliva. a. Saliva lubricates food, and contains enzymes that digest starch and lipids (salivary amylase and linguinal lipase) 15. List three effects on the salivary glands of increased parasympathetic stimulation. a. Increased secretion, vasodilation, increased metabolism, and increased growth 16. Diagram the mechanism of H+ secretion by parietal cells. 17. List the three major physiological stimulants of H+ secretion. a. Gastrin (the most potent) b. Acetylcholine from parasympathetic nerves c. Histamine: from mast cells in lamina propria 18. Make a diagram showing the mechanisms regulating H+ secretion during the gastric phase. 19. State where pepsin is synthesized, how it is activated, and what kind of enzyme it is. a. Pepsin is synthesized and secreted by Chief cells in the gastric mucosa. It is secreted as pepsinogen, a proenzyme that is activated only when pH < 5. It is a protein digesting enzyme, and will be deactivated once the pH > 5 in the duodenum. 20. Describe the mechanisms that protect the gastric mucosa from potentially damaging gastric contents. a. Secretion of mucus and HCO3- protect the surface layer of epithelium from gastric acid, pepsin, extreme pH, ethanol, aspirin, ibuprofen, etc 21. List the effects of secretin, cholecystokinin and parasympathetic and sympathetic stimulation on pancreatic acinar and ductal secretions. a. Secretin will act on pancreatic ductal cells to increase aqueous ductal secretion b. Cholecystokinin will act on pancreatic acinar cells to increase enzymatic secretion c. Parasympathetic nerves stimulate exocrine secretion, and sympathetic nerves are inhibitory 22. Describe the effects of acidity, fatty acids, peptides and amino acids on pancreatic secretions. a. Increased H+ (pH < 4.5), will increase aqueous ductal secretion b. Fatty acids, peptides, and amino acids will increase enzymatic secretion from the pancreatic acinar cells 23. Describe the enterohepatic circulation of bile salts. a. Bile salts are synthesized in hepatocytes from cholesterol taken up from the capillaries. It is secreted to the bile canaliculus and combined with H2O, Na+, and HCO3- from bile duct cells b. The bile salts are moved through the hepatic duct to the gall bladder, where they are concentrated by the secretion of Na, H2O, and HCO3- into the duodenum during a meal. c. Bile salts are secreted into the duodenum to help emulsify fats. They are absorbed back into portal circulation (passively or actively) in the ileum. d. In blood circulation they are bound to albumin, and returned to the hepatocytes to start the cycle again. 24. Name the hormone that stimulates fluid and electrolyte secretion by the bile ducts. a. Cholecystokinin 25. List the two main functions of the gall bladder. a. To store, concentrate, and secrete bile into the duodenum. 26. Describe the effect of parasympathetic stimulation and of cholecystokinin on the gall bladder & Sphincter of Oddi a. Cholecystokinin and parasympathetic activity stimulate gall bladder contraction and relax the Sphincter of Oddi. (Sphincter of Oddi controls release of bile into the duodenum). 27. Define the terms digestion, luminal digestion and contact digestion. a. Digestion is the chemical breakdown of food into molecules that can be absorbed Human Physiology 11/25 - 11/26/08 Jeffrey Weiner b. Luminal digestion occurs in the lumen of the gut; enzymes are secreted from the salivary glands, stomach & pancreas. c. Contact digestion occurs via enzymes located on the luminal cell membranes of enterocytes 28. Name the location in the GI tract where bile salts and vitamin B 12 (cobalamin) are absorbed. a. Bile salts and B12 are absorbed in the ileum 29. Describe the role of luminal and contact digestion in digestion of carbohydrates. a. Amylopectin is digested by both luminal and contact digestion i. Amylopectin is digested by α-amylase to give α-limit dextrin and maltose (luminal) ii. Dextrin and maltose are digested by α-dextrinase and maltase, respectively, to form glucose. (contact) b. Sucrose and lactose are both digested by contact digestion i. In the brush border, sucrose is digested by sucrase to give glucose & fructose ii. In the brush border, lactose is digested by lactase to give glucose & galactose 30. Explain the mechanism for absorption of monosaccharides across the intestinal epithelium. a. Glucose and galactose are absorbed actively by an Na +/sugar symport b. Fructose diffuses passively 31. Name the four major pancreatic proteases, and describe how they are converted from pro-enzymes to active enzymes. a. The four major pancreatic proteases are trypsin, chymotrypsin, elastase, and carboxypeptidase. b. The pancreas will secrete trypsinogen, which is converted to trypsin by enterokinase in the brush border. Trypsin will convert all of the other pro-enzymes to the active enzymes 32. Describe the cellular mechanisms of absorption of amino acids and di- and tripeptides in the intestine. a. Di and tripeptides are absorbed across the luminal membrane by cotransport with H+ b. Amino acids are absorbed by cotransport with Na+ 33. Define amphipathic and give examples of amphipathic compounds that affect lipid digestion. a. Amphipathic compounds are molecules with both hydrophilic and hydrophobic portions. i. Examples: lecithin, fatty acids, monoglycerides, some proteins 34. Describe the roles of emulsification and micelles in lipid digestion & absorption. a. Micelles are soluble particles with bile salts & other amphipathic compounds arranged at the outer surface & hydrophobic molecules in the center. b. Micelles contain bile salts, lecithin from bile, FA, monoglycerides, cholesterol & phospholipids c. FA are absorbed from the micelle into the enterocytes, where they are packaged into chylomicra 35. Name the products of triglyceride hydrolysis by pancreatic lipase. a. A triglyceride will yield a 2-monoglyceride and 2 free fatty acids after being hydrolized by pancreatic lipase 36. Describe the path for production of chylomicrons in the enterocyte. a. FA --> TG --- TG + apoproteins ---> Chylomicron 37. Name the form in which most iron is absorbed into the enterocyte in someone ingesting a diet containing meat. a. Food iron is mostly heme iron or Fe+3+ from meat 38. Name two conditions that stimulate iron absorption. a. Gastric acid solubilizes Fe+3, Fe+3 is chelated (by mucin, amino acids, and sugars) and absorbed in the duodenum, and ascorbic acid (Vit. C) will reduce Fe +3 to Fe+2 39. Describe the mechanism providing for Ca++ transport across the brush border and basolateral membranes of the enterocyte. a. Calcium will diffuse across the brush border in the duodenum and jejunem. It is combined with calbindin and absorbed either by the ATPase or the Na/Ca antiport. 40. Name the cells that secrete intrinsic factor, and explain the role of intrinsic factor in the absorption of vitamin B12 a. Parietal cells secrete intrinsic factor, which will complex with B12.