* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Outline20 Cardio2 - Napa Valley College
Management of acute coronary syndrome wikipedia , lookup
Coronary artery disease wikipedia , lookup
Cardiothoracic surgery wikipedia , lookup
Cardiac contractility modulation wikipedia , lookup
Heart failure wikipedia , lookup
Artificial heart valve wikipedia , lookup
Cardiac surgery wikipedia , lookup
Electrocardiography wikipedia , lookup
Myocardial infarction wikipedia , lookup
Hypertrophic cardiomyopathy wikipedia , lookup
Mitral insufficiency wikipedia , lookup
Jatene procedure wikipedia , lookup
Heart arrhythmia wikipedia , lookup
Ventricular fibrillation wikipedia , lookup
Quantium Medical Cardiac Output wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
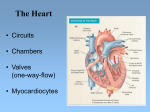
Biology 219 – Human Physiology Clemens Cardiovascular System 2 – Cardiac Function Text: Ch. 14 A. Cardiac Cycle systole - contraction phase (ventricular systole ~1/3 of cycle) diastole - relaxation phase (ventricular diastole ~2/3 of cycle) 5 specific phases of cardiac cycle (1) ventricular filling (mid to late diastole): low P in ventricle AV valves open, semilunar valves closed ventricular volume ↑ (2) atrial systole (end of ventricular diastole): atrial contraction “tops off” ventricles after passive phase of ventricular filling (3) isovolumic contraction (beginning of ventricular systole) P↑↑ rapidly as ventricles contract AV valves close → 1st heart sound (“LUB”) semilunar valves still closed, so volume stays constant as P increases (4) ventricular ejection: (mid to late systole): P↑ to maximal semilunar valves open blood ejected to arteries and ventricular volume ↓ (5) isovolumic relaxation (beginning of diastole) P↓↓ rapidly semilunar valves close → 2nd heart sound (“DUP”) AV valves stay closed until ventricular P < atrial P - Pressure in LV ranges from ~ 0 during diastole to 120 mm Hg at peak of systole. - Arterial BP in aorta & large arteries ranges from 80 (diastolic) to 120 mm Hg (systolic). BP is sustained in diastole by closure of semilunar valves and elastic recoil of arteries. - Volume in ventricles is highest at end of diastole, lowest at end of systole. Wiggers cardiac output diagram (refer to textbook) correlates: - electrical events (ECG) - pressure changes in atria, ventricles, and aorta, volume and heart - volume changes in ventricles - heart sounds B. Cardiac Output = total blood flow per minute from one ventricle; RV and LV have the same output cardiac output (CO) = heart rate (HR) X stroke volume (SV) resting: 5,000 mL/min ≈ 72 beats/min X 70 mL/beat - CO is total blood flow to all tissues of the body (systemic circuit); increased demand for O2 and nutrients is accommodated by increase in CO 2. Stroke Volume end-diastolic volume (EDV) – end-systolic volume (ESV) = SV (Resting values: 130 mL 60 mL 70 mL ) Control of Cardiac Output 1. Modulation of Heart Rate a. Autonomic NS sympathetic: sympathetic cardiac nerve (NE) → β1 adrenergic receptors → increased rate of pacemaker depolarization at SA node → increases HR - E & NE secreted by the adrenal medulla also bind to β1 receptors to increase HR parasympathetic: vagus nerve (ACh) → muscarinic receptors → decreases HR at SA node - parasympathetic control dominates at rest (“vagal tone”) Biology 219 – Human Physiology Clemens 2. Modulation of Stroke Volume a. Intrinsic control: Starling’s Law of the Heart increase in EDV → increase in force of contraction → increase in SV - results from the length-tension relationship of cardiac muscle: increased filling stretches sarcomeres to a more optimal part of L-T curve - EDV increases due to increased venous return to the heart b. Extrinsic control sympathetic NS → NE → increase in contractility of the heart adrenal medulla → E & NE Signal transduction pathway: 1. E and NE bind to β1 adrenergic receptors 2. GPCR activates the cAMP second messenger system → phosphorylation of proteins 3. ↑ Ca2+ entry from the ECF and ↑ Ca2+ release from the SR 4. ↑ actin-myosin crossbridge formation → ↑ force & speed of contraction