* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Alteration in the global and regional strains of heart in patients with
Cardiac contractility modulation wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Drug-eluting stent wikipedia , lookup
Coronary artery disease wikipedia , lookup
Remote ischemic conditioning wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
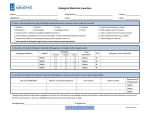
Alteration in the global and regional strains of heart in patients with inferior acute myocardial infarction before and after percutaneous coronary intervention Running head: Myocardial strains in heart infarction 1 Abstract Objectives: To investigate the alteration on regional and global strains of left (LV) and right ventricle (RV) in patients with inferior acute myocardial infarction (AMI) before and after percutaneous coronary intervention (PCI). Methods: From June 2008 to October 2011, forty-four patients with inferior AMI and fifty healthy controls were admitted to Renmin Hospital of Wuhan University in China. Echocardiographic recordings were obtained before and seven days after PCI. Regional and global strains were measured from three deformations including radial, longitudinal and circumferential using specking tracking techniques. Results: Three types of LV global strains were significantly lower in patients than in controls, and LV global longitudinal and circumferential strains were moderately improved by PCI. LV regional longitudinal strains progressively reduced from base toward apex, and were significantly improved in the apical and middle segments by PCI. LV regional radial and circumferential strains gradually diminished from remote through adjacent to infarct myocardium, and were significantly improved in infarct and adjacent myocardium by PCI. The RV global longitudinal strains were significantly lower in patients than in controls, and were moderately improved by PCI. Conclusions: The regional longitudinal strains of LV and RV progressively reduced from base toward apex, and the regional circumferential and radial strains of LV gradually diminished from remote through adjacent to infarct myocardium. PCI mostly improve regional strains of the infarct and adjacent myocardium in the apical and middle levels. 2 Keywords: Strain; acute inferior myocardial infarction; echocardiography; percutaneous coronary intervention 3 Introduction Reliable assessment of regional or overall heart contractility is critical for the diagnosis of disease, evaluation of therapeutic interventions, and prediction of clinical outcomes in the field of myocardial ischemia and infarction. Although computed tomography and magnetic resonance imaging are valuable and feasible diagnostic alternatives, echocardiography remains advantageous for widespread clinical utilization because of its portability, low risk, and comparatively high temporal resolution. Currently, most echocardiography laboratories contribute to use the visual assessment of wall thickening or wall motion score index for everyday clinical use; nonetheless, it is known that subjective visualization and semi-quantitative scores are hampered by substantial observer variability.1 To circumvent these limitations, myocardial velocity imaging and strain imaging have been proposed as objective and quantitative measurement of wall motion abnormalities.2,3 The superiority of strain analysis over myocardial velocity measurement is that strain imaging is not influenced from neighbouring tissue effects and the rotation motion of heart.4,5 Myocardial strain by Doppler echocardiography has been validated to be a powerful method for quantifying regional myocardial with sonomicrometry6 and magnetic resonance imaging.7,8 Regional myocardial strain can be measured by velocity gradient from tissue Doppler imaging (TDI). However, TDI is Doppler angle dependent, which makes the acquisition and correct interpretation of the data more difficult. Furthermore, the clinical use of strain measured by TDI is limited to experienced users due to the low signal-to-noise ratio. Recently, improved hardware and software have allowed angle-independent quantification of myocardial strain based on speckle tracking (ST) technique in two-dimensional B-mode 4 echocardiography. Strain measured using ST method has been shown to identify the presence, location and transmural extent of myocardial infarction,9,10 predict the clinical outcomes and left ventricle remodelling following myocardial infarction (MI).11,12 Left ventricle (LV) contractility is the critical determinant for determining myocardial damage after MI and predicting functional recovery following percutaneous coronary intervention (PCI). ST imaging-derived strains might more accurately reflect intrinsic measures of myocardial contractility and enable quantification of LV regional myocardial deformation by three principal types of deformation: longitudinal, radial and circumferential. Right ventricle (RV) function is an important prognostic factor for clinical outcomes in patients with acute MI of LV. Moreover, RV involvement occurs in a percentage of patients suffering an inferior acute MI and increases in-hospital death rates.13,14 The objective of the present study was to quantify regional or global deformation of LV and RV in patients with acute inferior MI before and after percutaneous coronary intervention (PCI). Additionally, these data was compared with corresponding functional parameters in age-matched control participants. Materials and methods Study population From June 2008 to October 2011, sixty-two consecutive patients were admitted to our hospital for acute inferior MI. The diagnosis of MI relied on characteristic chest pain, electrocardiographic changes, and diagnostic changes in cardiac enzymes. Inferior MI was defined as squeezing chest pain lasting for more than 30 minutes, ST segment elevation ≥ 1 5 mm in inferior leads (leads Ⅱ, Ⅲ and aVF), and a significant rise in serum-specific cardiac enzymes. Eight patients were excluded from the following reasons: two for the history of MI, two for pulmonary hypertension (>30mmHg), one for concurrent severe RV MI, and three for the poor acoustic window. The forty-four of the remaining fifty-four patients underwent emergency PCI within the first twelve hours of symptom onset and were finally enrolled in the study. Fifty age-matched adults, with no cardiovascular pathology and with normal echocardiogram finding, were also enrolled and served as controls. Baseline clinical characteristics of patients and control subjects are summarized in Table 1. The study was approved by the ethics committee of the hospital and all participants gave written informed consent. Echocardiographic data acquisition Thoracic echocardiography was performed with the patients in the left lateral decubitus position before PCI in the angiography laboratory and seven days after PCI in the wards. The echocardiographic evaluation was performed using the Vivid E9 commercial ultrasound scanner (version BT11; GE Vingmed Ultrasound AS, Horten, Norway) and 2.5-MHz transducer. All echocardiographic finding were performed by another physician blinded to the electrocardiographic finding. Conventional echocardiographic measurements were performed according to the recommendations of the American Society of Echocardiography.15 After standard echocardiographic examination, parasternal long-axis, parasternal short-axis, apical four-, three-, and two-chamber views were obtained in end-expiration to minimize translational movement of the heart. All data were acquired at a high frame rate of 70-80 6 frames. At least three cardiac cycles were digitally stored for offline analyses. RV end-systolic and end-diastolic diameters (RVESD and RVEDD) were determined in the four-chamber view from the maximal medium to lateral dimension at mid-cavity. LV endsystolic and end-diastolic diameters (LVESD and LVEDD) were measured in the parasternal long-axis view. LV ejection fraction (LVEF) was assessed using apical two- and fourchamber views with the modified Simpson rule. Strain measurement by speckle tracking model The high frame rate acoustic capture gray-scale images were analyzed offline using a special software program (EchoPac 6.4 Vingmed, Horten, Norway). This software provides an angle-independent tool for evaluation of velocities and strain, and allows for automatic evaluation of the dynamic properties of the endocardial border and of the sub-endocardial tissue from 2-dimensional B-mode echocardiographic clips. The endocardial border was initially manually drawn by the operator during end-systole. From the tracked contour of the endocardium, angle-independent strains were measured by comparing the displacement of the speckles in relation to one another along the endocardial contour through the cardiac cycle. Apical four, three and two-chamber views were analyzed for measurements of longitudinal function, while parasternal short-axis views were analyzed for evaluation of radial and circumferential function. The apical long-axis images were then longitudinally divided into apical sections. At the apical, mid and basal levels, parasternal short-axis images were divided into six segments of equal size: anteroseptal, anterior, anterolateral, inferolateral, inferior, and inferoseptal. Peak strain curves were then computed automatically 7 by tracking the motion of acoustic objects frame-by-frame. Regional strains were obtained from each of the RV or LV divided segments. A composite regional strain value for each patient was derived from the mean values of involved segmental strains. Strain and strain rate were analyzed by another physician blinded to electrocardiographic findings. Statistical analyses Statistical analyses were performed with the SPSS 13.0 software (SPSS Science, Chicago, IL, USA). All data are expressed as mean ± standard deviated (SD). Demographic and echocardiographic variables between patients and controls were compared using unpaired Student’s t test. For continuous variables within groups, a paired t-test was used. A two-tailed P value < 0.05 was considered to be statistically significant. Results Clinical characteristics The baseline clinical features of the study population are summarized in Table 1. Patients and control subjects were similar in age, weight, height, and body mass index (BMI). There were equal ratios of cardiovascular risk factors including hypertension, diabetes mellitus, hyperlipemia and smoking between patients and control subjects. The mean duration of chest pain in the patient group was 220.2 ± 113.2 minutes, mean concentration of cardiac Troponin I was 1.2 ± 0.1ng/ml, and the mean door-to-needle time was 120 ± 63.2 minutes. Forty patients (90%) had primary stent implantation and four patients (10%) received balloon angioplasty procedure in combination with stent implantation. No re-occlusion, ischemic 8 coronary events, or in-hospital deaths occurred during the study period. Conventional echocardiographic data The conventional echocardiographic parameters are summarized in Table 2. LVESD and LVEDD were significantly greater in patients with acute inferior MI than in controls. There were the significant decreases on LVESD and LVEDD in patients at seven days after PCI. Inferior acute MI was associated with decreased EF, nonetheless, EF recovered to closenormal ranges after the PCI. These suggests that inferior acute MI deteriorates the LV function, and PCI promotes the recovery of LV function. RVESD and RVEDD did not differ between controls and patients with inferior acute MI. Moreover, there were similar RVESD and RVEDD between before and after PCI. These indicate that inferior acute MI appears not to cause the enlargement of the RV. Left ventricle global peak strain Figure 1 shows the LV global peak systolic strain in controls and patients before and after PCI. Figure 2 exhibits the representative LV global strain imaging in controls and patients before and after PCI. LV global radial, longitudinal and circumferential strains were less in patients than in controls. LV global radial strain did not differ between after and before PCI. However, LV global longitudinal and circumferential strains were greater in patients after PCI than before PCI. These indicate that PCI improves LV global longitudinal and circumferential strains, which were responsible the recovery of LV contractile function after PCI. 9 Left ventricle regional longitudinal peak strain The regional longitudinal peak strains of LV are summarized in Table 3. All LV regional longitudinal strains were categorized into apical, mid and basal levels. The longitudinal strain values and representative longitudinal strain imaging are illustrated in the upper and lower panels of Figure 3. LV apical, mid and basal longitudinal strains were significantly less in patients with inferior acute MI than in controls. LV basal longitudinal strain did not differ before and after PCI, nonetheless, LV apical and mid longitudinal strains were significantly greater after PCI than before PCI. More importantly, LV regional longitudinal strains progressively reduced from basal toward apical level in patients with inferior acute MI. These suggest that inferior acute MI resultes in the progressive reduction of LV longitudinal strains from base toward apex, and that PCI preliminarily improves longitudinal strains in the apical and mid levels of LV. Left ventricle regional radial peak strain The regional radial peak strains of the LV are summarized in Table 4. All LV regional radial strains were categorized into the six sections consisting of anterior, anterolateral, inferolateral, inferior, inferoseptal and anteroseptal walls. The radial strains and representative radial strain imaging are illustrated in the upper and lower panels of Figure 4. Except for the anterior section, the LV radial strains of remaining five sections were significantly less in patients with inferior AMI than in controls. LV radial strains of anterior section became smaller after PCI than before PCI, nonetheless, LV radial strains of three sections (inferior, inferoseptal, inferolateral) were significantly greater after PCI than before 10 PCI. More importantly, LV radial strains gradually diminished from remote through adjacent to infarct myocardium. These indicate that inferior acute MI resultes in the gradual reduction of LV radial strains from remote through adjacent to infarct myocardium, and that PCI preliminarily improves radial strains in the infarct and adjacent myocardium. Left ventricle regionall circumferential peak strains The regional circumferential peak strains of LV are summarized in Table 5. All LV regional circumferential strains are categorized into the six sections consisting of anterior, anterolateral, inferolateral, inferior, inferoseptal and anteroseptal walls. The circumferential strains and representative circumferential strain imaging are illustrated in the upper and lower panel of Figure 5. Except for the anterior section, the LV circumferential strains of remaining five sections were significantly less in patients with inferior acute MI than in controls. LV circumferential strains of anterior section were smaller after PCI than before PCI; nonetheless, LV circumferential strains of three sections were significantly greater after PCI than before PCI. More importantly, LV circumferential strains gradually diminished from remote through adjacent to infarct myocardium. These indicate that inferior acute MI resultes in the progressive reduction of LV circumferential strains from remote through adjacent to infarct myocardium, and that PCI preliminarily improves circumferential strains in the infarct and adjacent myocardium. Right ventricle global longitudinal peak strain Figure 6 shows the RV global longitudinal strain in controls and patients before and after 11 PCI. Figure 7 exhibits the representative RV global longitudinal strain imaging in controls and patients before and after PCI. Patients with inferior acute MI exhibited a decreased RV global longitudinal strain as compared with controls. However, RV global longitudinal strain was significantly greater after PCI than before PCI. These indicate that inferior acute MI adversely influences the RV function, which is improved by PCI. Right ventricle regional longitudinal peak strain The regional longitudinal peak strains of the RV are summarized in Table 6. All RV regional longitudinal strains are categorized into apical, mid and basal levels. The longitudinal strains and representative longitudinal strain imaging are illustrated in the upper and lower panels of Figure 8. RV apical, mid and basal longitudinal strains were significantly less in patients with inferior acute MI than in controls. RV basal longitudinal strain did not differ before and after PCI, nonetheless, LV apical and mid longitudinal strains were significantly greater after PCI than before PCI. More importantly, LV longitudinal strains progressively reduced from base toward apex in patients with inferior acute MI. These suggest that inferior AMI adversely influences the RV longitudinal strains with their progressive reduction from basis toward apex, and that PCI preliminarily improves the apical and mid longitudinal strains. Discussion Speckle-tracking (ST) derived 2-dimensional strain imaging is a novel echocardiographic technique for the objective assessment of myocardial systolic function. Standard grey scale 12 images are analysed with a dedicated software package that focuses on specific spackles (natural acoustic markers) and tracks them from frame to frame during a cardiac cycle. The motion pattern of myocardial tissue was reflected by the motion pattern of speckles. The ST technique tracks in two dimensions, along the direction of wall, not along the ultrasound beam, and thus is angle independent. Different from velocity and displacement measurement, strain analysis allows discrimination between active and passive myocardial tissue movement. By tracking these speckles, strain can be calculated and reveals the dimensional changes (deformation) as a percentage.16 Shortening or contraction is reflected as a negative value and lengthening or relaxation is reflected as a positive value. Strain values have been reported to be superior to myocardial velocities in the assessment of segmental dysfunction severity after acute MI.17,18 This study utilizes this novel method to investigate the alteration on regional and global LV and RV deformation in patients suffering from inferior AMI before and after PCI. Age-matched healthy subjects were used as controls. In principle, myocardial strains are independent of translational motion and other through-plane motion effects and should be relatively uniform throughout the normal LV myocardium. In this study, we found that regional longitudinal systolic strains progressively decreased from base toward apex along the long axis of LV, and that peak radial and circumferential systolic strains gradually diminished from remore through adjacent into infarct myocardium along the short axis of LV. Moreover, peak systolic strains were uniformly distributed in the nonischemic remote segments. The MI is characterized by the interrupted homogeneous distribution of LV peak systolic strain, which has been proven by other investigations. Sun et al19 found that the homogenous distribution of systolic strain from 13 apical to basal segments was lost during myocardial ischemia and infarction. Ingul et al 20 found that a clear gradient of systolic deformation strain from mid-infarct through the infarct and border zone to normal myocardium. Global strain reflects the averaged segmental myocardial relative shortening and is suggestive of high sensitivity and specificity in the detection of LV systolic dysfunction in patient post-MI.21 As a result, this study also found that LV global strains were significantly decreased in comparison with the control group, and markedly increased after PCI. These findings are consistent with previous reports. Sun et al19 demonstrated that both radial and circumferential strains were decreased significantly in ischemic regions as a result of myocardial ischemia and infarction. Kukulski et al22 found that a significant reduction in strain rate and strain occurred in “at-risk” segments during severe acute ishchemia by epicardial artery occlusion and that these indices recovered to near baseline values immediately after balloon deflation. Ingul et al12 demonstrated that in patients with AMI treated by PCI the global strain indices were improved significantly within two days. Bach et al23 demonstrated that myocardial velocities decreased during acute ischemia and showed a rebound increase after reperfusion in regions supplied from culprit coronary artery. The present study also found that the improved regional strains after PCI was most located in the infract and adjacent myocardium especially in the apical and middle segments of LV. The PCI-resulted reperfusion improves the impaired regional systolic strain, which may be attributed to the salvage of irreversible ischemia myocardium and functional recovery of stunned myocardium.20 As an organic system, all parts of the heart harmoniously to produce an effective cardiac output. Under the conditions of reperfusion, the damaged myocardium acquires activation and contraction, leading to the improvement of LV global 14 function. Longitudinal strain and strain rate imaging have been reported to be well suitable for functional assessment of the complex anatomy and thin wall structure of the RV.24,25 To the best of our knowledge, there are no previous studies assessing RV functions in the patients with inferior AMI by use of ST 2-dimensional strain imaging. This study is the first one assessing strain properties of RV in patients with inferior AMI. Our study found that longitudinal systolic strains were significantly decreased in the apical and mid segments of RV in patients with inferior AMI. The heterogeneous segmental impairment is in accordance with previous investigations. Oguzhan et al26 indicated that the systolic velocities of middle segments of RV were decreased in patients with RV infarction. Sevimli et al27 found that tissue velocity values were progressively decreased from the base toward the apex in inferior AMI without RV infarction. The observation that RV segments presented with significantly impaired systolic strain values than those seen in healthy subjects has several possible pathophysiologic explanations including concomitant therapy with beta-blockers, different afterload of RV compared with normal ventricle, and perfusion abnormalities at the microcirculatory level associated with LV myocardial ischemia. In conclusion, speckle tracking 2D strain imaging allows for the comprehensive and reliable assessment of myocardial contractility and therapeutic efficacy of intervention. Homogeneous distribution of regional strains is lost as a result of ischemic events. The regional longitudinal systolic strains of LV and RV progressively decrease from base to apex; and regional circumferential and radial strains gradually diminish from infarct through adjacent to remote myocardium. Reperfusion by PCI resultes in significant recovery of LV 15 and RV global strains, which are mainly located in the infarct and adjacent myocardium of apical and middle segments. Conflicts of Interest and Source of Funding None. 16 Reference 1. Hoffmann R, Marwick TH, Poldermans D, Lethen H, Ciani R, van der Meer P, Tries HP, Gianfagna P, Fioretti P, Bax JJ, Katz MA, Erbel R, Hanrath P. Refinements in stress echocardiographic techniques improve inter-institutional agreement in interpretation of dobutamine stress echocardiograms. Eur Heart J 2002; 23: 821-829. 2. Sengupta PP, Mohan JC, Pandian NG. Tissue Doppler echocardiography: principles and applications. Indian Heart J 2002; 54: 368-378. 3. Sutherland GR, Di Salvo G, Claus P, D'hooge J, Bijnens B. Strain and strain rate imaging: a new clinical approach to quantifying regional myocardial function. J Am Soc Echocardiogr 2004; 17: 788-802. 4. Luo J, Konofagou EE. High-frame rate, full-view myocardial elastography with automated contour tracking in murine left ventricles in vivo. IEEE Trans Ultrason Ferroelectr Freq Control 2008; 55: 240-248. 5. Kowalski M, Herregods MC, Herbots L, Weidemann F, Simmons L, Strotmann J, Dommke C, D'hooge J, Claus P, Bijnens B, Hatle L, Sutherland GR. The feasibility of ultrasonic regional strain and strain rate imaging in quantifying dobutamine stress echocardiography. Eur J Echocardiogr 2003; 4: 81-91. 6. Urheim S, Rabben SI, Skulstad H, Lyseggen E, Ihlen H, Smiseth OA. Regional myocardial work by strain Doppler echocardiography and LV pressure: a new method for quantifying myocardial function. Am J Physiol Heart Circ Physiol 2005; 288: H23752380. 7. Edvardsen T, Urheim S, Skulstad H, Steine K, Ihlen H, Smiseth OA. Quantification of left 17 ventricular systolic function by tissue Doppler echocardiography: added value of measuring pre- and postejection velocities in ischemic myocardium. Circulation 2002; 105: 2071-2077. 8. Herbots L, Maes F, D'hooge J, Claus P, Dymarkowski S, Mertens P, Mortelmans L, Bijnens B, Bogaert J, Rademakers FE, Sutherland GR. Quantifying myocardial deformation throughout the cardiac cycle: a comparison of ultrasound strain rate, greyscale M-mode and magnetic resonance imaging. Ultrasound Med Biol 2004; 30: 591598. 9. Jurcut R, Pappas CJ, Masci PG, Herbots L, Szulik M, Bogaert J, Van de Werf F, Desmet W, Rademakers F, Voigt JU, D'hooge J. Detection of regional myocardial dysfunction in patients with acute myocardial infarction using velocity vector imaging. J Am Soc Echocardiogr 2008; 21: 879-886. 10. Thibault H, Gomez L, Donal E, Augeul L, Scherrer-Crosbie M, Ovize M, Derumeaux G. Regional myocardial function after myocardial infarction in mice: a follow-up study by strain rate imaging. J Am Soc Echocardiogr 2009; 22: 198-205. 11. Hung CL, Verma A, Uno H, Shin SH, Bourgoun M, Hassanein AH, McMurray JJ, Velazquez EJ, Kober L, Pfeffer MA, Solomon SD; VALIANT investigators. Longitudinal and circumferential strain rate, left ventricular remodeling, and prognosis after myocardial infarction. J Am Coll Cardiol 2010; 56: 1812-1822. 12. Ingul CB, Malm S, Refsdal E, Hegbom K, Amundsen BH, Støylen A. Recovery of function after acute myocardial infarction evaluated by tissue Doppler strain and strain rate. J Am Soc Echocardiogr 2010; 23: 432-438. 18 13. Pereira AC, Franken RA, Sprovieri SR, Golin V. Impact on hospital mortality and morbidity of right ventricular involvement among patients with acute left ventricular infarction. Sao Paulo Med J 2006; 124: 186-191. 14. Turhan H, Yilmaz MB, Yetkin E, Atak R, Biyikoglu SF, Senen K, Ileri M, Cehreli S, Korkmaz S, Kutuk E. Diagnostic value of aVL derivation for right ventricular involvement in patients with acute inferior myocardial infarction. Ann Noninvasive Electrocardiol 2003; 8: 185-188. 15. Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I, et al. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 1989; 2: 358-367. 16. Dandel M, Lehmkuhl H, Knosalla C, Suramelashvili N, Hetzer R. Strain and strain rate imaging by echocardiography - basic concepts and clinical applicability. Curr Cardiol Rev 2009; 5: 133-148. 17. Jamal F, Kukulski T, Sutherland GR, Weidemann F, D'hooge J, Bijnens B, Derumeaux G. Can changes in systolic longitudinal deformation quantify regional myocardial function after an acute infarction? An ultrasonic strain rate and strain study. J Am Soc Echocardiogr 2002; 15: 723-730. 18. Ohara Y, Hiasa Y, Hosokawa S, Miyazaki S, Ogura R, Miyajima H, Yuba K, Suzuki N, Takahashi T, Kishi K, Ohtani R. Usefulness of ultrasonic strain measurements to predict regional wall motion recovery in patients with acute myocardial infarction after 19 percutaneous coronary intervention. Am J Cardiol 2007; 99: 754-759. 19. Sun JP, Niu J, Chou D, Chuang HH, Wang K, Drinko J, Borowski A, Stewart WJ, Thomas JD. Alterations of regional myocardial function in a swine model of myocardial infarction assessed by echocardiographic 2-dimensional strain imaging. J Am Soc Echocardiogr 2007; 20: 498-504. 20 Ingul CB, Stoylen A, Slordahl SA. Recovery of stunned myocardium in acute myocardial infarction quantified by strain rate imaging: a clinical study. J Am Soc Echocardiogr 2005; 18: 401-410. 21 Reisner SA, Lysyansky P, Agmon Y, Mutlak D, Lessick J, Friedman Z. Global longitudinal strain: a novel index of left ventricular systolic function. J Am Soc Echocardiogr 2004; 17: 630-633. 22. Kukulski T, Jamal F, D'Hooge J, Bijnens B, De Scheerder I, Sutherland GR. Acute changes in systolic and diastolic events during clinical coronary angioplasty: a comparison of regional velocity, strain rate, and strain measurement. J Am Soc Echocardiogr 2002; 15: 1-12. 23. Bach DS, Armstrong WF, Donovan CL, Muller DW. Quantitative Doppler tissue imaging for assessment of regional myocardial velocities during transient ischemia and reperfusion. Am Heart J 1996; 132: 721-725. 24. Jamal F, Bergerot C, Argaud L, Loufouat J, Ovize M. Longitudinal strain quantitates regional right ventricular contractile function. Am J Physiol Heart Circ Physiol 2003; 285: H2842-2847. 25. Jategaonkar SR, Scholtz W, Butz T, Bogunovic N, Faber L, Horstkotte D. Two20 dimensional strain and strain rate imaging of the right ventricle in adult patients before and after percutaneous closure of atrial septal defects. Eur J Echocardiogr 2009; 10: 499-502. 26. Oguzhan A, Abaci A, Eryol NK, Topsakal R, Seyfeli E. Colour tissue Doppler echocardiographic evaluation of right ventricular function in patients with right ventricular infarction. Cardiology 2003; 100: 41-46. 27. Sevimli S, Gundogdu F, Aksakal E, Arslan S, Tas H, Islamoglu Y, Buyukkaya E, Gurlertop HY, Senocak H. Right ventricular strain and strain rate properties in patients with right ventricular myocardial infarction. Echocardiography 2007; 24: 732-738. 21 Figure Legends Figure 1. LV global strain in controls and patients with inferior acute MI after and before PCI. Inferior acute MI was associated with substantial reduction of global radial (a), longitudinal (b) and circumferential strains (c). Only global longitudinal (b) and circumferential (c) strains were significantly greater after PCI than before PCI. Figure 2. Representative LV regional strain curves in controls and patients with inferior acute MI before and after PCI. The LV regional strains were significantly lower in patients than in controls; and regional strain curves showed important dyssynchrony and dyssynergy in patients with inferior AMI. Moreover, there were increased LV regional longitudinal and circumferential strains; and there was a relevant improvement in the synchrony and synergy of regional strains revealed by the more uniform amplitude in patients with inferior AMI after PCI. Figure 3. LV longitudinal strains measured in three levels of LV and representative LV longitudinal strain curves obtained from apical two-chamber view in patients with inferior acute MI before and after PCI. The LV longitudinal strains were progressively decreased from base toward apex (a, b). Moreover, the LV longitudinal strains were significantly improved in apical and middle segments after PCI (c, d). #P < 0.05 versus Pre-PCI. Figure 4. LV radial strains measured in six segments of LV and representative LV radial 22 strain curves obtained from parasternal short-axis view in patients with inferior AMI before and after PCI. The LV radial strains were progressively diminished from remote through adjacent to infarct myocardium (a, b). Moreover, the LV radial strains were significantly improved in infarct and adjacent myocardium after PCI (c, d). #P < 0.05 versus Pre-PCI. Figure 5. LV circumferential strains measured in six segments of LV and representative LV circumferential strain curves obtained from parasternal short-axis view in patients with inferior AMI before and after PCI. The LV circumferential strains were progressively diminished from remote through adjacent to infarct myocardium (a, b). Moreover, the LV circumferential strains were significantly improved in infarct and adjacent myocardium after PCI (c, d). #P < 0.05 versus Pre-PCI. Figure 6. RV global longitudinal strain in controls and patients with inferior AMI after and before PCI. Inferior AMI was associated with significantly decreased global longitudinal strains. Global longitudinal strains were significantly greater after PCI than before PCI. Figure 7. Representative RV regional longitudinal strain curves in controls and patients with inferior AMI before and after PCI. The RV regional longitudinal strains were significantly lower in patients than in controls; and regional strain curves showed important dyssynchrony and dyssynergy in patients with inferior AMI. Moreover, there were increased RV regional longitudinal strains after PCI. 23 Figure 8. RV longitudinal strains measured in three levels of LV and representative RV longitudinal strain curves obtained from apical four-chamber view in patients with inferior AMI before and after PCI. The RV longitudinal strains were progressively decreased from base through mid toward apex (a, b). Moreover, the RV longitudinal strains were significantly improved in apical and middle segments after PCI (c, d). #P < 0.05 versus Pre-PCI. 24 Table 1. Baseline clinical characteristics of patients and control subjects. Variables Patients (n = 44) Controls (n = 50) Age, years 60 ± 9 62± 8 Gender, Male/female 28/16 28/22 Height, cm 165 ± 9.7 164 ± 9.5 Weight, kg 68 ± 9 62 ± 8.0 BMI 24.7 ± 2.6 22.8 ± 2.5 Hypertension, n (%) 13(31.8%) 7(14.0%) Diabetes mellitus, n (%) 5(11.3%) 2(4.0%) Hyperlipemia, n (%) 6(13.6%) 2(4.0%) Smoking, n (%) 9(20.4%) 8(16.0%) 25 Table2. Conventional echocardiographic data before and after PCI in inferior AMI patients. Controls Pre-PCI Post-PCI LVESD, mm 34.5 ± 3.4 41.3 ± 3.8* 38.2 ± 3.3# LVEDD, mm 45.4 ± 3.2 53.4 ± 2.4* 50.2 ± 2.5# LVEF (%) 58 ± 3 51 ± 8* 55 ± 3# RVESD, mm 11.9 ± 1.5 12.2 ± 0.9 12.3 ± 0.5 RVEDD, mm 19.5 ± 1.2 21.0 ± 1.3 20.3 ± 0.9 PCI, percutaneous coronary intervention; AMI, acute myocardial infarction; LVESD, left ventricle end-systolic diameter; LVEDD, left ventricle end-diastolic diameter; LVEF, left ventricle ejection fraction; RVESD, right ventricle end-systolic diameter; RVEDD, right ventricle end-diastolic diameter. * P < 0.05 versus Controls. # P < 0.05 versus Pre-PCI. 26 Table 3. Left ventricle longitudinal peak systolic strains obtain in the apical, mid and basal levels before and after PCI in inferior AMI patients. Strain, % Control Pre-PCI Post-PCI Apical - 22.60 ± 4.14 - 10.29 ± 3.58* - 16.47 ± 3.46*# Mid - 22.87 ± 3.63 - 14.62 ± 3.11* - 17.45 ± 4.78*# Basal - 21.06 ± 2.01 - 17.73 ± 3.88* - 19.61 ± 4.31* PCI, percutaneous coronary intervention; AMI, acute myocardial infarction. * P < 0.05 versus Control. # P < 0.05 versus Pre-PCI. 27 Table 4. Left ventricle radial peak systolic strains obtained from the six segments of LV before and after PCI in inferior AMI patients. Strain, % Control Pre-PCI Post-PCI Anterior 47.11 ± 3.26 41.82 ± 5.32 36.40 ± 5.87*# Anterolateral 48.09 ± 8.46 35.21 ± 4.46* 33.24 ± 5.79* Inferolateral 47.30 ± 4.13 20.61 ± 6.25* 37.28 ± 5.10*# Inferior 48.41 ± 4.71 15.27 ± 5.80* 42.34 ± 5.26*# Inferoseptal 45.54 ± 7.02 20.96 ± 7.07* 34.55 ± 4.07*# Anteroseptal 46.64 ± 8.17 32.41 ± 6.06* 33.69 ± 5.45* PCI, percutaneous coronary intervention; AMI, acute myocardial infarction. * P < 0.05 versus Control. # P < 0.05 versus Pre-PCI. 28 Table 5. Left ventricle circumferential peak systolic strains obtained from the six segments of LV before and after PCI in inferior AMI patients. Strain, % Control Pre-PCI Post-PCI Anterior - 31.38 ± 7.02 -30.05 ± 5.95 - 20.23 ± 5.79*# Anterolateral - 29.45 ± 5.35 - 24.59 ± 4.46* - 24.96 ± 5.41* Inferolateral - 30.35 ± 6.87 - 11.67 ± 6.01* - 24.50 ± 6.11*# Inferior - 31.69 ± 6.33 - 8.53 ± 4.88* - 29.5 ± 7.13*# Inferoseptal - 31.19 ± 3.73 - 13.78 ± 7.36* - 25.31 ± 7.12*# Anteroseptal - 30.24 ± 5.54 - 21.65 ± 8.74* - 24.94 ± 6.97* PCI, percutaneous coronary intervention; AMI, acute myocardial infarction. * P < 0.05 versus Control. # P < 0.05 versus Pre-PCI. 29 Table 6. Right ventricle longitudinal peak systolic strains measured in apical, mid and basal levels before and after PCI in inferior AMI patients. Strain, % Control Pre-PCI Post-PCI Apical - 22.25 ± 4.75 - 8.15 ± 3.65* - 12.60 ± 3.46*# Mid - 21.05 ± 3.05 - 10.45 ± 3.75* - 16.61 ± 4.85*# Basal - 23.07 ± 4.01 - 18.75 ± 5.18* - 19.45 ± 4.81* 30 31 32