* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Biology 233
Survey
Document related concepts
Transcript
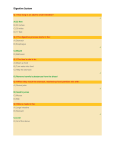
VT 106 Comparative Anatomy and Physiology Digestive System digestive anatomy and physiology depend on diet herbivores – plant-eaters carnivores – meat-eaters omnivores – eat diverse diets animal must be able to digest (chemically break down) its diet depends on enzymes available to catalyze reactions monogastrics – simple stomach produce most of their own digestive enzymes ruminants & hindgut fermenters have fermentation chambers where microbes produce enzymes to digest plant materials DIVISIONS OF THE DIGESTIVE SYSTEM Gastrointestinal (GI) Tract – path that food follows mouth, pharynx, esophagus, stomach, small intestine, large intestine, rectum, anus Accessory Digestive Structures tongue, teeth, salivary glands liver, gallbladder, pancreas FUNCTIONS OF THE DIGESTIVE SYSTEM 1) prehension – grasping food to ingest it 2) mechanical digestion – grinding food into smaller particles and mixing it mastication – chewing rumination – regurgitating and rechewing food GI motility – smooth muscle contractions churning, segmentation – mix food with digestive secretions peristalsis – propels food from esophagus to anus 3) chemical digestion (catabolism) – chemically breaking down food into molecules that can be absorbed (digestive enzymes) 4) absorption – passage of nutrients from GI tract into the blood 5) elimination of wastes excretion – secretion of cellular wastes into GI tract defecation – elimination of feces excreted wastes, undigested or unabsorbed materials 1 ABDOMINAL (PERITONEAL) CAVITY – contains most of GI tract parietal peritoneum – lines walls visceral peritoneum – lines organs peritoneal cavity – space between parietal and visceral peritonea serous fluid lubricates surfaces ascites – fluid accumulation in peritoneal cavity peritonitis – inflammation of peritoneum GENERAL HISTOLOGY OF THE GI TRACT 4 Main Layers: 1) Mucosa – inner epithelial lining stratified squamous epithelium – protects from abrasion mouth, pharynx, esophagus, anus simple columnar epithelium – secretes and absorbs stomach, small and large intestines MALT (mucosa-associated lymphatic tissue) – immune protection 2) Submucosa – connective tissue contains various digestive glands and many capillaries to absorb nutrients 3) Muscularis smooth muscle in most regions skeletal muscle – mouth, pharynx, upper esophagus, anal sphincter voluntary control of swallowing and defecation 4) Serosa – outer visceral peritoneum MOUTH (ORAL OR BUCCAL CAVITY) oral mucosa – stratified squamous epithelium Functions of Mouth: Prehension – grasping and manipulating food lips – skeletal muscle and sensitive tactile receptors in many herbivores tongue – skeletal muscle anchored to hyoid apparatus papillae with tactile and taste receptors Chemical Digestion salivary glands – secrete saliva lubricates food and begins chemical digestion mucus lubricates food and GI tract digestive enzymes – minor function amylase – digests starch (omnivores) lipase – digests fats (nursing animals) bicarbonate ions – large volumes of basic saliva in ruminants neutralize acids in the rumen parotid glands – base of ear submandibular glands – between mandibles sublingual glands – base of tongue 2 ANS Regulation of Salivation parasympathetic n.s. – stimulates salivation stimulated by taste, feel, smell, sight, or thought of food sympathetic n.s. – inhibits salivation Mastication (chewing) – mechanically breaks down food and mixes it with saliva forms a bolus (ball of food) for swallowing increases surface area for digestive enzyme function TEETH maxillae – upper arcade mandible – lower arcade periodontal ligaments – dense fibrous CT that anchors tooth in alveolus gingiva (gums) – oral mucosa lining alveolar processes Regions of a Tooth crown – visible portion above gumline neck – region where gingiva attaches root – portion embedded in alveolus occlusal surface – surface where upper and lower arcade make contact Layers of a Tooth pulp – central connective tissue w/blood vessels and nerves apex – root tip where vessels and nerves enter tooth dentin – main component of tooth harder than bone – 70% calcium salts enamel – outer lining of crown only hardest substance in body – 95% calcium salts protects tooth from abrasion and acids DENTAL FORMULA 4 Types of Teeth: 1) incisors – front teeth chisel-shaped for cutting food 2) canines pointed for grasping and tearing food 3) premolars broader, flatter occlusal surface to crush and grind food 4) molars – back teeth broad, flat occlusal surface to crush and grind food deciduous teeth – baby teeth lost and replaced by adult teeth permanent teeth – adult teeth 3 basic dental formula 3143 seen in some omnivores (eg. pig) 3143 carnivore teeth are more pointed to grasp and tear prey herbivore teeth are flatter to grind fibrous plant material grow continuously to compensate for excessive wear ruminants dental pad (thick connective tissue pad) replaces upper incisors and canines PHARYNX – conducts food and liquid from mouth to esophagus bolus of food or liquid is pushed into pharynx by tongue swallowing reflex – integrated in swallowing center (medulla) larynx elevated – epiglottis closes glottis pharyngeal muscles contract – push bolus into esophagus ESOPHAGUS – muscular tube from pharynx to stomach lies dorsal to trachea and passes through diaphragm mucosa – stratified squamous epithelium (abrasion) peristalsis – coordinated contraction and relaxation of circular and longitudinal muscularis moves bolus from pharynx to stomach regulated by swallowing center and local reflexes lower (gastro)esophageal sphincter – remains closed until bolus arrives prevents gastroesophageal reflux (acid from stomach damages esophagus) horses and rabbits – one-way valve; almost impossible to vomit regurgitation – food comes back up from esophagus or forestomach MONOGASTRIC STOMACH – simple stomach roughly J-shaped greater curvature – large outer curvature lesser curvature – small inner curvature rugae – folds in mucosa mucosa – simple columnar epithelium gastric glands – deep glands beneath mucosa 3 layers of muscularis FUNCTIONS OF STOMACH storage of food – stretches to accommodate food churning – mechanically breaks down food and mixes with secretions chyme – soupy mixture of food and secretions gastric motility – regulated by hormones and ANS 4 secretion of gastric juice hydrochloric acid (HCl) denatures proteins – breaks down food tissues activates digestive enzymes (eg. pepsinogen) kills bacteria in food (stimulated by gastrin, parasympathetic n.s., histamine) digestive enzymes pepsin (active form or pepsinogen) – digests proteins mucus – protects mucosa of stomach from HCl ulcers – erosions of mucosa prostaglandins – help protect stomach from acid NSAIDs can cause ulcers regulatory secretions intrinsic factor – needed to absorb vit. B12 gastrin – hormone released as stomach fills stimulates HCl secretion REGIONS OF STOMACH 1) cardia – attached to esophagus 2) fundus – sac-like region next to cardia stretches to store large meals; has many gastric glands 3) body – muscular central portion churns food; has many gastric glands 4) antrum – connects to small intestine pylorus – sphincter that regulates chyme entering small intestine antrum secretes gastrin Regulation of Gastric Activity 1) cephalic phase (head) – taste, smell, sight, thought of food parasympathetic stimulation of gastric functions 2) gastric phase – food entering stomach stretch reflexes and gastrin stimulate gastric functions 3) intestinal phase – chyme entering intestine stretch reflexes and intestinal hormones inhibit gastric functions SMALL INTESTINE – site of chemical digestion and absorption FUNCTIONS OF SMALL INTESTINE motility – regulated by strretch reflexes, hormones, and ANS segmentation – mixing contractions of circular muscles peristalsis – slow waves move contents from stomach to large intestine hypermotility – contents move too rapidly less absorption causes diarrhea hypomotility (ileus) – contents move too slowly bacterial growth – bloat, sepsis (bacteria in blood) 5 chemical digestion mucus – alkaline to buffer HCl from stomach digestive enzymes intestinal (brush border) enzymes – attached to mucosa pancreatic enzymes – pancreas secretes into duodenum amylase – digests starch sucrase, maltase, lactase – digest disaccharides trypsin, chymotrypsin, peptidases – digest proteins lipases – digest fats (lipids) bile – liver secretes into duodenum emulsifies fats – breaks up lipid droplets so they can be digested by lipases regulatory secretions – hormones secreted as chyme enters duodenum coordinate activities of stomach, intestines, liver, and pancreas secretin – inhibits gastric function stimulates liver and pancreatic secretions cholecystokinin (CCK) – inhibits gastric functions stimulates gallbladder secretions and intestinal motility absorption nutrient molecules pass through mucosa into blood or lymph villi and microvilli increase surface area for absorption Substances Absorbed in Small Intestine into blood capillaries monosaccharides (carbohydrates) amino acids (proteins) electrolytes (ions) water-soluble vitamins water into lymphatic capillaries micelles – small lipid droplets surrounded by bile salts dissolve lipids in intestinal lumen and transport them to mucosa to be absorbed fatty acids, monoglycerides (lipids) lipid-soluble vitamins ANATOMY OF SMALL INTESTINE duodenum – short, proximal region attached to stomach bile duct and pancreatic duct empty into intestine here jejunum – longest, middle region ileum – short, distal region attached to large intestine ileocecal valve – opening into colon large intestine regulated by a smooth muscle sphincter 6 mucosa – simple columnar epithelium w/goblet cells villi – finger-like extensions of mucosa increase surface area for absorption lacteals – large lymphatic capillaries in villi microvilli – finger-like extensions of epithelial cell membrane brush border (fuzzy appearance) – increases surface area Peyer’s patches – MALT LARGE INTESTINE FUNCTIONS OF LARGE INTESTINE motility haustral churning – haustra (pouches) fill, churn contents, pass contents to the next haustra peristalsis – moves contents from ileum to anus chemical digestion bacterial flora (resident bacteria) perform minor digestive functions produce vitamins K and B absorption water, vitamins (K and B), bile salts stores feces ANATOMY OF THE LARGE INTESTINE mucosa – simple columnar epithelium many goblet cells – mucus lubricates feces cecum – variable-sized blind pouch at proximal end contains microbes for hindgut fermentation colon – highly variable in size and appearance rectum – distal end; expands to store feces anus – exit for digestive tract (defecation) internal anal sphincter – involuntary (smooth muscle) external anal sphincter – voluntary (skeletal muscle) mucosa – stratified squamous epithelium REGULATION OF LARGE INTESTINE gastrocolic reflex – stretch of stomach and duodenum triggers increased peristalsis defecation reflex – triggered by stretch receptors in wall of rectum parasympathetic relaxation of internal anal sphincter conscious component – feces in anal canal causes urge to defecate voluntary control of external anal sphincter contraction of abdominal muscles aids defecation 7 PANCREAS endocrine function – pancreatic islets regulate blood glucose level exocrine function – secretes pancreatic juice into small intestine sodium bicarbonate – neutralizes HCl from stomach pancreatic enzymes proenzymes – inactive until activated in intestine ANATOMY OF PANCREAS located in mesentery between stomach and duodenum pancreatic duct – carries pancreatic juice to duodenum REGULATION OF EXOCRINE PANCREAS cephalic phase of gastric stimulation parasympathetic n.s. stimulates secretions chyme entering duodenum secretin – stimulates secretions LIVER hepatic portal system carries venous blood with absorbed nutrients from GI tract to liver for processing before it enters the general circulation liver regulates composition of the blood FUNCTIONS OF LIVER carbohydrate metabolism – maintains blood glucose level glycogenesis – glucose stored as glycogen glycogenolysis – glycogen broken down to release glucose gluconeogenesis – amino acids, lactic acid, other nutrients converted to glucose synthesizes most plasma proteins albumin, alpha and beta globulins, fibrinogen, prothrombin removal or inactivation of many toxins in blood detoxification – breaks down may drugs and toxins eg. converts toxic ammonia to urea excretes or stores other drugs and toxins (eg. antibiotics, pesticides) eg. excretes bilirubin – from old blood cells storage vitamins (A,B12,D,E,K) minerals (iron, copper) phagocytosis and antigen presentation macrophages remove old blood cells, debris, pathogens synthesis and secretion of bile 8 COMPOSITION OF BILE bicarbonate ions – neutralize acid from stomach bile salts – lipids derived from cholesterol amphipathic – have charged and uncharged regions emulsification – break large lipid droplets into tiny micelles lipid droplets coated by a layer of bile salts aids in lipid digestion and absorption bile pigments – from bilirubin; give bile its color Regulation of Bile Secretion parasympathetic n.s. stimulates bile secretion chyme in duodenum CCK – stimulates contraction of gall bladder ANATOMY OF LIVER AND GALL BLADDER largest gland of body hepatic lobes – variable divisions of liver gallbladder – pear-shaped sac near liver stores bile produced by liver (no gallbladder in horses) common bile duct – empties bile into duodenum HISTOLOGY OF LIVER lobules – functional units of liver central vein – drains into hepatic vein triads at each corner of lobule branch of hepatic artery – brings O2 and hormones to lobule branch of hepatic portal vein – brings GI nutrients to lobule bile duct – drains bile produced in lobule hepatic sinusoids – large capillary spaces connecting central vein to blood vessels of triad contain macrophages – phagocytosis and present antigens hepatocytes – liver cells lining sinusoids adjust content of blood produce bile bile canaliculi – ducts which collect bile from hepatocytes drain into bile ducts 9 RUMINANT DIGESTION – have forestomach that acts as a microbial fermentation chamber to provide additional nutrition 4 Stomach Compartments: 1) reticulum – 1st chamber heavy objects swallowed droop into reticulum hardware disease – sharp metallic objects can penetrate wall of reticulum, diaphragm, and pericardium of heart 2) rumen – 2nd chamber; fills most of left abdominal cavity fermentation chamber – normal bacteria and protozoans mixed with large volumes of basic saliva and ingested plant material microbe enzymes digest cellulose (plant carbohydrate) form volatile fatty acids (VFAs) VFAs are absorbed by rumen and reticulum and converted to glucose or lipids by ruminant microbes use ingested proteins and urea from liver to grow and multiply (ruminant digests microbes as a protein source) microbes also synthesize vitamins K and B rumination – contractions of rumen and reticulum regurgitate fibrous plant material (cud) to be rechewed eructation – fermentation produces gases which are expelled (burps) borborygmi – regular “gut sounds” due to normal motility bloat – excess gas production, obstruction, reduced motility 3) omasum – 3rd chamber muscular chamber with many inner folds (leaves) mechanically breaks down food particles, absorbs water and bicarbonate 4) abomasum – 4th chamber; “true stomach” similar to monogastric stomach young ruminants – function as monogastrics small, nonfunctional rumen and reticulum nursing stimulates reflex folding of wall of reticulum reticular groove – funnels milk directly to omasum reflex stops in weeks to months as young begins grazing HINDGUT FERMENTERS – large cecum and colon act as fermentation chambers horse – cecum and large colon (dorsal and ventral colon) cellulose and urea nourish microbial colonies VFAs absorbed by cecum and large and small colons (bicarbonate secreted into colon to neutralize acids) other hindgut fermenters rabbit, pig, guinea pig, rat, (ruminants) 10 11