Section 5: Somatoform Disorders
... 2. Loss of interest or pleasure in all or most activities 3. Significant weight loss or gain due to changes in appetite 4. Sleeping more or less than usual 5. Speeding up or slowing down of physical and emotional reactions 6. Fatigue or loss of energy 7. Feelings of worthlessness or unfounded guilt ...
... 2. Loss of interest or pleasure in all or most activities 3. Significant weight loss or gain due to changes in appetite 4. Sleeping more or less than usual 5. Speeding up or slowing down of physical and emotional reactions 6. Fatigue or loss of energy 7. Feelings of worthlessness or unfounded guilt ...
ap abnormal - HopewellPsychology
... mannerisms, and the original one typically denies any awareness of the other(s) ...
... mannerisms, and the original one typically denies any awareness of the other(s) ...
Somatoform Disorders
... • Pain that causes clinically significant distress or impairment in functioning • There may have been clear physical reasons for the pain initially, but psychological factors play a major role in maintaining it. • The pain is real & it hurts regardless of the cause • Whatever its cause, the pain has ...
... • Pain that causes clinically significant distress or impairment in functioning • There may have been clear physical reasons for the pain initially, but psychological factors play a major role in maintaining it. • The pain is real & it hurts regardless of the cause • Whatever its cause, the pain has ...
Psy 3604
... 1. Be able to describe the essential features of all of the mood disorders, including Major Depressive Disorder, Dysthymia, Bipolar I and II Disorder, and Cyclothymia. 2. Be able to identify and describe the main features of the 6 specifiers of a mood episode. 3. Identify the main features of the 3 ...
... 1. Be able to describe the essential features of all of the mood disorders, including Major Depressive Disorder, Dysthymia, Bipolar I and II Disorder, and Cyclothymia. 2. Be able to identify and describe the main features of the 6 specifiers of a mood episode. 3. Identify the main features of the 3 ...
West Mifflin Area High School Stand Up to Stigma
... have a mental illness or substance use disorder by educating myself and others about these disorders. • I will not ridicule those with a mental illnesses or substance use disorder. • I will not use stigmatizing language like “psycho”, “mental”, “schizo” to refer to anyone whether that person has an ...
... have a mental illness or substance use disorder by educating myself and others about these disorders. • I will not ridicule those with a mental illnesses or substance use disorder. • I will not use stigmatizing language like “psycho”, “mental”, “schizo” to refer to anyone whether that person has an ...
Introduction to Pharmacology
... Both lead to employee loss of time at work Sleep disturbance can also cause absenteeism Cognitive difficulties, i.e. concentration, memory, decision-making Can be associated with other illnesses (cancer, diabetes, cardiac problems) Side effects from medication ...
... Both lead to employee loss of time at work Sleep disturbance can also cause absenteeism Cognitive difficulties, i.e. concentration, memory, decision-making Can be associated with other illnesses (cancer, diabetes, cardiac problems) Side effects from medication ...
Introduction to Pharmacology
... • Both lead to employee loss of time at work • Sleep disturbance can also cause absenteeism • Cognitive difficulties, i.e. concentration, memory, decision-making • Can be associated with other illnesses (cancer, diabetes, cardiac problems) • Side effects from medication ...
... • Both lead to employee loss of time at work • Sleep disturbance can also cause absenteeism • Cognitive difficulties, i.e. concentration, memory, decision-making • Can be associated with other illnesses (cancer, diabetes, cardiac problems) • Side effects from medication ...
Mood Disorders chapter 13
... • For women 20-30% risk • For men 7-12% risk • Depression often occurs along with other medical and psychiatric illnesses ...
... • For women 20-30% risk • For men 7-12% risk • Depression often occurs along with other medical and psychiatric illnesses ...
Disruptive, Impulse Control, and Conduct Disorders
... is what type of aggressive outbursts should be considered: DSM-IV-TR required physical aggression, whereas in DSM-5 verbal aggression and nondestructive/noninjurious physical aggression also meet criteria. An important departure from past diagnostic manuals is that the substancerelated and addictive ...
... is what type of aggressive outbursts should be considered: DSM-IV-TR required physical aggression, whereas in DSM-5 verbal aggression and nondestructive/noninjurious physical aggression also meet criteria. An important departure from past diagnostic manuals is that the substancerelated and addictive ...
Affective Disorders
... Lifetime prevalence: 10-20% Mean age of onset: 27 M:F – 1:2 4th leading cause of disease burden ...
... Lifetime prevalence: 10-20% Mean age of onset: 27 M:F – 1:2 4th leading cause of disease burden ...
Dissociative Disorders
... (aka Functional neurological symptom disorder) • A person experiences very specific physical symptoms for which no physical basis can be found. • blindness • paralysis • Inability to swallow ...
... (aka Functional neurological symptom disorder) • A person experiences very specific physical symptoms for which no physical basis can be found. • blindness • paralysis • Inability to swallow ...
The Use Of Medication In Autism
... • Obsession - recurrent or persistent idea, impulse or image that is intrusive and recognized as being inappropriate • Compulsion - repetitive behavior based on rules and with a stereotypic pattern performed to suppress or diminish dysphoria related to obsession • Occur for more than 1 hour daily an ...
... • Obsession - recurrent or persistent idea, impulse or image that is intrusive and recognized as being inappropriate • Compulsion - repetitive behavior based on rules and with a stereotypic pattern performed to suppress or diminish dysphoria related to obsession • Occur for more than 1 hour daily an ...
Hypochondrias - Cloudfront.net
... People that have had a physical or sexual abuse are more likely to have this disorder. (This doesn't mean people that has this disorder have been sexual or physically abuse). ...
... People that have had a physical or sexual abuse are more likely to have this disorder. (This doesn't mean people that has this disorder have been sexual or physically abuse). ...
"Chronic non-malignant pain - Psychological Interventions
... Types of psycho-somatic disorder • Somatic Symptom Disorder (psychological distress presenting with physical symptoms) • Illness Anxiety Disorder (hypochondria) • Conversion Disorder (now 100% neurological) • Psychological Factors Affecting Other Medical ...
... Types of psycho-somatic disorder • Somatic Symptom Disorder (psychological distress presenting with physical symptoms) • Illness Anxiety Disorder (hypochondria) • Conversion Disorder (now 100% neurological) • Psychological Factors Affecting Other Medical ...
Mood Disorders
... Must have 5 of the following nine symptoms for 2 weeks: Depressed mood most of the day, nearly every day. Little interest or pleasure in almost all activities. Significant changes in weight or appetite. Sleeping more or less than usual. Agitated or decreased level or activity. Fatigue ...
... Must have 5 of the following nine symptoms for 2 weeks: Depressed mood most of the day, nearly every day. Little interest or pleasure in almost all activities. Significant changes in weight or appetite. Sleeping more or less than usual. Agitated or decreased level or activity. Fatigue ...
Memory
... Somatoform and Dissociative Disorders Chapter 14, Lecture 4 “It is little comfort to be told that the problem is ‘all in your head.’ Although the symptoms may be psychological in origin, they are nevertheless genuinely felt.” - David Myers ...
... Somatoform and Dissociative Disorders Chapter 14, Lecture 4 “It is little comfort to be told that the problem is ‘all in your head.’ Although the symptoms may be psychological in origin, they are nevertheless genuinely felt.” - David Myers ...
Chapter12 - J. Randall Price, Ph.D.
... • Humane treatment based on rest, contemplation, and simple work. • Became overcrowded warehouses ...
... • Humane treatment based on rest, contemplation, and simple work. • Became overcrowded warehouses ...
Treatments for Mental Illness
... • mania that does not improve with medications • schizophrenia when symptoms are severe or medications aren’t enough ...
... • mania that does not improve with medications • schizophrenia when symptoms are severe or medications aren’t enough ...
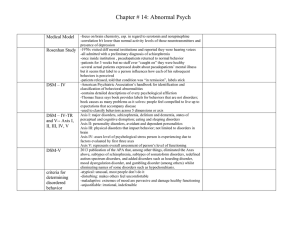
Notes_14 abnormal - Biloxi Public Schools
... -focus on brain chemistry, esp. in regard to serotonin and norepinephine -correlation b/t lower than normal activity levels of those neurotransmitters and presence of depression -1970s visited diff mental institutions and reported they were hearing voices -all admitted with a preliminary diagnosis o ...
... -focus on brain chemistry, esp. in regard to serotonin and norepinephine -correlation b/t lower than normal activity levels of those neurotransmitters and presence of depression -1970s visited diff mental institutions and reported they were hearing voices -all admitted with a preliminary diagnosis o ...
Jason Bernard Christopher Rodriguez Christian Lopez
... Theories of Causes: Inherited tendencies, or genes and child abuse. People with antisocial or alcoholic parents are at increased risk. ...
... Theories of Causes: Inherited tendencies, or genes and child abuse. People with antisocial or alcoholic parents are at increased risk. ...
Chapter 14 Powerpoint
... No real external source Occurs most days in a 6 month period Worry excessively about money, health, friends, family May occur with Depression ...
... No real external source Occurs most days in a 6 month period Worry excessively about money, health, friends, family May occur with Depression ...
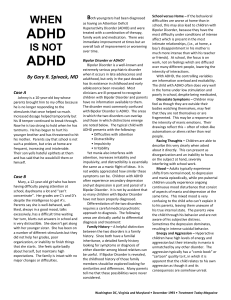
ADHD vs. Mood Disorders - Columbia Associates in Psychiatry
... not widely appreciated how similar these symptoms can be. Children with ADHD often experience secondary depression and yet depression is part and parcel of a Bipolar Disorder. It is not by accident that so many children with Bipolar Disorder have not been properly diagnosed. Differentiation of the t ...
... not widely appreciated how similar these symptoms can be. Children with ADHD often experience secondary depression and yet depression is part and parcel of a Bipolar Disorder. It is not by accident that so many children with Bipolar Disorder have not been properly diagnosed. Differentiation of the t ...
Lifespan Development
... may be disconnected and illogical. Peculiar behaviors may be associated with social withdrawal and disinterest. Diagnostic criteria for Schizophrenia (cautionary statement) A. Characteristic symptoms: Two (or more) of the following, each present for a significant portion of time during a 1-month ...
... may be disconnected and illogical. Peculiar behaviors may be associated with social withdrawal and disinterest. Diagnostic criteria for Schizophrenia (cautionary statement) A. Characteristic symptoms: Two (or more) of the following, each present for a significant portion of time during a 1-month ...
Schizoaffective disorder

Schizoaffective disorder (abbreviated as SZA or SAD) is a mental disorder characterized by abnormal thought processes and deregulated emotions. The diagnosis is made when the patient has features of both schizophrenia and a mood disorder—either bipolar disorder or depression—but does not strictly meet diagnostic criteria for either alone. The bipolar type is distinguished by symptoms of mania, hypomania, or mixed episode; the depressive type by symptoms of depression only. Common symptoms of the disorder include hallucinations, paranoid delusions, and disorganized speech and thinking. The onset of symptoms usually begins in young adulthood, currently with an uncertain lifetime prevalence because the disorder was redefined, but DSM-IV prevalence estimates were less than 1 percent of the population, in the range of 0.5 to 0.8 percent. Diagnosis is based on observed behavior and the patient's reported experiences.Genetics, neurobiology, early and current environment, behavioral, social, and experiential components appear to be important contributory factors; some recreational and prescription drugs may cause or worsen symptoms. No single isolated organic cause has been found, but extensive evidence exists for abnormalities in the metabolism of tetrahydrobiopterin (BH4), dopamine, and glutamic acid in people with schizophrenia, psychotic mood disorders, and schizoaffective disorder. People with schizoaffective disorder are likely to have co-occurring conditions, including anxiety disorders and substance use disorder. Social problems such as long-term unemployment, poverty and homelessness are common. The average life expectancy of people with the disorder is shorter than those without it, due to increased physical health problems from an absence of health promoting behaviors including a sedentary lifestyle, and a higher suicide rate.The mainstay of current treatment is antipsychotic medication combined with mood stabilizer medication or antidepressant medication, or both. There is growing concern by some researchers that antidepressants may increase psychosis, mania, and long-term mood episode cycling in the disorder. When there is risk to self or others, usually early in treatment, brief hospitalization may be necessary. Psychiatric rehabilitation, psychotherapy, and vocational rehabilitation are very important for recovery of higher psychosocial function. As a group, people with schizoaffective disorder diagnosed using DSM-IV and ICD-10 criteria have a better outcome than people with schizophrenia, but have variable individual psychosocial functional outcomes compared to people with mood disorders, from worse to the same. Outcomes for people with DSM-5 diagnosed schizoaffective disorder depend on data from prospective cohort studies, which haven't been completed yet.In DSM-5 and ICD-9 (which is being revised to ICD-10, to be published in 2015), schizoaffective disorder is in the same diagnostic class as schizophrenia, but not in the same class as mood disorders. The diagnosis was introduced in 1933, and its definition was slightly changed in the DSM-5, published in May 2013, because the DSM-IV schizoaffective disorder definition leads to excessive misdiagnosis. The changes made to the schizoaffective disorder definition were intended to make the DSM-5 diagnosis more consistent (or reliable), and to substantially reduce the use of the diagnosis. Additionally, the DSM-5 schizoaffective disorder diagnosis can no longer be used for first episode psychosis.