* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download EMBRYOLOGY
Embryonic stem cell wikipedia , lookup
Optogenetics wikipedia , lookup
Cell theory wikipedia , lookup
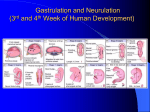
Nerve guidance conduit wikipedia , lookup
Microbial cooperation wikipedia , lookup
Anatomical terms of location wikipedia , lookup
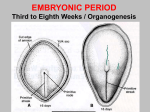
Adoptive cell transfer wikipedia , lookup
Central nervous system wikipedia , lookup
Regeneration in humans wikipedia , lookup
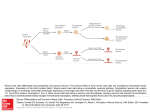
Syllabus This syllabus is designed to provide a schedule for a short course in medical embryology with 18 one-hour lectures. It provides a sample format for organizing such a course that can be modified to fit schedules of longer or shorter duration. Course Description This course provides basic information about critical events in human development. Virtually every physician, regardless of their discipline, will see a woman who is already pregnant or of childbearing age at some time in their career. Therefore, it is extremely important that the physician realize that he or she is treating two people, not one, and that whatever procedures or medications are prescribed may have a serious impact on the unborn child. This course will describe the classical embryologic events, from formation of gametes to birth, that result in a newborn child and the genes that regulate them. It will also focus on clinical problems associated with birth defects and their means of prevention. Textbook Langman's Medical Embryology by T.W. Sadler, 9th ed. Lippincott, Williams and Wilkins, 2004 Additional Teaching Aids The syllabus is designed to focus your studying, especially the sections labeled The Bottom Line. Knowing the material in The Bottom Line will enable you to pass the course. This edition of Langman’s has new information about the molecular regulation of development that covers most of the organ systems. Additional information about genetic regulation of developmental events can be found in Scott Gilbert's textbook of Developmental Biology, 6th ed., Sinauer Assoc. Inc., 2000, and on Dr. Gilbert's website called Developmental Biology (address: www.devbio.com). The Simbryo CD attached to each Langman text provides a three-dimensional interactive video of normal and clinical embryology. 1 Objectives Lecture 1: Gametogenesis (Chapter 1) 1. Explain why the process of mitosis requires one cell division, while meiosis requires two. 2. Describe examples of chromosomal and genetic factors responsible for congenital malformations in humans. Terms to define: ploidy, haploid, diploid, homologous chromosomes, nondisjunction, balanced and unbalanced translocations, mosaicism, spermiogenesis, spermatogenesis The Bottom Line, Chapter 1 Mitosis: replication of cells—each daughter gets same number of chromosomes— homologous chromosomes do not pair. Meiosis: two cell divisions—homologous chromosomes pair and crossover occurs—four full-size spermatids but only one egg result from meiosis. Nondisjunction: if it occurs during mitosis = mosaicism. If it occurs during meiosis = loss or gain of a chromosome, i.e., Down Syndrome. Translocations: balanced = breakage and reunion with no loss of genetic material = higher risk in subsequent generations. Unbalanced = loss of genetic material, i.e., Down Syndrome. Chromosomal and Genetic Factors: Numerical (from nondisjunction) Down (Trisomy 21), Klinefelter (XXY), Turner (gonadal dysgenesis XO) Structural, partial deletions - cri du chat microdeletions - Prader-Willi, Angelman = imprinting = deletion from father = PW; if from mother = Angelman Mutations (single genes) FISH – fluorescence in situ hybridization: diagnosis of deletions of genetic material using fluorescent-specific DNA probes. Oogenesis: primary oocytes—held in prophase of 1st meiotic division by oocyte maturation inhibitor (OMI) secreted by follicular cells (granulosa cells). Primary follicle, secondary or antral follicle, preovulatory 2 Spermatogenesis = cell division and shape changes Type A spermatogonia = mitosis Type B spermatogonia = primary spermatocytes (meiosis I forms secondary spermatocytes, meiosis II = spermatids) Spermiogenesis - shape changes and acrosome formation Sertoli cells = nurse cells. Interstitial cells of Leydig = testosterone 3 Lecture 2: Ovulation to Implantation, Bilaminar Germ Disc (Chapters 2 and 3) 1. Compare the ovarian cycle with the endometrial cycle. 2. Describe the process of fertilization and discuss at least four results accomplished by union of the gametes. 3. Define the normal site of implantation and list the more common sites of ectopic pregnancy. 4. Trace the period of development from zygote to blastocyst formation. 5. Describe primary villus formation in the placenta and the role of the cytotrophoblast and syncytiotrophoblast. Terms to define: gonadotropin-releasing hormone, follicl- stimulating hormone, luteinizing hormone, chorionic gonadotropin, capacitation, zona pellucida, morulla, blastocyst, embryoblast, trophoblast, cytotrophoblast, syncytiotrophoblast, hypoblast, epiblast, imprinting The Bottom Line, Chapters 2 and 3 Hypothalamus secretes gonadotropin-releasing hormones (GnRH); these signal the pituitary to secrete the gonadotropins, follicle-stimulating hormone (FSH), and leuteinizing hormone (LH). FSH stimulates maturation of follicles. LH surge stimulates ovulation at 14th day of cycle. Ovulation - oocyte (completes meiosis I, stops in metaphase of meiosis II) surrounded by follicular cells = the corona radiata. Captured by fimbriae of uterine tube into ampulla. Corpus luteum = granulosa cells and theca interna = progesterone. If fertilization occurs, then the corpus luteum is maintained by human chorionic gonadotropin (hCG) produced by the syncytiotrophoblast = forms basis for a pregnancy test. Fertilization = ampulla of uterine tube. Capacitation = maturation of sperm in female reproductive tract. Acrosome reaction = release of enzymes by sperm to dissolve zona pellucida (ZP). ZP = receptors for sperm. Fusion of oocyte and sperm membranes triggers: cortical and zona reactions = prevents polyspermy oocyte completes meiosis II egg is activated After fusion of pronuclei, division of the blastomeres forms a morula. Compaction is followed by formation of the blastocyst consisting of an inner cell mass = embryo, and an outer cell mass = trophoblast (placenta). Uterus: proliferative phase (estrogen), progestational phase (progesterone, corpus luteum), menstrual phase (basal layer of endometrium remains to regenerate. 4 Trophoblast secretes hCG = maintenance of corpus luteum that makes progesterone to maintain pregnancy. No fertilization = no hCG = corpus luteum regresses = no more progesterone = menstruation, leaving the basal layer to regenerate endometrial glands for next cycle. Second week: Trophoblast consists of two layers = cytotrophoblast (makes cells), syncytiotrophoblast = invasion and hormones. Inner cell mass = germ disc = two layers: epiblast and hypoblast. Two cavities: amniotic = dorsal to epiblast; yolk sac = ventral to hypoblast. Extraembryonic mesoderm formed around the amniotic and yolk sac cavities = splits into two layers = somatic and splanchnic. Cavity between = chorionic cavity. Two layers of extraembryonic mesoderm connected at connecting stalk (umbilical region). At about 12-14 days, the embryo penetrates uterine vessels = some bleeding = may misdiagnose as menstrual bleeding = misdiagnose pregnancy and age of embryo. Ectopic pregnancy = ampullary region = most common. Rectouterine (Douglas) pouch = most common in abdomen. Week 2 - week of 2s: 2 layers to trophoblast: syncytiotrophoblast and cytotrophoblast 2 layers to embryoblast: epiblast and hypoblast 2 cavities: amniotic and yolk sac 2 layers of extraembryonic mesoderm: somatic and splanchnic 5 Lecture 3: Trilaminar Germ Disc (Chapter 4) 1. Describe the process of gastrulation and distinguish it from the process of neurulation. 2. 3. 4. 5. 6. Name the three germ layers and describe their origins. What is the organizer and what does it organize? Define the term notochord and describe its significance. When is laterality established? What is the embryologic basis for caudal dysgenesis (sirenomelia) and sacrococcygeal teratomas? Terms to define: primitive streak, node and pit, notochord, prechordal plate, cloacal membrane, neural plate, neurectoderm, caudal dysgenesis The Bottom Line, Chapter 4 Gastrulation = process of making three germ layers: ectoderm (skin, CNS), mesoderm (blood, bones, connective tissue), and endoderm (gut, parenchyma of glands). Epiblast = forms all three germ layers = all of the embryo. Hypoblast disappears. Primitive streak forms at the caudal end of embryo at the beginning of the third week = cell migration from epiblast to form germ layers. Node = organizer = cranial end of streak = notochord cells. Notochord = induces CNS, forms nucleus pulposus in intervertebral discs. Anterior-posterior axis specified by the anterior visceral endoderm (AVE) = expresses OTX2, LIM1, and HESX1 and the secreted factor cerberus. Head mesoderm organized by Goosecoid and other genes that antagonize BMP-4. BMP-4 ventralizes mesoderm = forms intermediate and lateral plate mesoderm. Brachyury (T gene) controls formation of dorsal mesoderm in regions caudal to the head = caudal dysgenesis. FGF8 and nodal regulate left right asymmetry during gastrulation. Caudal dysgenesis = insufficient mesoderm formed by gastrulation = missing kidneys, fused lower limbs. Situs inversus = transposition of the viscera = usually no other defects. Laterality sequences = incomplete situs inversus = one or more organs = often have other defects. Trophoblast = forms villi for placenta = vessels formed in extraembryonic mesoderm connect to umbilical vessels = fetal circulation. Week 3 = week of 3s: 3 germ layers: ectoderm, mesoderm, endoderm 6 3 cavities: amniotic, yolk sac, chorionic 7 Lecture 4: Embryonic Period (Chapter 5) 1. Name the major derivatives of the three germ layers. 2. Explain why the embryonic period is considered the most critical time in human development for induction of birth defects. 3. What is a homeobox gene? What role do they play in specifying the anterioposterior axis? Terms to define: neural tube, neuropores, neural crest, placode, somite, dermomyotome, sclerotome, vitelline duct, crown rump length, intraembryonic coelom (cavity), visceral and parietal mesoderm The Bottom Line, Chapter 5 Ectoderm: forms neural plate = induced by organizer, notochord, and prechordal mesoderm = block BMP-4 activity. Neural plate folds into a tube = CNS. Cells at top of neural folds = neural crest = migrate to form bones and connective tissue of the face and skull, spinal ganglia, sympathetic and enteric ganglia, melanocytes, adrenal medulla, cranial nerve ganglia (V, VII, IX, X). Mesoderm paraxial (dorsal) = somites = vertebral column. Somitomeres form in head region and contribute to the base of the skull intermediate (ventral) = urogenital structures lateral plate (ventral) = splits into splanchnic (visceral, surrounds organs) and somatic (parietal, lines body cavities) Mesenchyme = any loose connective tissue regardless of origin. Mesoderm = derived from mesodermal germ layer. Somites = sclerotome (bone), myotome (muscle), dermatome (skin). Sonic hedgehog from notochord and floor plate of neural tube induces sclerotome. Endoderm = gut tube and its derivatives. Cephalocaudal (head and tail folds) and lateral folding closes gut tube around the umbilical region. Vitelline duct (yolk sac duct) connects gut tube to yolk sac. Gut divided into fore-, mid-, and hindgut = closed at the cranial (buccopharyngeal membrane) and caudal (cloacal membrane) ends. Homeobox genes = contain conserved DNA binding motif; grouped into four clusters; regulate anterior-posterior patterning of embryo. 8 Cloaca = expanded portion of hindgut = allantois forms off of cloaca = later forms bladder. Crown rump length (CRL) = head to tip of buttocks. Period of organogenesis = third to eighth weeks = most sensitive to teratogenic insult. 9 Lecture 5: Fetal Development, Fetal Membranes, and Placenta (Chapter 6) 1. Determine the time of pregnancy. 2. Understand what is meant by fetal period versus embryonic period. 3. Know when in gestation most of the increase in fetal length versus fetal weight occurs. 4. Describe the formation of the amnion, primitive and secondary yolk sacs, and intra- and extraembryonic coeloms (cavities). 5. Understand the functions of the placenta. 6. Understand the origin of dizygotic, monozygotic, and conjoined twins. Terms to define: amnion, chorion, terminal villi, chorionic plate, cotyledons, hydramnios, oligohydramnios, amniotic bands, conjoined twins The Bottom Line, Chapter 6 Fetal period = ninth week to birth. Pregnancy = 40 weeks after onset of last normal menstrual period (LNMP) or 38 weeks after fertilization. Fetal length = first half of pregnancy. Fetal weight = second half = 50% in last 2 1/2 months = why pregnancy should last as long as possible. Placenta (see Fig. 6.10) Fetal portion = chorion frondosum = villi. Maternal portion = deciduas basalis of the uterus. Implantation site grows = amnion fuses with chorion = amniochorionic membrane = forms hydrostatic wedge and ruptures during labor. Chorion fuses with outer wall of uterus obliterating uterine cavity. Cotyledons = septa from deciduas basalis that separate villi into groups (15-20). Placental circulation = fetal separate from maternal. Still get some fetal cells into maternal circulation. Placental functions: Exchange gases, nutrients, etc. 10 Transmission of antibodies. May develop reaction to fetal blood cells (isoimmunization) = Rh incompatibility = fetus is R positive, mother Rh negative = hemolytic disease of the newborn (erythroblastosis fetalis) can be prevented by anti Rh immunoglobulin. Hormone production = progesterone. Twins – not normal = increased risk of mortality and morbidity. Dizygotic = two eggs. Monozygotic = one egg, usually splits at early blastocyst stage. Conjoined = splitting or duplication of primitive streak. 11 Lecture 6: Birth Defects and Prenatal Diagnosis (Chapter 7) 1. Understand when and why prenatal diagnosis tests are conducted. 2. Define the terms congenital malformations, teratogen, teratology, and dysmorphology. 3. Estimate the percentage of liveborn infants that will have congenital malformations and provide reasons why this estimate will vary from one study and one region of the world to another. 4. Describe the factors determining the action of a teratogen (principles of teratology). 5. Gain an appreciation for the type of defects that can be diagnosed prenatally. 6. Obtain a better perspective of the embryonic versus the fetal period of development. 7. Appreciate the problem of birth defects and learn what physicians can do to prevent them. 8. Define the most sensitive period to a teratogen. 9. Distinguish between the terms “low birth weight” and “prematurity.” Terms to define: teratology, malformation, syndrome, amniocentesis, chorionic villus biopsy, ultrasound, alpha fetoprotein The Bottom Line, Chapter 7 Teratology = study of congenital malformations (birth defects), 2%-3% present at birth, 2%3% more diagnosed in first year of life: leading cause of infant deaths. Most are caused during the third to eighth weeks = period of organogenesis. Prematurity = born before 37 weeks of gestation = second leading cause of infant death. Low birth weight = intrauterine growth retardation (IUGR) = small for gestational age = learning and other disorders. Syndrome = groups of anomalies occurring together with a common etiology. Environmental factors: Viruses = either directly or by fevers Radiation Chemicals: thalidomide, alcohol (fetal alcohol syndrome) = leading cause of mental retardation, other drugs of abuse, lead Antiepileptic agents = teratogens. Maternal disease = diabetes, PKU. Nutritional deficiencies, folic acid prevents up to 70% of all neural tube defects (NTDs) if given by 2 months preconceptionally and continued throughout pregnancy. Susceptibility = dose, time of exposure, genetics (mother and fetus), duration of exposure. Male-mediated teratogenesis = seminal fluid, household contamination from the work place, germ cell mutations, imprinting. 12 Prevention = folic acid, maternal diabetes, antiepileptic agents, alcohol, PKU. Prenatal diagnosis: Ultrasound: used to determine age, birth defects, sex. Amniocentesis – alphafetoprotein (AFP) = in amniotic fluid = elevated in babies with NTDs and abdominal wall defects. Done around 14 weeks to get enough amniotic fluid. Also get cells = culture = genetic abnormalities. Do serum alphafetoprotein of mother first = 95% accurate. Chorionic villus sampling (CVS) = piece of villus = cells = genetic analysis. Done earlier than amniocentesis, cannot do AFP. Tests done on high-risk mothers = advanced age, previous problem, genetic history 13 Lecture 7: Skeletal System (Chapter 8) 1. Describe the bony derivatives of the sclerotome, somatic mesoderm of the body wall, and the neural crest. 2. Contrast development of the membranous versus the cartilaginous neurocranium. 3. Define the terms suture and fontanelle and describe their locations and functions. 4. Define craniosynostosis and its leading genetic cause. 5. Describe the basic processes of limb development and define apical ectodermal ridge, hyaline cartilage model, and epiphyseal plate. 6. What genes control proxinodistal, anterior posterior growth, and bone patterning in the limbs? 7. Describe vertebral formation and determine the origin of the intersegmental arrangement of the vertebral column. Terms to define: somitomeres, somites, suture, fontanelle, cranioschisis, craniostenosis (craniosynostosis), apical ectodermal ridge (AER), zone of polarizing activity (ZPA), meromelia, polydactyly, syndactyly The Bottom Line, Chapter 8 Somites (body), somitomeres (head) = paraxial mesoderm. Somites = dermatome (skin), myotome (muscle), sclerotome (bone). Mesoderm = from the germ layer. Mesenchyme = any loose connective tissue regardless of origin, i.e., neural crest. Skull Neurocranium = skull: flat bones = intramembranous; chondrocranium: formed in cartilage first = bones of base. Prechordal = neural crest = cranial to pituitary: rest = paraxial mesoderm. Sutures = coronal, sagittal, etc., form seams that allow moulding of the head during birth. Craniosynostosis = early fusion of the sutures = misshapened skull = many of these defects result from mutations in fibroblast growth factor receptors (FGFRs). Fontanelles = soft spots. Viscerocranium = face = mostly first and second pharyngeal arches = neural crest cells. First arch = maxilla, mandible, malleus, incus; second arch = stapes, part of hyoid bone. Limbs = buds form during fourth and fifth weeks at positions specified by HOX genes. 14 AER = apical ectodermal ridge = proximodistal growth = FGFs. Cell death in ridge = digits. ZPA = zone of polarizing activity = cranial to caudal (anterior-posterior) patterning; thumb to little finger = sonic hedgehog and retinoic acid = morphogens. Bone patterning = HOX genes. Amelia = no limbs; meromelia = short limbs; thalidomide = limb defects, now an anticancer, anti-AIDS drug. Polydactyly = too many digits, syndactyly = fused digits. Vertebral column: derived from somites (scleretome) and from notochord (nucleus pulposus of invertebral disc). Caudal part of one sclerotome fuses with cranial part of another = intersegmental so that muscles bridge the vertebra to act on them. 15 Lecture 8: Muscular System and Body Cavities (Chapters 9 and 10) 1. Describe the muscular derivatives of the epimeres and hypomeres. 2. Describe the origins of the innervation of the segmental musculature. 3. Describe the processes of cephalocaudal and lateral folding of the embryonic disc and their significance with respect to establishment of body form. 4. What is the embryologic basis for gastroschisis versus omphalocele and ectopia cordis? 5. Describe the subdivisions of the intraembryonic mesoderm and the role this tissue plays in development of the intraembryonic coelomic cavity. 6. Describe the role of the pleuropericardial folds in determining the pericardial and pleural cavities. 7. Describe the formation of the diaphragm and explain the origins of diaphragmatic hernias. Terms to define: dermomyotome, epimere, hypomere, visceral and parietal mesoderm, serous membrane, septum transversum The Bottom Line, Chapters 9 and 10 Muscles: Skeletal = paraxial mesoderm = muscle cells from somites and somitomeres. Myotome = epimere = extensor muscles of vertebral column = dorsal primary rami. Hypomere = formed from migration of dorsolateral cells in somite = carry nerve of origin with them = ventral primary rami. Head = somitomeres = tongue, eye (except those of the iris = optic cup) and pharyngeal arches. Muscles in the head are patterned by connective tissue that is formed by neural crest. Limb = dorsolateral cells from somite = directed by connective tissue formed by lateral plate mesoderm—regulated by Myo D genes = transcription factors. Cardiac: splanchnic mesoderm around heart tube. Smooth: splanchnic mesoderm around gut tube. Body cavity = same as intraembryonic coelom (cavity) = will form; cardiac, pleural, and peritoneal cavities = all three cavities derived from space between the two layers of the lateral plate mesoderm: splanchnic (visceral) layer = surrounds gut tube, heart, and lungs; somatic (parietal) layer = lines body wall. Two sides of cavity are brought together by embryonic folding = caudal and cranial folds and two lateral folds = draws everything around the umbilical region. Cleft sternum = failure of folds to close. Two layers of lateral plate mesoderm form serous membranes that secrete fluid for lubrication. Two layers continuous at the root of each organ. 16 Gut is suspended by dorsal mesentery = double layer of peritoneum = where two layers are continuous . Division of cavities: Septum transversum = block of mesentery = lies in anterior region between cardiac and peritoneal cavities = positioned by caudal folding that curved the heart into the thoracic region. Pericardioperitoneal canals = posterior to septum transversum = connect primitive cavities. Pleuroperitoneal membranes close pericardioperitoneal canals behind the liver. Pleuropericardial folds (membranes) grow around the heart = separate pleural and cardiac cavities = form the fibrous pericardium. Diaphragm formed by: Pleuroperitoneal membranes. Septum transversum = central tendon. Muscular components = from cervical myotomes C3, 4, 5 = carry phrenic nerve with them. Mesentery of the esophagus = crura. Diaphragmatic hernia = usually on left = failure of pleuroperitoneal membrane to close pericardioperitoneal canal = abdominal organs may compress lungs and heart. 17 Lectures 9 and 10: Cardiovascular System I and II (Chapter 11) 1. Explain the role of cephalocaudal and lateral embryonic folding in positioning of the heart tube. 2. Define the term cardiac loop and describe its formation. 3. Identify the bulbus cordis, conus cordis, and truncus arteriosus and name their derivatives. 4. Describe the contributions of the sinus venosus to atrial development. 5. Describe the processes involved in septation of the atria, ventricles, and truncus arteriosus, including the role of the endocardial cushions. 6. Explain the embryologic origins of ventricular septal defects (VSD), atrial septal defects (ASD), and transposition defects of the great vessels. 7. Know the derivatives of the third, fourth, and sixth aortic arches. 8. Understand that arteries shift to the left and veins to the right during development. 9. Describe the origin of the umbilical vein, the portal system, and the inferior vena cava. 10. Trace the patterns of pre- and postnatal blood flow and describe the changes that occur at birth. 11. Determine the identity of the tinman. Terms to define: endocardial cushions, foramen ovale, double aortic arch, vascular ring (around the trachea and esophagus), Tetralogy of Fallot, ductus arteriosus, coarctation of the aorta The Bottom Line, Chapter 11 Heart development Starts as horseshoe tube cranial to the cranial neural folds, brought to thoracic cavity by cranial folding. BMPs (TGF- family) plus WNT inhibition induces NKX 2-5, which establishes cardiogenic field. TBX5 (T Box transcription factor) regulates septation. Endocardium = lines heart cavity = same as blood vessels. Myocardium = muscle cells. Epicardium = same as visceral pericardium: parietal pericardium lines inside of fibrous pericardium. Fibrous pericardium comes from pleuropericardial folds. Heart loop = cranial end grows vertically and to the right; caudal end grows dorsally and to the left = helps distinguish atria, ventricles, and outflow tract as these regions expand. Atrioventricular junction = canal = will be separated into two channels = right and left AV canals. Outflow tract = conus cordis into truncus arteriosus = will become pulmonary and aortic channels. 18 Sinus venosus = primitive receiving end of the heart = right and left sinus horns = each receives umbilical, vitelline, and common cardinal veins. Veins shift to right = left sinus horn diminishes, right increases in size to form smooth-walled portion of the right atrium (trabeculated part of right atrium is derived from the original primitive right atrium. Crista terminalis = dividing line between smooth [sinus venarum] and trabeculated parts). Valves guard opening into smooth portion of right atrium = valve of the inferior vena cava and valve of the coronary sinus. Left sinus horn = forms oblique vein of left atrium and the coronary sinus. Septum formation: key = endocardial cushions = areas of expanded matrix production between the endocardium and myocardium = form in AV canals (four of them) and in conotruncal region. The key to the origin of most heart defects involves problems with endocardial cushions. Atrial septum: septum primum grows toward AV endocardial cushions, but before fuses, cell death creates a hole = ostium secundum. Septum secundum grows toward cushion, but never gets there = forms valve over ostium secundum = new opening = foramen ovale. Septum primum = valve of the foramen ovale. Probe patency of the foramen ovale = valve does not close completely at birth. Left atrium = smooth part = from outgrowth of pulmonary vessel that later gets incorporated. Trabeculated = original left atrium. AV valves = superior and inferior endocardial cushions grow together. Valves formed by thinning of cushions, right = tricuspid, left = bicuspid (mitral). Conus and truncus septation = conotruncal cushions spiral and fuse in midline to create pulmonary and aortic vessels. Neural crest cells help form truncus cushions = basis for many heart defects. Often, heart and craniofacial abnormalities go together = both result from insult to neural crest. Ventricular septation: created by growth of the muscular portion (expansion of the ventricular chambers) and membranous portion (at top; growth of the inferior endocardial cushion). Membranous portion = where most ventricular septal defects occur. Heart defects: Transposition of great vessels = conotruncal cushions do not spiral. Stenosis = when these cushions grow to far off center. Tetralogy of Fallot = anterior displacement of conotruncal septum. Leads to four problems: (1) pulmonary stenosis, (2) hypertrophy of the right ventricle, (3) overriding aorta, (4) ventricular septal defects. Dextrocardia: heart loops the opposite way, usually associated with transposition of other organs = situs inversus = loss of left/right symmetry. 19 Vascular development Arterial system: Aortic arches (5 pairs) associated with pharyngeal arches = arise from aortic sac off the heart outflow tract, course through pharyngeal arches, undergo modification: Aortic sac splits into brachiocephalic and aortic arch 1st arch = mostly disappears, leaves maxillary artery 2nd arch = mostly disappears, leaves hyoid and stapedial artery 3rd arch = carotid system 4th arch = persists on both sides = subclavian and part of the aortic arch 6th arch = forms pulmonary arteries = on left, the distal part persists as the ductus arteriosus Vitelline arteries supply the gut: celiac = foregut; superior mesenteric = midgut; inferior mesenteric = hindgut. Umbilical arteries: join common iliacs and ultimately become internal iliacs and medial umbilical ligaments. Arterial defects: (1) Patent ductus (2) Coarctation of aorta: preductal and postductal = blood finds ways around the block. May be due to abnormal location or too many receptors for bradykinin, secreted by the lungs and responsible for signaling closure of the ductus (3) Double aortic arch = difficulty swallowing = both parts of dorsal aorta remain Venous system Vitelline v = gut and liver, left disappears, right = hepatic sinusoids, hepato cardiac portion of inf vena cava, portal v, sup mesenteric v. Umbilical v: right disappears; left connects placenta to inf vena cava = ductus venosus = bypasses liver and later becomes the ligamentum teres; ductus becomes ligamentum venosum. Cardinal v: drain body wall. As organs form new v develop to drain them and all shift to the right = lots of variations because pressure is low. Anterior and post cardinal v drain to common cardinals to heart. Subcardinals = kidneys, sacrocardinals = lower limbs, supracardinals = body wall via 20 intercostals. L braciocephalic = anastomosis between ant card v. Sup vena cava = R common and R ant cardinal v. L renal v = anastomosis between subcardinal v. L common iliac v = anastomosis of sacrocardinal v. Sacrocardinal and subcardinal on R = inf vena cava. Circulatory changes at birth: Before birth: blood flow in fetus = umbilical v from placenta (oxygenated) to ductus venosus (bypasses liver) to inf vena cava to R atrium to L atrium through foramen ovale to L ventricle to aorta to umbilical arteries to placenta (little blood goes to R ventricle because pulmonary circulation not functional = lungs not working. Any blood in R ventricle goes out pulmonary vessel and through ductus arteriosus into aorta.) After birth: sphincter regulating flow in ductus venosus closes (ligamentum venosum), umbilical arteries close (medical umbilical ligaments), umbilical v closes (lig teres), ductus arteriosus closes (bradykinin from lungs causes closure = lig arteriosum), foramen ovale closes. 21 Lecture 11: Respiratory System and Digestive System (Mesenteries) Chapters 12 and 13, to p 289 1. Define the terms respiratory distress syndrome and hyaline membrane disease. 2. Describe the factors involved in lung maturation, including the role of alveolar type I and II cells. 3. Describe the relationship of the cephalocaudal and lateral folding of the embryo to development of the foregut, midgut, and hindgut regions. Terms to define: visceral and parietal pleura, surfactant, intraperitoneal, retroperitoneal, dorsal and ventral mesentery The Bottom Line, Chapters 12 and 13 (to p 289) Lung bud (respiratory diverticulum) grows off foregut = endoderm = lung cells, splanchnic mesoderm surrounding gut tube = connective tissue. Esophagotracheal septum = separates esophagus and trachea. Esophageal atresia with or without fistulas = abnormal septation. Lung bud divides = bronchial buds = divides and branches into lungs to create bronchopulmonary segments and ultimately alveoli. Lungs keep making divisions (6) postnatally. Cells in lungs = alveolar cells: Type I = blood air barrier = very thin. Type II = make surfactant, a phospholipid, that decreases surface tension = essential to keep alveoli open = not made until 28 weeks = premature babies have trouble = respiratory distress syndrome = insufficient surfactant = give artificial surfactant (exosurf). Pleura = visceral (around lung, derived from splanchnic mesoderm); parietal = around body wall. Two are continuous at hilus area: space between layers = pleural cavity. Mesentery = double layer of peritoneum: Visceral peritoneum = around the organ; parietal peritoneum = on body wall. Both layers are continuous where parietal layer leaves body wall to surround the organ. Mesenteries = suspend organs from body wall = allow for passage of blood and lymph vessels and nerves. Dorsal mesentery extends from the caudal region of the esophagus to the end of the hindgut. In stomach area = dorsal mesogastrium = forms greater omentum. Also have dorsal mesoduodenum, dorsal mesocolon. Dorsal mesentery to jejunum and ileum = mesentery proper. Ventral mesentery forms from thinning of septum transversum. Only exists from caudal esophagus to upper part of duodenum. Lesser omentum = ventral mesentery extending from the gut tube to liver. Falciform ligament = part from liver to ventral body wall = contains umbilical v = 22 ligament teres Peritoneal ligaments = mesenteries joining organs or attaching organs to the body wall. 23 Lecture 12: Digestive System: Fore-, Mid-, and Hindgut (Chapter 13, starting p 289) 1. List the derivatives of the fore-, mid-, and hindgut regions and briefly describe their morphogenesis. 2. Describe the formation of the liver and its function during fetal life. 3. Describe the process of gut rotation and its role in producing retroperitoneal versus intraperitoneal structures. 4. Describe the vascular supply of the primitive gut tube. How does this arrangement compare to hat in the adult? 5. Define the term physiological umbilical herniation and the time and reasons for its occurrence. 6. Describe the embryologic origin of the following defects: congenital umbilical hernia, left-sided colon, Meckel's diverticulum, gut stenosis, gastroschisis, and omphalocele. Terms to define: omental bursa, retroperitoneal, epiploic foramen (of Winslow), falciform ligament, portal triad, annular pancreas The Bottom Line, Chapter 13 (starting at p 289) Foregut = outgrowth of organs = lungs, pancreas, gall bladder, liver. Endoderm forms parenchyma of these tissues; splanchnic mesoderm around gut tube forms connective tissue. Stomach also from foregut–rotates and pulls mesenteries with it (ventral and dorsal). Dorsal grows down = greater omentum. Ventral = lesser omentum connected to liver; free margin of the lesser omentum = roof of epiploic foramen (of Winslow) = entrance to lesser sac. Free margin also contains portal triad = bile duct, portal v, hepatic artery. Greater sac = rest of peritoneal cavity. Celiac artery = a to foregut. Liver = hematopoietic organ. Duodenum = fuses to posterior body wall except cap (secondarily retroperitoneal). Duodenal atresias are a result of problems of recanalization. Pancreas = two buds = two ducts: accessory (of Santorini) and main (of Wirsung). Buds may surround duodenum, causing stenosis. Midgut = forms primary loop with mesenteric artery as axis. Rotates 270 (around axis and herniates out umbilicus (6th week); gut returns to cavity in tenth week. Omphalocoele = gut fails to return = usually associated with other defects, also increased AFP. Gastroschisis = gut comes back and then herniates through the body wall = usually no other defects. Vitellinc duct = connects yolk sac to midgut = if remains = Meckel's diverticulum. Atresias and stenosis of midgut = vascular accidents. Hindgut = ends in cloaca, supplied by inf mesenteric a. Urorectal septum separates cloaca from hindgut. Hindgut extends from left third of the transverse colon to upper two thirds of anal canal. 24 Anal canal supplied by sup and mid rectal a (upper two thirds) and inf rectal a (lower third, because the lower part is derived from ectoderm). Congenital megacolon (Hirschsprung’s disease = no ganglia in smooth muscle of gut = no neural crest = no mobility). 25 Lecture 13: Urogenital System: Urinary System (Chapter 14, to p 337) 1. Describe the role of the intermediate mesoderm in development of the urinary system. 2. Define the terms pronephros, mesonephros, and metanephros. 3. List the derivatives of the ureteric bud and the metanephric mesoderm. 4. Understand the importance of epithelial mesenchymal interactions in kidney developments. 5. Describe the embryologic origin of congenital cystic kidney, renal agenesis, double ureter, and horseshoe and pelvic kidneys. 6. Describe the formation of the urinary bladder and the urogenital sinus. Terms to define: nephron, glomerulus, renal corpuscle, urorectal septum The Bottom Line, Chapter 14 (to p 337) Urogenital system = mostly from intermediate mesoderm Three kidneys in succession: Pronephros = cervical = nonfunctional. Mesonephros = thoracolumbar: duct = mesonephric duct. Metanephros = definitive kidney. Collecting system = ureteric bud off mesonephric duct grows into and induces metanephric blastema = (intermediate) mesoderm. Bud continues to divide = forms ureter, renal pelvis, major and minor calyces, collecting tubules. Metanephric mesoderm induced by ureteric bud forms filtration system = glomerulus, Bowman's capsule, proximal convoluted tubule, loop of Henle, and distal convoluted tubule. WT 1 gene = kidney gene = allows mesoderm to be induced by ureteric buds. Kidney development is dependent upon epithelial-mesenchymal interactions. Congenital polycystic kidney = proximal convoluted tubules do not form properly. Kidneys form in pelvis. Differential growth moves them into lumbar region. If kidneys fuse = horseshoe kidney = gets stuck on inf mesenteric a. Urorectal septum = separates hindgut from cloaca which forms primitive urogenital sinus Bladder forms from upper part of urogenital sinus = expands and incorporates ureters; mesopheric ducts move lower to enter urethra where prostate forms. Part of ducts incorporated into bladder forms trigone area of bladder. Bladder connected to umbilicus by urachus (old allantois) = median umbilical ligament. 26 Lecture 14: Urogenital System: Genital System (Chapter 14, starting p 337) 1. Define the terms genital ridge and indifferent gonad and describe the changes that occur when the primordial germ cells arrive carrying an XY chromosome complement. 2. Contrast the development of the mesonephric and paramesonephric duct systems and their derivatives in the male and female. 3. Describe the formation of the vagina. 4. Contrast the fate of the genital tubercle, urethral folds, and genital swellings in the male and female. 5. Describe the process involving descent of the testes from the abdominal cavity into the scrotum and define a congenital inguinal hernia. Terms to define: testis determining factor, testosterone, dihydrotestosterone, hypospadias, pseudohermaphrodites, testicular feminization syndrome The Bottom Line, Chapter 14 (starting on p 337) Y chromosome = testis determining factor gene (TDF) on the sex determining region (SRY) = regulates male development. Genital ridges = ovaries or testes = germ cells from the yolk sac migrate to the ridges and arrive in the sixth week and enter the primitive sex cords. Primitive cords remain in male = seminiferous tubules = lose contact with surface that gets covered by tunica albuginea. Sertoli cells = nurse cells for sperm. Interstitial cells (Leydig) = testosterone. Seminiferous tubules = old sex cords = canalize at puberty. In female primitive cords degenerate = cortical cords form and then form follicular cells around germ cells. Both sexes have: Mesonephric duct = remains in male, lost in female = remnants may be cysts. Paramesonephric duct (Mullerian) = lost in male = mullerian inhibiting substance (MIS) or antimullerian hormone made by Sertoli cells. Ducts remain in female = no Sertoli cells = no MIS. Mesonephros contributes tubules for male ducts = efferent ducts (from old excretory tubules), epididymis, seminal vesical, ductus deferus (all from mesonephric duct). Paramesonephric duct = uterine tubes (Fallopian), uterus, upper part of vagina. Rest of vagina = from urogenital sinus = vaginal bulbs. 27 External genitalia: start with genital tubercle and cloacal folds around cloacal membrane. Urorectal septum separates region into urogenital (surrounded by urethral folds) and anal (surrounded by anal folds) areas. Genital swellings form on sides of urethral folds. Genital tubercle Urethral folds Genital swellings In Male penis fuse = urethra fuse = scrotum In Female clitoris no fusion = labia minora no fusion = labia majora Testicular feminization (androgen insensitivity): 46XY, but tissues unresponsive to testosterone. Testosterone = mesonephric ducts internal structures. Dihydrotestosterone = external genitalia. No testosterone plus estrogen = female. Descent of testes = develop in abdomen, descend to scrotum through internal ring, inguinal canal, external ring: preceded by processes vaginalis that later surrounds each testis as the tunica vaginalis. Gubernaculum attaches to caudal pole and to scrotum = assists in descent. As testes passes through the abdominal wall it picks up layers: Fascia transversalis = internal spermatic fascia. Internal abdominal oblique = cremaster fascia and muscle. External abdominal oblique = external spermatic fascia. Cryptorchism = one or both testes do not descend. Inguinal hernia (indirect) = processes vaginalis fails to close and intestines pass through rings to scrotum. Ovary descends = ligament of ovary = round ligament of uterus. Attachment of the ligament to the uterus prevents ovary from reaching labia majora. 28 Lectures 15 and 16: Head and Neck (Chapter 15) 1. Define the terms pharyngeal arch, pouch, and cleft. 2. Define the term HOX code and what it means with respect to arch development. 3. Know the derivatives of the first and second arches, the first cleft and pouch, and that the remaining pouches give rise to the parenchyma of numerous glands. 4. Know the nerves associated with each arch. 5. Describe the origin of the tongue, including its nerve supply. 6. Explain the origin of the thyroid gland, how it assumes its final position in the adult, and the formation of thyroglossal cysts. 7. Define the term facial prominences and describe their role in formation of the face. 8. Define the terms primary and secondary palate and explain the origins of clefts in these structures and the upper lip. Terms to define: ectodermal placodes, neural crest, cervical cyst, preauricular pit, DiGeorge sequence, nasolacrimal duct The Bottom Line, Chapter 15 (to p 386) Mesenchyme in head: Paraxial = somites and somitomeres = muscles, floor of brain case. Lateral plate = laryngeal cartilages and connective tissue. Neural crest = face and skull bones and all other tissues. Ectodermal placodes (with NC) = sensory ganglia V, VII, IX, X. Pharyngeal arches (branchial arches), like gills around pharynx = mesoderm core, endoderm (inside), ectoderm (outside), blood vessel (aortic arch), and cranial nerve. First arch = maxillary and mandibular = maxilla and mandible = muscles of mastication = trigeminal nerve (mandibular division). Second arch = muscles of facial expression, stapes and hyoid bones, facial nerve. Third arch = glossopharyngeal nerve. Fourth to sixth arches = vagus (superior laryngeal) muscles of pharynx, laryngeal cartilages: (recurrent branch) intrinsic muscles of larynx. Crest cells migrate from segmented regions of hindbrain, called rhombomeres, into the arches. Arch patterning regulated by HOX code carried to arches by crest cells. Pouches: One = auditory tube, middle ear. Two = palatine tonsils. Three = inf parathyroid and thymus. 29 Four = superior parathyroid. Fifth = parafollicular cells of thyroid = calcitonin. Clefts: One = ext. auditory meatus. Fistulas = lower clefts or pouches remain as openings. Neural crest cells form much of the face = if insulted = facial clefts = neural crest also form conotruncal septum in heart = explains why facial defects and heart defects often occur in combination if crest cells are affected. Tongue = ant two thirds = first arch = mandibular nerve; post third = mostly third arch = glossopharyngeal n; line between the two = terminal sulcus. Muscles = occipital somites = hypoglossal n; taste = facial n (chorda tympani). Thyroid gland = forms at base of tongue; descends in midline along thyroglossal duct: remnants or cysts may remain = midline. The Bottom Line, Chapter 15 (starting on p 386) Face = prominences = maxillary, mandibular, frontonasal, medial and lateral nasal (around nasal placodes, pits). Upper lip = fusion of two medial nasal prominences and maxillary. Lower lip = fusion of mandibular prominence. Nose = frontal prominence (bridge), medial nasal (crest and tip), lateral (alae). Nasolacrimal duct = between maxillary and lateral nasal prominences. Intermaxillary segment = medial nasal prominences merge = philtrum, incisor part of jaw, primary palate. Secondary palate = shelves off maxillary prominence elevate and fuse (incisive foramen = fusion of primary and secondary palates). Facial clefts: Median cleft lip = medial nasal prominences = often mentally retarded associated with holoprosencephaly = lacking midline of face and brain. Lateral cleft lip = between medial nasal and maxillary prominences. Oblique clefts = between maxillary and lateral nasal prominences. Cleft palate = maxillary prominence (palatal shelves). 30 Lecture 17: Ear and Eye (Chapters 16 and 17) 1. Define the terms external, middle, and internal ear and be able to describe their origins. 2. Describe the development of the tympanic cavity and the ear ossicles. 3. Describe the relationship of the optic cup to the brain vesicles and the lens placode. 4. Describe the origin of coloboma iridis. Terms to define: cochlea, semicircular canals, pupil, anophthalmia The Bottom Line, Chapters 16 and 17 Ear = internal, middle, external. Internal = otic placodes form otic vesicles = form cochlear duct, semicircular canals, and membranous labyrinth. Middle = tympanic cavity = contains malleus and incus (first arch) and stapes (second arch): tensor tympani (malleus) = trigeminal nerve; stapedius = facial nerve. External = meatus = first arch. Six auricular hillocks from first and second arches. External ear defects = common = often associated with other defects = good sign to look for additional birth defects. All frequently occurring chromosomal syndromes have ear abnormalities. Eye = optic cup and lens. Cup = outpocketing of diencephalon = invaginates to form two layers = neural and pigment layer of retina. Lens = from surface ectoderm induced by contact by optic cup. Optic stalk = outgrowth of diencephalon to cup = optic nerve has a groove = choroid fissure = hyaloid artery = becomes central artery of the retina. Pax6 = master gene for eye development. Coloboma = choroid fissure stays open. Microphthalmia = small eye. Anophthalmia = no eye = cup fails to form or make contact with ectoderm = usually other brain defects. Synophthalmia (cyclopia) = midline brain defect, brings eyes together. 31 Lecture 18: Integumentary and Central Nervous System (Chapters 18 and 19) 1. Describe the origin of the epidermis and dermis 2. Describe the establishment of the neural tube from the neural plate and segregation of the primary brain vesicles and their subsequent subdivisions. 3. Describe the passageway for cerebral spinal fluid. 4. Define the terms mantle and marginal layers, and basal, alar, roof, and floor plates. 5. Describe the origin of neuroblasts and glial cells. 6. Define the terms spina bifida, anencephaly, rachischisis, meningocele, myelomeningocele, and meningoencephalocele. 7. Describe the origin of the cerebellum, the cerebral cortex, and hypophysis (pituitary). 8. Describe the origin of the sympathetic and parasympathetic nervous systems. Terms to define: neuropore, neuroepithelium, sensory (dorsal root) ganglia, spinal nerve, lumbar puncture, hydrocephalus, harlequin fetus, polythelia, holoprosencephaly, Sonic hedgehog (SHH) The Bottom Line, Chapters 19 and 20 Skin = ectoderm = epidermis and dermis; melanocytes = neural crest. Mammary glands = mammary line = from axilla to groin = accessory nipples and glands. Central nervous system = neural plate = rolls into neural tube during fourth week (neural folds fuse). Cephalic end of tube forms three primary brain vesicles, later it subdivides: Prosencephalon (forebrain) = telencephalon (cerebral hemispheres); diencephalon = optic vesicles, thalamus. Mesencephalon (midbrain) = anterior (visual) and posterior (auditory) = does not subdivide. Rhombencephalon (hindbrain) = metencephalon (pons, cerebellum) and myelencephalon (medulla oblongata). Organizing centers = anterior neural ridge (ANR) = FGF8 = forebrain; isthmus (between hind- and midbrain) = mid- and hindbrain specification = FGF8. Spinal cord = neuroepithelial cells = proliferative cells. Mantle layer = grey matter. Marginal layer = outside = white matter = fiber tracts. Basal plates = motor horn cells. Alar plates = dorsal horns = sensory; separated from basal plates by sulcus limitans. Roof and floor plates = pathways. Neural crest cells = dorsal root (spinal ganglia) = sensory. Spinal nerves = ventral roots = motor; dorsal roots = sensory: split into dorsal and ventral 32 primary rami = motor and sensory fibers mixed. Spinal cord = full length of column at third month. Thereafter, vertebral column grows faster so cord ends at L2-L3. Spina bifida = open neural tube anywhere from cervical to lumbosacral area. Lumbosacral = most common = results from nonclosure of neural folds = 70% can be prevented by taking folic acid for at least 2 months preconception and throughout pregnancy. Occulta = tube closes, but vertebra do not = covered by skin. Increase risk if have one child. Anencephaly = cranial folds fail to close, death results = folic acid works as preventative. Brain = alar and basal plates like spinal cord = mostly alar (cerebral hemispheres) in forebrain. Sonic hedgehog secreted by notochord and floor plate of neural tube = ventralizing gene for basal plate and motor areas = spinal cord and brain. Pituitary gland = diencephalon (neurohypophysis, posterior lobe); Rathke's pouch off roof of stomadeum (adenohypophysis, anterior lobe). Pharyngeal hypophysis = remnants of Rathke's pouch, also craniopharyngiomas. Ventricles = connected via pathway from the lateral ventricles (cerebral hemispheres) through foramen of Monroe into third ventricle (diencephalon) into aqueduct of Sylvius (through midbrain) into fourth ventricle (hindbrain). Cerebrospinal fluid (CSF) is made by choroid plexuses in the ventricles and circulates through these connections. If the circulation of CSF is blocked, the fluid continues to be made but has nowhere to go, causing the brain to swell = hydrocephalus; usually blocked at aqueduct. Alcohol abuse = leading cause of mental retardation. Autonomic system: sympathetic and parasympathetic. Sympathetic = neural crest = paravertebral ganglia (sympathetic trunk ganglia) paraaortic ganglia (celiac, sup mesenteric, inf mesenteric); neural crest also contribute to the adrenal medulla. Parasympathetic = craniosacral = III, VII, IX, X and S2, 3, 4 = neural crest. Congenital megacolon = no parasympathetic ganglia in gut = no neural crest = no bowel movement. 33