Mental Health Nursing: Anxiety Disorders
... A condition characterized by a mood that is elevated, expansive, or irritable Accompanied by hyperactivity, undertaking too many activities, lack of judgment in anticipating consequences, pressured speech, flight of idea, distractibility, inflated self-esteem, or hypersexuality ...
... A condition characterized by a mood that is elevated, expansive, or irritable Accompanied by hyperactivity, undertaking too many activities, lack of judgment in anticipating consequences, pressured speech, flight of idea, distractibility, inflated self-esteem, or hypersexuality ...
Chapter 16: DEVELOPMENTAL PSYCHOPATHOLOGY
... material with toxic protein called beta amyloid • The plaque injures/kills neurons • Neurofibrillary tangles – twisted strands of ...
... material with toxic protein called beta amyloid • The plaque injures/kills neurons • Neurofibrillary tangles – twisted strands of ...
Chapter 25 - Stellenbosch University
... experience is that it is the manic phase in both girls and boys that first brings the child to hospital. The depressive episode, if present, is probably being missed by the family and the school. ...
... experience is that it is the manic phase in both girls and boys that first brings the child to hospital. The depressive episode, if present, is probably being missed by the family and the school. ...
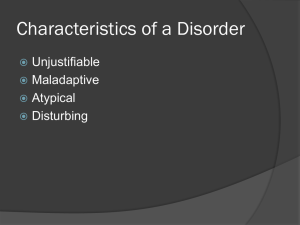
Classification in Psychiatry
... suffering of self or partner, children or non consenting partner. ...
... suffering of self or partner, children or non consenting partner. ...
PSY240H1S Introduction to Abnormal Psychology
... • Females 10 x more likely to develop an eating disorder • Around 5% of young women will develop an eating disorder • Course and outcome of eating disorders is highly variable • Eating disorders are associated with serious complications, and have the highest mortality rate ...
... • Females 10 x more likely to develop an eating disorder • Around 5% of young women will develop an eating disorder • Course and outcome of eating disorders is highly variable • Eating disorders are associated with serious complications, and have the highest mortality rate ...
Open Document
... 4.) Obsessive Compulsive Disorder ◦ Marked by persistent, uncontrollable intrusions of unwanted thoughts (obsessions) and urges to engage in senseless rituals (compulsions) ◦ Some common behaviors ...
... 4.) Obsessive Compulsive Disorder ◦ Marked by persistent, uncontrollable intrusions of unwanted thoughts (obsessions) and urges to engage in senseless rituals (compulsions) ◦ Some common behaviors ...
Schizophrenia-like Disorders - Viktor`s Notes for the Neurosurgery
... 2) psychotic episode (at least 2 weeks duration) without mood symptoms in individual with previously diagnosed mood disorder ← this distinguishes from MOOD DISORDER WITH PSYCHOTIC FEATURES. DSM-IV Diagnostic Criteria for Schizoaffective Disorder A. Uninterrupted period of illness during which there ...
... 2) psychotic episode (at least 2 weeks duration) without mood symptoms in individual with previously diagnosed mood disorder ← this distinguishes from MOOD DISORDER WITH PSYCHOTIC FEATURES. DSM-IV Diagnostic Criteria for Schizoaffective Disorder A. Uninterrupted period of illness during which there ...
Mental Health: Depression
... dysthymia, it is long-term (two years or longer) feelings of depression that are not extremely severe but still prevent a person from normal functions of daily life • Psychotic depression—occurs in conjunction with a form of psychosis, such as hallucinations or delusions • Postpartum depression—can ...
... dysthymia, it is long-term (two years or longer) feelings of depression that are not extremely severe but still prevent a person from normal functions of daily life • Psychotic depression—occurs in conjunction with a form of psychosis, such as hallucinations or delusions • Postpartum depression—can ...
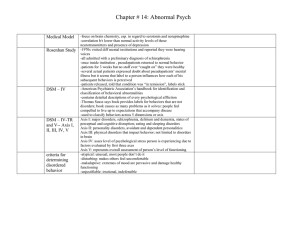
Medical Model - Biloxi Public Schools
... -focus on brain chemistry, esp. in regard to serotonin and norepinephine -correlation b/t lower than normal activity levels of those neurotransmitters and presence of depression -1970s visited diff mental institutions and reported they were hearing voices -all admitted with a preliminary diagnosis o ...
... -focus on brain chemistry, esp. in regard to serotonin and norepinephine -correlation b/t lower than normal activity levels of those neurotransmitters and presence of depression -1970s visited diff mental institutions and reported they were hearing voices -all admitted with a preliminary diagnosis o ...
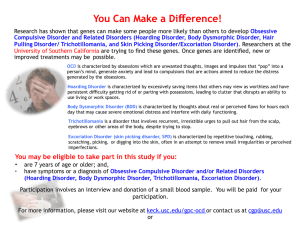
OCDR USC Sites Flyer_20150326_IRB Approved_No Riverside Ofc
... Research has shown that genes can make some people more likely than others to develop Obsessive Compulsive Disorder and Related Disorders (Hoarding Disorder, Body Dysmorphic Disorder, Hair Pulling Disorder/ Trichotillomania, and Skin Picking Disorder/Excoriation Disorder). Researchers at the Univers ...
... Research has shown that genes can make some people more likely than others to develop Obsessive Compulsive Disorder and Related Disorders (Hoarding Disorder, Body Dysmorphic Disorder, Hair Pulling Disorder/ Trichotillomania, and Skin Picking Disorder/Excoriation Disorder). Researchers at the Univers ...
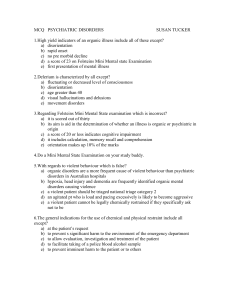
MCQ PSYCHIATRIC DISORDERS
... a) there is a disturbance of cognitive and higher cortical functioning b) consciousness is sometimes clouded but not always c) it is characterized by short term memory loss d) there is also some evidence of global memory impairment e) it is a disease of the elderly 14.Which is incorrect with regard ...
... a) there is a disturbance of cognitive and higher cortical functioning b) consciousness is sometimes clouded but not always c) it is characterized by short term memory loss d) there is also some evidence of global memory impairment e) it is a disease of the elderly 14.Which is incorrect with regard ...
Schizophrenia and Other Psychoses
... • There will be significant psychosocial impairment and/or distress • Symptoms must have begun at least 6 months earlier. ...
... • There will be significant psychosocial impairment and/or distress • Symptoms must have begun at least 6 months earlier. ...
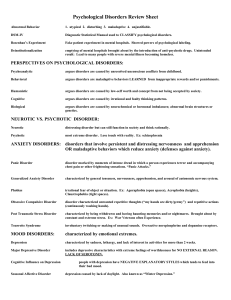
AP_Chapter_16_psychological_disorders[1][1]
... mannerisms, and the original one typically denies any awareness of the other(s) ...
... mannerisms, and the original one typically denies any awareness of the other(s) ...
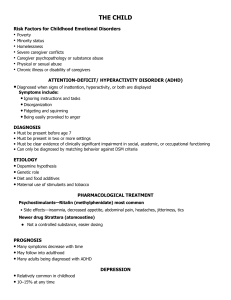
THE CHILD
... • Must be present before age 7 • Must be present in two or more settings • Must be clear evidence of clinically significant impairment in social, academic, or occupational functioning • Can only be diagnosed by matching behavior against DSM criteria ETIOLOGY ...
... • Must be present before age 7 • Must be present in two or more settings • Must be clear evidence of clinically significant impairment in social, academic, or occupational functioning • Can only be diagnosed by matching behavior against DSM criteria ETIOLOGY ...
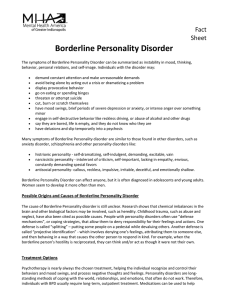
Borderline Personality Disorder
... mechanisms”, or coping strategies, that allow them to deny responsibility for their feelings and actions. One defense is called “splitting” – putting some people on a pedestal while devaluing others. Another defense is called “projective identification” - which involves denying one’s feelings, attri ...
... mechanisms”, or coping strategies, that allow them to deny responsibility for their feelings and actions. One defense is called “splitting” – putting some people on a pedestal while devaluing others. Another defense is called “projective identification” - which involves denying one’s feelings, attri ...
Unit 6
... Bipolar disorder rates are the same for both genders. Married women are more often depressed than single women. The more children a woman has the more likely she is to become depressed. Learned helplessness: a condition is which a person has accepted the generalized idea that she can do nothing to h ...
... Bipolar disorder rates are the same for both genders. Married women are more often depressed than single women. The more children a woman has the more likely she is to become depressed. Learned helplessness: a condition is which a person has accepted the generalized idea that she can do nothing to h ...
Drop the language of disorder Evidence
... with less unusual and distressing mental states. There is no easy ‘cut-off’ between ‘normal’ experience and ‘disorder’. We should also recognise that psychosocial factors such as poverty, unemployment and trauma are the most strongly evidenced causal factors for psychological distress (2) although, ...
... with less unusual and distressing mental states. There is no easy ‘cut-off’ between ‘normal’ experience and ‘disorder’. We should also recognise that psychosocial factors such as poverty, unemployment and trauma are the most strongly evidenced causal factors for psychological distress (2) although, ...
Schizoaffective disorder

Schizoaffective disorder (abbreviated as SZA or SAD) is a mental disorder characterized by abnormal thought processes and deregulated emotions. The diagnosis is made when the patient has features of both schizophrenia and a mood disorder—either bipolar disorder or depression—but does not strictly meet diagnostic criteria for either alone. The bipolar type is distinguished by symptoms of mania, hypomania, or mixed episode; the depressive type by symptoms of depression only. Common symptoms of the disorder include hallucinations, paranoid delusions, and disorganized speech and thinking. The onset of symptoms usually begins in young adulthood, currently with an uncertain lifetime prevalence because the disorder was redefined, but DSM-IV prevalence estimates were less than 1 percent of the population, in the range of 0.5 to 0.8 percent. Diagnosis is based on observed behavior and the patient's reported experiences.Genetics, neurobiology, early and current environment, behavioral, social, and experiential components appear to be important contributory factors; some recreational and prescription drugs may cause or worsen symptoms. No single isolated organic cause has been found, but extensive evidence exists for abnormalities in the metabolism of tetrahydrobiopterin (BH4), dopamine, and glutamic acid in people with schizophrenia, psychotic mood disorders, and schizoaffective disorder. People with schizoaffective disorder are likely to have co-occurring conditions, including anxiety disorders and substance use disorder. Social problems such as long-term unemployment, poverty and homelessness are common. The average life expectancy of people with the disorder is shorter than those without it, due to increased physical health problems from an absence of health promoting behaviors including a sedentary lifestyle, and a higher suicide rate.The mainstay of current treatment is antipsychotic medication combined with mood stabilizer medication or antidepressant medication, or both. There is growing concern by some researchers that antidepressants may increase psychosis, mania, and long-term mood episode cycling in the disorder. When there is risk to self or others, usually early in treatment, brief hospitalization may be necessary. Psychiatric rehabilitation, psychotherapy, and vocational rehabilitation are very important for recovery of higher psychosocial function. As a group, people with schizoaffective disorder diagnosed using DSM-IV and ICD-10 criteria have a better outcome than people with schizophrenia, but have variable individual psychosocial functional outcomes compared to people with mood disorders, from worse to the same. Outcomes for people with DSM-5 diagnosed schizoaffective disorder depend on data from prospective cohort studies, which haven't been completed yet.In DSM-5 and ICD-9 (which is being revised to ICD-10, to be published in 2015), schizoaffective disorder is in the same diagnostic class as schizophrenia, but not in the same class as mood disorders. The diagnosis was introduced in 1933, and its definition was slightly changed in the DSM-5, published in May 2013, because the DSM-IV schizoaffective disorder definition leads to excessive misdiagnosis. The changes made to the schizoaffective disorder definition were intended to make the DSM-5 diagnosis more consistent (or reliable), and to substantially reduce the use of the diagnosis. Additionally, the DSM-5 schizoaffective disorder diagnosis can no longer be used for first episode psychosis.






![AP_Chapter_16_psychological_disorders[1][1]](http://s1.studyres.com/store/data/008609904_1-bcd0b4691952c52f8b5635246f54a50a-300x300.png)