* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download Clinic Laboratory Tests in Cardiac Disease1.82 MB
Survey
Document related concepts
Transcript
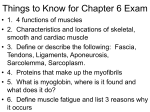
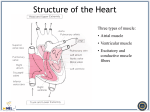
Clinic Laboratory Tests in Cardiac Disease Prof. Dr. ARZU SEVEN Cardiac markers should be: absolutely heart specific highyl sensitive able to differentiate irreversible damage from reversible able to detect reocclusion and reinfarction able to monitor reperfusion therapy able to estimate size of infarct and prognosis stable able to make measurements rapidly easy to perform cost effective Ruling out AMI requires a test with high diagnostic sensitivity. Ruling in AMI requires a test with high specificity. A single test that will quickly and accurately assess AMI (acute myocardial infarction) does not exist. A combination of markers is used : An early marker that increases within 6 hr. after onset of symptoms A definite marker that increases after 6-9 hrs. and remains high for several days Enzymes as Cardiac Markers Creatine kinase (CK or CPK) Aspartate amino transferase (AST) Lactate dehydrogenase (LDH or LD) Creatine Kinase A cytoplasmic and mitochondriac enzyme Total CK is %40 sensitive and %80 specific CK-1(BB) : Brain CK-2(MB) :Myocardium CK-3(MM) :Skeletal muscle ,heart CK-3 has 3 isoforms :CK-31, CK-32 and CK-33 (posttranslational products) CK-2 has 2 isoforms Half life :CK-31 > CK-32>CK-33, CK-21>CK-22 CK-MB (CK-2) has the most specificity for cardiac muscle (>%85) CK-MB (CK-2) accounts for only 3-20 % of total CK activity in heart Normal skeletal muscle contains 1 % CK-2 CK-2 is increased in severe skeletal muscle injury (trauma/surgery ),chronic muscle disease (muscular dystrophy, polymyositis ) and extreme exercise. Reason:Regeneration process of muscle (reexpression of CK-MB genes ) In AMI,CK-MB increases at least 4-6 hr.after onset of chest pain,makes a peak at 12-24 hr. and returns to baseline level in 2-3 days (t 1/2 is 10-12 hr ) Factors that might affect the classic pattern : 1-Size of infarction 2-CK-2 composition in myocardium 3-Concomitant skelatal muscle injury and reperfusion Differentation of increased CK-2 due to heart or muscle monoclonic anti CK-2 antibody based assays %relative index (%RI)= CK-2 activity /total CK X %100 helpful in the detection of AMI CK-22: the predominant isoform in blood collected 2-6 hr. after AMI .It makes a peak ≈10-18 hr.,decreases rapidly 12-24 hr concomitantly as CK-21 gradually increases. Following trombolitic therapy in AMI patients, greater than two fold increases of CK-2 occur within 90 min. of reperfusion The rate of which CK-2 isoform is released from the myocardium to circulation appears to be the more useful index of coronary reperfusion CK22 ∕ CK-21 ratio→best discriminant within 1 hr. after treatment Lactate Dehydrogenase (LDH) A cytoplasmic enzyme found in skeletal, muscle, liver, heart, kidney and red blood cells 5 izoenzymes, composed of 4 subunit peptides of 2 distinct types:M (muscle ), H (heart) LDH isoenzyme determination increases specificity for cardiac tissue. LD1 (HHHH):moves fastest towards anode LD5 (MMMM):moves closest towards cathode LD2 (HHHM ) LD3 (HHMM ) LD4 (HMMM ) LD1 in heart,kidney(cortex), red blood cells LD5 in liver,skeletal muscle In healthy adults: 14-26 % LD1 (slow removal ) 29-39% LD2 20-26% LD3 8-16 % LD4 6-16 % LD5 (rapid disappearance ) Not a tissue specific enzyme In AMI total LD -elevation at 12-18 hr peak at 48-72 hr return to baseline level after 6-10 days LD 1 (heart) elevation at 10-12 hr clinical specificity 85-90 in patients suspected of AMI peak at 72-144 hr return to normal >10 days Total LD patern ≈LD1 pattern (contrast with total CK and CK-2 pattern) Because of its prolonged half life, LD-1 is a clinically sensitive (%90) marker for infarction when measured after 24 hr. LD1∕LD2 >1,0 →FLIPPED PATTERN (clinical sensitivity %75 , clinical specificity 85-90 in patients suspected of AMI) if CK-2 values are diagnostic for AMI, cancel LD isoenzyme test request, because LD isoenzyme results don’t increase the clinical specificity of diagnostic CK-2 results for AMI As with CK-2 in skeletal muscle, the heart specific LD-1 isoenzyme in skeletal muscle can increase twofold during a 9-wk exercise training, with paralel decreases in LD-5 LD and isoenzymes play no role in unstable and stable angina. Aspartate aminotransferase (AST ) Widely distributed in many tissues Highest concentrations are found in cardiac tissue, liver and skeletal muscle. Clinical utility in hepatocellular disorders and skeletal involvement. Unuseful in diagnosis of AMI Beginsto rise within 6-8 hr. Makes a peak at 24 hr. Generally returns to normal within 5 days. Myoglobin O2 binding protein of cardiac and skeletal muscle. Low molecular weight and cytoplasmic location-early appearance in circulation after muscle injury Cleared rapidly by kidney→unreliable as a long term marker of cardiac damage Cardiac muscle trauma, skeletal muscle trauma, Crush injury and AMI cause an increase in myoglobin levels. serum myoglobin methods are unable to distinguish the tissue of origin reference intervals vary according to age, rate and sex 1. age myoglobulin 2. male > female 3. black > white very sensitive early diagnostic marker for AMI (%90-100) ,poor clinical specificity (%60-95) rises as early as 1 hr. after AMI, peaks in 4-12 hr reflects the early course of myocardial necrosis, lasts for 24 hr. the role of myoglobin in the detection of AMI is within 0-4hr. (CK-2 is within its reference level). To improve clinical specificity,carbonic anhydrase III (CAIII) should be measured. After AMI, CK-2 and myoglobin increase,but CA III remains unchanged.In severe skeletal muscle trauma (exercise, shock and i.m injection ), CK-2, myoglobin and CAIII increase. If myoglobin remains unchanged and within reference levels on multiple,early samplings within 3-6 hr. after onset of chest pain,there is 100 %certainty that muscle (either skeletal or cardiac ) injury has NOT occurred recently—Negative predictor Myoglobin/total CK >5 reperfusion indicator (clinical sensitivity 75 %,clinical specificity 96 % ) Cardiac Troponins Contractile proteins found in muscle that play role in actin-myosin interaction Complex of 3 protein subunits : 1. troponin C: calcium binding component 2. troponin I: inhibitory component 3. troponin T:tropomyozin_binding component Subunits exist in many isoforms like CK Distribution of these isoforms varies between cardiac muscle and slow/fast twitch skeletal muscle Only 2 major isoforms of troponin C are found in human heart and skeletal muscle Troponin is located in ; 1. myofibril (%94-97) 2. cytoplasm (%3-6) Cardiac troponin I and T have different amino acid sequences Human cTn I has an additional 3I AA residue compared to skeletal muscle Tn I (cardiac specificity) 11 AA residue gives troponin T unique cardiac specificity Early release kinetics of both cTnI and cTnT are similiar to CK-2 after AMI Elevation at 4-8 hr. Remains elevated at 4-10 days (replaces LD isoenzyme assay in the detection of patients presenting late after AMI) Cardiac specificity of troponin I and T eliminate the false clinical impression of AMI in patients with high CK-2 after skeletal muscle injury Troponin T (cTnT) Clinical sensitivity is similiar to that of CK-2 in the 48 hr. after the onset of pain (%50-65) Rises within a few hrs. after chest pain,peaks by day 2 →Like CK-2, cTnT is insufficient for effective early diagnosis However cTnT remains high for a longer time (up to 7-10 days) giving high clinical sensitivity (>%90) up to 5-7 days after AMI . When AMI patients are grouped separately from other cardiovascular pathologies Clinical specificity for cTnT %40-60 “ “ “ CK-2 %75-80 When AMI patients are grouped with unstable angina and minor myocardial injury specificity for cTnT improves to >%80 Troponin I (cTnI) Comparable to CK-2 for diagnostic sensitivity of AMI in the first 48-72 hr. After 72-96 hr cTnI sensitivity increases Has serial rise and fall kinetics similiar to CK-2 after AMI during 48-72 hr, remains elevated 3-7 days In patients with high CK-2 concentrations due to acute skeletal muscle injury following marathon racing, Duchenne’s muscular dystrophy, chronic renal failure requiring dialysis, cTn I is NOT elevated cTn I should be measured in patients with falsely increased CK-2 values for the detection of cardiac injury cTn I has (+) predictive value (%95) and (-) predictive value (%100) cTnI is successful: in ruling out AMI patients with cocaine induced chest pain in accurately detecting cardiac injury in patients with blunt chest trauma in accurately determining high incidence of cardiac injury in critically ill patients in risk stratification analysis neither cTn I nor cTn T offered advantages over myoglobin in the early (< 2 hr) screening for AMI, both troponins could identify AMI > 6 hr after presentation. elevation of troponin T or I within 6 hr of symptoms increased risk of complication need for intervention increased cTnI in unstable angina predicts a poorer clinical outcome to determine the effects of reperfusion, cTnT should be measured at the time of trombolytic therapy initiation and 90 min. after therapy BNP and NT – pro BNP (Brain natriuretic peptide) To diagnose congestive heart failure To grade the severity of heart failure To differentiate between heart failure and lung disease To monitor the effects of therapy for heart failure NT pro BNP is a marker in the blood for BNP, a hormone that rises during cardiac stress Homocysteine An amino acid Too much homocysteine in the blood is related to a higher risk of coronary heart diseases, stroke and peripheral vascular diseases. Has an effect on atherosclerosis. High levels of homocysteine are the result of lack of certain B Vitms. ,inheritance or dietary excess and have been implicated in vascular wall injury. Testing for plasma homocysteine levels can improve the assessment of risk, particularly in patients with a personal family history of cardiovascular disease. CRP Sensitive marker of acute and chronic inflammation and infection and in such cases is increased several hundred- fold. Useful in predicting the risk for a thrombotic event ( a blood clot causing MI ) Heart patients who have persistant CRP levels between 4-10 mg/dl with clinical evidence of low grade inflammation should be considered to be at increased risk for thrombosis. CRP protein results may be affected by the use of -oral contraceptives -NSAID’s -steroids -salicylates -IUD Homocysteine levels may be affected by -smoking -DM -coffee