* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download July 2015 NHS Highland CAMHS Tier 2 CAMHS Referral Requests
Survey
Document related concepts
Abnormal psychology wikipedia , lookup
Clinical mental health counseling wikipedia , lookup
Involuntary commitment internationally wikipedia , lookup
Deinstitutionalisation wikipedia , lookup
Child migration wikipedia , lookup
Psychiatric survivors movement wikipedia , lookup
History of mental disorders wikipedia , lookup
Causes of mental disorders wikipedia , lookup
Child Protective Services wikipedia , lookup
Community mental health service wikipedia , lookup
Transnational child protection wikipedia , lookup
Lifetrack Therapy wikipedia , lookup
Mental health professional wikipedia , lookup
Unaccompanied minor wikipedia , lookup
Transcript
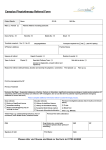
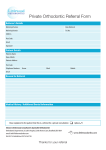
July 2015 NHS Highland CAMHS CAMHS REFERRAL GUIDANCE AND CRITERIA Tier 2 CAMHS Referral Requests for service from the Primary Mental Health Worker Service are considered through consultation. Where focused targeted therapeutic intervention at an early stage is likely to have long term benefit to the well being of the young person and their family. Tier 3 CAMHS Referral If there are concerns regarding a child or young person who might need an urgent mental health assessment (e.g. evidence of early psychosis; risk of suicide with specific plans and preparation i.e. gathering of medication; severe depression; severe eating disorder with significant weight loss over a short period. We would suggest if possible these referrals are discussed with a CAMHS clinician prior to referral submission. Referrals of an urgent nature out with normal working hours and at weekends should be directed to A&E. All other referrals would be considered for routine appointments. Tier 4 CAMHS Referral Young people with mental health difficulties and one or more of; Too high risk to attempt to treat with usual out-patient resources for example suicidal, psychotic with disorganisation, self harm or violent behaviour. Need intensive assessment or treatment (equivalent to more than weekly out-patient contact and more than one CAMHS professional) Not responding to usual out-patient treatment – which may be because they need re-assessment or more intensive input. July 2015 NHS Highland CAMHS CAMHS REFERRAL GUIDANCE Introduction to this Guidance This guidance document is intended to assist those in front line services to know when to refer to NHS Highland CAMHS, as well as offering suggestions for advice or where to go to get more information. The guidance is designed to improve access to CAMHS for those children and young people who need it most, whilst at the same time making sure that other sources of help have been tried where appropriate. Referrals are accepted from GPs, Public Health Nurses, Health Visitors, Paediatricians, Other Hospital Doctors, including Dentists, Allied Health Professionals, Educational Psychologists, Social Workers, Reporters to the Children’s Panel etc NHS Highland CAMHS NHS Highland CAMHS provides specialist assessment as part of a tiered system which includes both stepped care (as a problem becomes more severe in nature the type of help that is available becomes more specialised) and matched care (the idea that there should be an accurate and properly informed match of need to provision at the earliest stage of a child or young person’s presentation). CAMHS 4 Tier Model of service delivery Specialist inpatient & Intensive Community outreach CAMHS operates within the Getting it right for every child principles using a tiered model of intervention that includes the established staged approach which ensures that children receive both a stepped care approach (the idea that as a problem becomes more sever in nature the type of help that is available becomes more specialised) and matched care approach (the idea that there should be an accurate and properly informed match of need to provision at the earliest stage of a child or young person’s presentation). Tier 1: Also referred to as universal level the child’s needs are addressed through normal class room/nursery management/by public mental health nurse, school nurse, health visitor, social worker, children’s service worker. CAMHS has no direct involvement at Tier 1 but remains committed to building capacity and confidence within universal services via training and consultation. Tier 4 Specialist CAMHS Team Tier 2: Also referred to single agency when concerns continue. My World Assessment undertaken and need/risk analysed and detailed within a child’s plan. Other staff may be involved; children may be receiving some specific support i.e. children’s service worker, family social work, health visitor etc. request for service to Tier 2 CAMHS may be accepted at this stage, via consultation. Tier 3 PMHW – Training/consultation to increase capacity & confidence. Consultation & direct work with children & young people Universal services who all have a role to promote Children emotional health consisting of all primary care agencies including GP’s, school nursing, health visitors, children’s service workers and schools Tier 3: Also referred to as single agency where concerns continue but targeted support is requested. Advice, plus recommendations sought perhaps from special educational services (e.g. Educational Psychologists) Children may have Individualised Education Programmes (IEP). At times PMHW’s offer a bridge into specialist CAMHS and could be both involved at this tier. Tier 2 Tier 1 Tier 4: Also referred to as mutli-agency plan or stage 4 interventions. Significant support from one or more agencies is required and the child may require a Co-ordinated support plan (CSP). A small minority if children may enter at this tier if their mental health deteriorates and are likely to receive inpatient care & may also require a multi agency response. Specialist CAMHS are nearly always involved at this stage. July 2015 NHS Highland CAMHS Referrals to NHS Highland CAMHS CAMHS accepts referrals from a variety of sources – some tips as to what makes a good referral can be found here. In deciding how to proceed we will consider whether there is evidence of specific mental health difficulties, whether there is any risk of harm to self or others and also the severity of the symptoms and the degree of impairment. If the CAMHS team assess that the difficulties noted represent mild to moderate mental health issues then the referral is passed to our Tier 2 Primary Mental Health Worker Service, via consultation. Those referrals that describe more severe, complex and enduring mental health difficulties will be seen by our Tier 3 CAMHS service. Child and Adolescent Mental Health Services are focussed on children and young people presenting with severe and complex difficulties whereas the Primary Mental Health Team aims to intervene earlier with the milder to moderate cases. Referrers should note that a multi disciplinary approach will always be taken by the Service with referrals of children who are looked after or looked after away from home. We find it is best to meet with the responsible Social Worker to discuss and plan how best to ensure the child or young person can access our Service. Referrals to our service are considered urgent if there are: a) concerns that a child/young person is suicidal b) concerns that a child/young person has an acute psychosis c) concerns that a child/young person has life-threatening weight loss or BMI of less than 18 Or occasionally when there is reason to believe that there is significant risk to a child that may be alleviated by the CAMHS becoming involved quickly. In these unusual cases we would often aim to discuss the referral personally with the referrer and suggest that you telephone the team and speak to a Clinician. Referrals of an urgent nature out with normal working hours and at weekends should be directed to A&E. All other referrals would be considered for routine appointments. NHS Highland currently provides Child & Adolescent Mental Health Services to children and young people from birth to eighteen years of age if in full time school OR sixteen years of age. For referrals in those children under the age of five years we find it is best to meet with the Health Visitor, Public Health or School Nurse in the first instance. PMHW can provide consultation for this age group. PMHW Service Consultation by the Primary Mental Health Team is the early intervention part of CAMHS. The purpose of consultation is to make information on childrens mental health accessible to all those professionals working with children within Highland. Consultation is accepted from ALL child care professionals including, Guidance Teachers, Head Teachers, Public Health Nurses, Family Support Workers, Social Workers, Voluntary Organisations etc. During consultation the PMHW may accept a direct request for service. The PMHW Service offers a range of treatment options including advice, self-help material, supported self-help, and a range of short-term individual and family based interventions using a stepped care approach. (hyper link to PMHW guidance) July 2015 NHS Highland CAMHS Consultation offers advice, guidance and can provide access to our resources gathered to work with children. It is NOT an emergency or crisis service. Referrals Accepted by Tier 3 CAMHS Referral to the Tier 3 CAMH Service should be by the referral form (link). There is specific information that must be included within the referral to ensure that the correct intervention can be targeted to the right child/young person. If a referrer is not sure what to include, s/he might want to phone the Tier 3 service and discuss the referral. If a referral is accepted we write to the child or young person and their family providing information about the service. If from the referral information it is not clear which intervention would be helpful then an assessment appointment may be offered. The Royal College of Psychiatrists have produced a helpful brochure on what to expect from CAMHS which can be downloaded from http://www.rcpsych.ac.uk/PDF/CAMHS%20inside%20outx.pdf Referral Criteria July 2015 NHS Highland CAMHS Problem Description Referral Pathway Anxiety: anxiety disorders are the most common type of mental health disorder in children Anxiety is a normal and common part of childhood. In most cases, anxiety in children is temporary, and may be triggered by a specific stressful event e.g. young child may experience separation anxiety when starting school. In some cases, anxiety in children can be persistent and intense, interfering with a child’s daily routines and activities. Anxiety disorders include phobias, general anxiety, panic or persistent unexplained physical symptoms, e.g. headache or stomach-ache, where physical cause has been excluded. Children who show persistent or severe symptoms of anxiety should be referred to Tier 3 CAMHS by letter and/or with a Child’s Plan. Schools and education departments have their own resources (e.g. inclusion support workers, educational psychologists and behavioural support services) which should to be exhausted prior to referral. A summary of school / education department involvement and action will be essential before a referral can be accepted therefore we would normally expect a child to be subject to Staged Intervention. CAMHS will not accept referrals for school truancy only and referrers should consult with other Children’s Services and/or the Highland Council Educational Psychology Service in the first instance. Separation Anxiety Disorder/School Refusal Those with less severe difficulties may be directed to the PMHW Service after consultation with the PMHW. You may want to discuss your concern with school first. The Educational Psychologist can refer to CAMHS if required. Schools can also access the PMHW Service for consultation. Advice The Tier 3 service should be involved: Where the child’s development or level of functioning has been seriously affected or there has been a sudden deterioration Where it appears to be out of proportion to the family circumstances Where there is a significant impact on the parent / carer / child relationship-please describe in referral. You may wish to find out more at www.moodjuice.scot.nhs.uk/anxiety www.shapeofmind www.youngminds.org.uk www.anxietyuk.org.uk www.stressandanxietyinteenagers.com www.handsonscotland.co.uk/topics/anxiety/scho ol_refusal.html July 2015 Bereavement: Grief is the normal response to the loss of a loved one. NHS Highland CAMHS Childrens response to grief can be varied, dependent on age, cognition and developmental stage. Quite often it can be the subsequent change in circumstances or other family members’ reactions that can prove difficult for the child. Consult with PMHW in the first instance describing what has been tried and how the difficulties are affecting the childs day to day functioning. The PMHW may work directly with the child/young person or may signpost other services that can provide bereavement support. You may want to consider referral to Tier 3 service when the loss has had an extreme impact on the child and their functioning, or when the child is experiencing difficulties after bereavement support. Learning Disabilities: this is also known as Global Learning Disability normally evident from early childhood and defined as significant impairment of intellectual functioning including impaired social functioning, If the child is experiencing significant distress and / or difficulties following a bereavement / loss that has occurred in extreme circumstances (e.g. trauma, illness, suicide or accident) you may want to refer to Tier 3 CAMHS Learning disability on its own is not CAMHS do not conduct initial diagnostic grounds for referral to Tier 3 CAMHS. For assessments for global learning CAMHS to become involved there have to disability. Paediatricians, Educational be concerns about a mental health Psychologists and pre school special problem in those already identified as teachers assess children for global having a Global Learning Disability and learning disability. associated behavioural or mental health problems. Professionals concerned about a child/young person with ASD can refer to the Highland Framework for This group may also include worries Assessment and Diagnosis of regarding ASD (Autism Spectrum Autism Spectrum Disorders, a multiDisorder) or Aspergers. Difficulties which may impact on daily living and are criteria disciplinary framework agreed by in which could support a referral include: Highland. Significant delay in acquiring Young people aged 18 and over should appropriate social skills be referred to adult learning disability Significant difficulties with the services. child’s peer relationships Although painful for everyone including professionals, you may wish to give the child & family some time to experience a normal grief process You may wish to consider referral to CHAS at Home (the Highland outreach service for the Children’s Hospice Association of Scotland) Where support is provided for children & parents who are bereaved as well as individual work. www.chas.org www.rd4u.org.uk www.winstonswish.org.uk www.childbereavement.org.uk www.cafamily.org.uk Developmental difficulties often come to light when a child gets older i.e. throughout the course of their development. www.incredibleyears,com www.angermgmt.com www.aspergersyndrome.org National Autistic Society offers information and support http://www.autism.org.uk/ July 2015 NHS Highland CAMHS Children and young people with a learning disability can present with any of the mental health problems described in this document but their presentation may be complicated by factors such as communication difficulties and sensory sensitivities ADHD: Attention Deficit Hyperactivity Disorder is characterised by pervasive lack of attention, impulsivity and hyperactivity across situations and settings – at home, school, and in public – which began before 7 years of age. Families with children who display difficulties in these categories should have already received significant advice and intervention from other professionals such as paediatricians, health visitors, social workers and educational support services before referral to CAMHS is made. www.adhdtraining.co.uk/ www.boxofideas.org/ The PMHW Service may offer consultation to those adults supporting the child/young person where their behavioural needs are causing concern. involves both obsessions and compulsions that take a lot of time and get in the way of activities. Obsessions (intrusive repetitive thoughts) Compulsions (repetitive, ritualistic, unwanted actions) These will be either distressing or disabling and interfere with the child’s functioning and across settings e.g. school and home. This behaviour can also be as the result of anxiety or a change. Depression: Low mood is a normal part of childhood Obsessive Compulsive Disorder (OCD): CAMHS would not normally assess a child for ADHD until they have completed at least one term within P1. For children all children the normal route to assessment would through referral to Community Paediatrics. If the outcome is unclear or severe presentation a referral to Tier 3 CAMHS may be considered, Children often experience obsessions and compulsions as part of normal childhood behaviour and they can often disappear without intervention. Therefore when considering specialist referral the situation has to be distressing, disabling and interfere with the childs day to day functioning. If pervasive and evident across settings then a referral to the Tier 3 CAMH Service may be considered. GPs may advise and review prior to This behaviour can often be due to a change therefore establishing normal routines may affect a positive change www.ocdyouth.ipo.kcl.ac.uk Info site run by Royal Maudsley Hospital on OCD www.ocduk.org Includes Information and Guide for parents of young children www.ocduk.org/pdf/children.pdf www.ocduk.org/pdf/youngpeople.pdf : www.ocduk.org/pdf/ParentsOCDGuide.pdf : Information and guide for parents of children worried about OCD For more info: July 2015 NHS Highland CAMHS disturbances of mood, sleeping, irritability, decrease in energy, social isolation, school performance is affected and thoughts of selfharm have been expressed and in most cases is temporary and might well resolve on its own. referral as often difficulties can resolve without intervention. In order for referral to CAMHS to be appropriate difficulties should be more than age appropriate variation of mood. There should be a significant change from previous levels of functioning and an impact on daily living. Where symptoms are mild or moderate in nature, a consultation with a PMHW will help clarify what support may be appropriate and whether they should provide some direct intervention to the child/young person. Bipolar disorder is rare in children and relatively uncommon in adolescents. For persistent and severe symptoms, or if concerns exist regarding suicidal thoughts then refer to Tier 3 CAMHS may be appropriate. Post Traumatic Stress Disorder / Acute stress disorder; due to PTSD is linked with an extreme traumatic stress involving direct personal experience of an event that involves actual or threatened death or serious injury. The event is re-experienced in one or more of the following ways: flashbacks, nightmares related to the event, reenactment through play, intense emotional arousal, numbness around memories and physical symptoms such as tummy aches and headaches. It is important to know whether there are legal proceedings pending and to establish who wishes to establish the severity of the symptoms. For example is someone asking for help or is the main concern a wish to support some legal case exposure to one or more traumatic, often life threatening events www.moodjuice.scot.nhs.uk/depression.asp www.shapeofmind.scot.nhs.uk www.depressioninteenagers.com www,beatingtheblues.co.uk www.breathingspacescotland.co.uk Where children and young people are currently experiencing trauma such as domestic violence a referral to the Family Team is likely to be appropriate. Psychological intervention is unlikely to be possible where the child's living situation continues to be insecure and traumatic. www.cedarfv.org.uk/ Where symptoms are mild or moderate in nature, a consultation with a PMHW will help clarify what support may be appropriate and whether they should provide some direct intervention to the child/young person. For persistent and severe symptoms, referral to Tier 3 CAMHS may be appropriate. Psychosis: Rare in children and adolescents but may involve transient states or short episodes of As manifested in thought disorder, delusions, perceptual disturbances, hallucinations Referral to Tier 3 CAMHS is indicated. If urgent, contact CAMHS within normal working hours. Outside this time contact Accident and Emergency if emergency assessment is required. www.rcpsych.ac.uk/mentalhealthinfo/mentalhealt handgrowingup/psychoticillnessyoungpeople.asp x July 2015 NHS Highland CAMHS delusions, hallucinations, disorganised speech or behaviour Self Harm : overdoses & other serious self harm. This is rare in children under 12 years of age. Deliberate self harm without suicidal intent takes many forms and can be seen as a way of dealing with difficult feelings that build up. Self harm here would have the absence of suicidal intent. If you feel concerned that the self harming behaviour is indicative of a disturbance of emotional and psychological well-being then you should refer to CAMHS. Where symptoms are mild or moderate in nature or appear to be due to a specific and recent incident or event, a consultation with a PMHW will help clarify what support may be appropriate and whether they should provide some direct intervention to the child/young person. Self harm at this level can be very anxiety provoking for professionals. PMHWs are committed to providing training and development opportunities to Tier 1 professionals to assist them to deal with things like self harm. They can provide or signpost towards training in Mental Health Awareness (Scottish Mental Health First Aid for Young People) and suicide prevention (ASSIST). www.selfharm.uk.org www.harmless.org.uk/downloads For persistent and severe symptoms, referral to Tier 3 CAMHS may be appropriate. Eating Disorders Anorexia: is characterised by a refusal to maintain Deliberate self harm with suicidal intent should always be taken seriously. However the decision to attempt suicide is often a hasty one – following arguments with family, friends and partner. Therefore it is important to establish if the intent was to end one’s life. Overdoses and other serious self-harm should be sent directly to A&E in the first instance. The ward or hospital will then refer on to CAMHS. Where there is concern in relation to an eating disorder it is advisable to discuss with GP in the first instance to think about medical investigations (blood, weight, height BMI etc) prior to referral. If there has been a recent rapid weight loss (1kg+ per week with ED cognitions present) with no physical cause, request urgent Tier 3 CAMHS appointment Referrals from hospital will be prioritised & referral protocols are already in place. A follow-up appointment from the Tier 3 service should always be arranged. This is an example of the sort of screening questions that can be helpful however any decision on referral will be based on relevant history and clinical presentation Do you make yourself sick because you feel July 2015 NHS Highland CAMHS uncomfortably full? a minimally normal body weight or an intense fear of gaining weight. Bulimia: is characterised by binge-eating and purging and maintaining adequate body weight. Sometimes the school nurse is also a good source of support in helping to weigh a child you suspect may be of low weight. It is important that a young person has a physical check with their GP or School Nurse. This not only gives us some ideas re BMI but assists with prioritisation as we would want to prioritise those children with low BMI. Feeding and Faltering Growth: this is where growth has been affected by feeding difficulties (also known as non organic failure to thrive) Faltering growth is a common occurrence and health visitors play a key role. Most children with faltering growth will be detected by the primary health care team and supported within the community. Feeding problems include: children with behavioural feeding problems in the context of chronic illness/medical problems; severe and chronic selective eaters; infant feeding problems and failure to thrive; emotional eating difficulties (e.g. food phobias) or in the context of somatic problems such as chronic fatigue syndrome. Consult Health Visitor/Public Health Nurse in the first instance. Refer on to paediatrician as necessary. Enuresis and Encopresis or complex soiling: Initial screening and treatment should be undertaken by paediatrician to rule out physical causes. Refer to paediatrician in the first instance who will then refer to other specialist services if appropriate. Both are categorised as elimination If the symptoms are less severe but there is some concern that a young person has some distorted thinking or body image, consult with PMHW in the first instance. The PMHW may work directly with the child/young person or may signpost other services that can provide support. Do you worry you have lost control over how much you eat? Have you recently lost more than 1 stone in a 3 month period? Do you believe yourself to be Fat when others say you are too thin? Would you say food dominates your life? If the young person answers yes to 2 of these questions consider referral. www.b-eat.co.uk You may wish to look at www.childrenfirst.nhs.uk/families/features/behavi our/fussy_eaters.html Initial screening and treatment should be undertaken by the paediatric team CAMHS referrals often come via this route. The PMHW can offer consultation to Health Visitors/ Public Health Nurses. You may wish to find out more information from www.eric.org.uk which includes a free downloadable toolkit for parents and professionals July 2015 NHS Highland CAMHS disorders and is the inability to control urination or soiling in those deemed old enough to exercise control Psychosomatic Difficulties: children experiencing emotional distress in the form of physical symptoms with no physical illness and also children with real physical illness where the presentation is complicated by mental health difficulties Physical complaints with no apparent medical basis may be a reflection of a stress, such as nervousness in a social situation, a demanding school setting, separation from parents, or other stressful situation. Referral should be considered only when this is having significant impact on the child’s normal functioning e.g. absence from school for long periods Initial referral to a paediatrician is often useful especially where there are unexplained physical symptoms in the absence of obvious mental health difficulties Where a child is experiencing physical symptoms initial referral to a paediatrician is recommended. Where symptoms are mild or moderate in nature a consultation with a PMHW will help clarify what support may be appropriate and whether they should provide some direct intervention to the child/young person. www.there4me.com Website for children and young people (12-16) who have got fears and worries. Run by NSSPCC www.rcpsych.ac.uk/mentalhealthinformation/men talhealthproblems/physicalillness/unexplainedphy sicalsymptoms Royal College of Psychiatrists Website For persistent and severe symptoms, referral to Tier 3 CAMHS may be appropriate. It is therefore useful that children have completed physical investigations prior to referral to rule out any organic cause so that the child and family will accept the idea some psychological cause for the difficulties. Better outcomes can be achieved by preparing the family in this way. Children / young people Looked After or Looked After Children are looked after and looked after away from home for many varied reasons. Their legal situations are also very varied and complex. Referrals to specialist CAHMS are best made by the responsible social worker. PMHWs offer training and consultation to foster parents to support them. LAC and LAAC can present with mental If concerns exist they will have been discussed in July 2015 Away from Home: those known to social services, LAC, LAAC, or families with longstanding problems and a poor history of engagement NHS Highland CAMHS health needs of varying nature. Referrals for children in this category need to identify whether a child or young person has a mental health difficulty or other condition that results in persistent symptoms of psychological distress, as well as an associated serious and persistent impairment of their day to day social functioning. OR, an associated risk that the child/young person may cause serious harm to themselves or others. Where symptoms are mild or moderate in nature a consultation with a PMHW will help clarify what support may be appropriate and whether they should provide some direct intervention to the child/young person. For persistent and severe symptoms, referral to Tier 3 CAMHS may be appropriate. multi agency groups. Local authority and CAMHS aim to work together to provide a common, coordinated framework across all agencies that support the delivery of appropriate, proportionate and timely help to all children as they need it. This includes not subjecting children to multiple assessments or to repeat information that other agencies hold. Therefore it is important that information is shared and accessed e.g. the Integrated Assessment Framework, or Staged Intervention process and Child Protection processes. Given these principles (called GIRFEC) its is important that professionals who are concerned about children utilise their existing referral protocols into our Service rather than suggest to the family that they attend their GP. We would need to know how the child/family is affected by their symptoms i.e. how is their day to day functioning affected. Early Years: Significant emotional or behavioural difficulties 0 – 5 years With this age group it is unusual for CAMHS to directly intervene. The normal referral route being from Health Visitors. Problems within this age range can take many forms : • Parent/child relationship • Factors affecting capacity to parent • Developmental concerns or illness Refer to health visitor or to Paediatrician CAMHS involvement with this age range should be secondary not primary. Consequently, families with young children with development and/or behavioural problems should have already received significant advice and intervention from other named PMHWs are committed to a programme of training and development for Tier 1 professionals and may be involved in direct work to support parents where issues arise eg Video Interaction Guidance. Often with these types of difficulties the relationship between the parent and child is the actual patient; therefore it is useful to know what July 2015 NHS Highland CAMHS Specialist consultation is offered to, SCUB/Paediatricians, Tier 3 to network as part of care planning when accommodated. Dyadic interventions professionals such as paediatricians, health visitors, social workers and educational support services including within Nursery. has already been attempted. Therefore referrals should include information on what has been attempted and who is involved. Inappropriate Referrals to CAMHS In order to improve accessibility for children and young people, we also need to clarify which types of problem it is not appropriate to refer to specialist CAMHS. (a) Children/Young People with Behavioural Difficulties as a Response to Normal Life Events These are sometimes called “normal adjustment reactions”. Unfortunately, we are unable to provide a service to children and young people whose behaviours are associated with a normal reaction to recent life events (e.g. bereavement, parental separation). Although challenging these are often within developmental and cultural norms. Some indication of mental health disorder needs to be evident in the behaviour for a referral to be appropriate. It is also important that CAMHS is a secondary or specialist route of referral when behaviour is being considered as the primary route should always be universal and primary care services who can support families within their own home. (b) Children/Young People Whose Difficulties Occur only at School Please note that specialist CAMHS does not provide a service for children and young people whose problems are solely related to specific learning or behavioural difficulties within the classroom. Schools have their own referral route and protocols for supporting such children. For these children/young people it is usually more appropriate for educational services to become involved to address the difficulties. If a referral to CAMHS is appropriate it is best made through the child’s plan. (c) Children/Young People Whose Parents are in Dispute within Legal Proceedings Children of separated / divorced parents who are in legal dispute about residence and /or contact arrangements or other issues are not specifically excluded in these guidelines though the decision to refer needs to be carefully considered on a case by case basis. If there are ongoing legal proceedings then it is usually better to consider a referral after the legal proceedings have been concluded and legal agreements or Order(s) have been made regarding the matters which are in dispute. Please note that it is for the Courts to order independent reports on the child, not the separate parties to the proceedings, and these reports cannot be obtained via a referral to the specialist child mental health services. Please note that specialist CAMHS does not mediate residence and contact arrangements for the child/young person. The parent(s) could instead be advised to approach the Family Mediation Service or discuss with their solicitor, as appropriate. (d) Children/Young People Whose Primary Difficulty is Substance Misuse July 2015 NHS Highland CAMHS AND (e) Children/Young People Whose Difficulty is Described as Offending Behaviour In both of these circumstances it is important that a coordinated integrated assessment to the child or young persons situation is undertaken. This is the responsibility of the local authority youth action team and or the child forensic psychology service. What Makes a Good Referral It is important that those referring have met with the parent(s)/carer(s) and the referred child/children. It is essential that the referral to CAMH service is made containing the information requested as per referral form. Child and Adolescent Mental Health Service Phoenix Centre Raigmore Hospital Inverness IV2 3UJ