* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Links between Infectious Diseases and Cardiovascular Disease: A
Middle East respiratory syndrome wikipedia , lookup
Oesophagostomum wikipedia , lookup
Marburg virus disease wikipedia , lookup
Hepatitis B wikipedia , lookup
Sexually transmitted infection wikipedia , lookup
Leptospirosis wikipedia , lookup
Schistosomiasis wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Chagas disease wikipedia , lookup
Onchocerciasis wikipedia , lookup
Eradication of infectious diseases wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
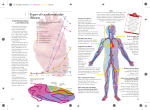
Links between Infectious Diseases and Cardiovascular Disease: A Growing Body of Evidence Kim Curry; Lauren Lawson Abstract It is widely acknowledged that a systemic inflammatory process is involved in atherogenesis leading to subsequent cardiovascular disease (CVD). Several types of microbes have been implicated as possible causative agents in acquired CVD. This article reviews current and emerging links established between specific microorganisms and cardiac vessel and other vascular damage. Studies are reviewed that have investigated a possible role for antibiotics in treatment and prevention; other potential primary and secondary preventive measures are then explored. Nurse practitioners have an important role in recognizing and effectively managing the multiple complex processes involved in the development of CVD. Introduction Cardiovascular disease (CVD) is the leading cause of death in industrialized nations. In the United States and other developed countries, risk factors such as smoking, high blood pressure, and elevated serum cholesterol levels are widely known and accepted as having a causative role in arteriosclerosis and the development of CVD. Much time and effort has been spent by both researchers and clinicians in investigating and attempting to modify these known risk factors. However, there is a growing body of evidence that other modifiable risk factors may also be at work. It is now widely acknowledged that a systemic inflammatory process is involved in atherogenesis leading to subsequent cardiac vessel disease and other vascular damage. Inflammatory markers such as C-reactive protein (CRP), fibrinogen, tumor necrosis factor alpha (TNF-α), and others can be used to measure systemic inflammation and risk of CVD. Patients with autoimmune diseases characterized by chronic systemic inflammation, such as rheumatoid arthritis (RA) and systemic lupus erythematosis (SLE), demonstrate a significantly increased risk of CVD. Several types of microbes are now also being implicated as possible causative agents in acquired CVD. A few bacterial agents have been the topic of research for several years. Organisms such as the spirochetes Borrelia burgdorferi (Lyme disease) and Treponema pallidum (syphilis), and flagellated bacteria such as the streptococci have well-recognized atherosclerotic potential. Now, additional studies are beginning to shed light on the possible role played by other bacterial and viral illnesses and the later development of atherosclerosis or other cardiovascular damage. Periodontal Disease The association between oral health and cardiovascular health has been the topic of clinical studies for over 20 years. Early studies indicated that patients with poor dental health were 1.3 to 1.7 times more likely to experience myocardial infarction than patients with good dental health.[1] Various mechanisms have been explored in an attempt to explain the relationship between dental and cardiovascular health. Periodontal disease involves inflammation and infection of the supportive structures for the teeth, including soft tissue and bone. Periodontal disease becomes established when plaque accumulation on the teeth causes an inflammatory response, resulting in detachment from the gums.[2] The majority of adults in the United States have a mild form of periodontal disease, but 20% to 30% of adults have more severe forms.[3] A number of studies have been conducted to elucidate the relationship between dental and cardiovascular health. The majority of studies have demonstrated that periodontal disease is a predictor of subsequent CVD.[4–6] However, not all studies have concluded that periodontal disease is a significant predictor. The main mechanism postulated in the subsequent development of CVD is that the chronic local infection characteristic of periodontitis increases the levels of systemic inflammatory chemicals. The increased presence of these inflammatory mediators promotes atherosclerosis.[7] Several periodontal pathogens have been found in atherosclerotic plaques in carotid arteries. [8] There are several confounding variables involved in establishing a firm link to periodontal disease. First, a number of different organisms have been implicated in periodontitis. These include Bacteroides forsythus, Porphyromonas gingivalis, and treponema denticola, among others. Second, multiple measures and definitions of periodontitis have been employed in the clinical studies completed to date. Third, there are several common elements involved in both periodontal disease and atherosclerosis. For example, both are more likely to occur in the elderly and in those with risk factors such as smoking, diabetes elevated cholesterol, and hypertension.[9] In conclusion, periodontal disease may be an independent or contributing risk factor for CVD. Not all studies have found a causal link, and further studies are needed to determine the extent of the relationship and whether outcomes are improved through preventive dental care. In the meantime, this area of health care is yet another in which inappropriate use of antibiotics is to be avoided. Patients with oral disease or decay should be referred for definitive dental care, with systemic medications used in conjunction with corrective treatment. Chlamydia Pneumoniae Chlamydia pneumoniae (C. pneumoniae) is a very common bacterial respiratory pathogen. About 50% of adults in the United States have been infected with C. pneumoniae by age 20. The germ causes 10% of community-acquired pneumonia cases in adults. Reinfection is common, as the organism is ubiquitous.[10] C. pneumoniae belongs to the same genus of organisms as Chlamydia trachomatas. C. pneumoniae is the most recently identified member of the genus, having first been cultured in 1965.[11] A number of studies have been conducted to determine the specific association between C. pneumoniae and the development of atherosclerotic plaque. This association was first suggested in 1988, when it was discovered that patients with CVD or acute myocardial infarction (AMI) were more likely to have antibodies to C. pneumoniae in their blood.[12] While a causative role has not been firmly established, C. pneumoniae has been detected in atherosclerotic plaques.[13] Arcari et al[14] studied the link between C. pneumoniae seropositivity and AMI in males aged 30 to 50. The authors found a significantly higher risk of AMI in patients who had high titers to C. pneumoniae immunoglobulin A (IgA) within the previous one to 5-year period. This risk persisted after adjusting for other cardiovascular risk factors. The complex pathophysiology involved in the development of vascular damage complicates the ability of researchers to link CVD to any particular cause or agent. Smoking, an independent CVD risk factor, has also been shown to be an independent risk factor for C. pneumoniae seropositivity. It has also been suggested that an exacerbation of C. pneumoniae infection through smoking cigarettes may increase the potential for a systemic infection and therefore increase the chance for development of atherogenesis.[15] Studies are underway to determine whether macrolide antibiotic therapy has a preventive role in reducing the subsequent development of CVD. However, controversy still exists concerning the actual cause-effect relationship, as it has been suggested that CVD may actually increase the susceptibility of the host to develop a chronic microbial infection, making the presence of C. pneumoniae an outcome, rather than a source, of CVD.[16] Helicobacter Pylori H. pylori is a known causal agent of several gastrointestinal diseases and has also been implicated in ischemic heart disease (IHD). Several different mechanisms are proposed for the role of H. pylori in IHD. There is speculation that H. pylori may act directly on atherosclerotic plaques, because studies have found its DNA in arterial plaque.[17] Another thought is that H. pylori infection results in indirect effects related to chronic inflammation, whereby long-term inflammation raises cytokine levels in the bloodstream.[18] Thus, H. pylori might serve as a trigger by starting the inflammatory cascade. Further studies suggest that H. pylori may induce platelet aggregation, and thereby play a role in the acute phase of IHD.[19] A recent meta-analysis indicates that infection with certain more virulent strains of H. pylori may provoke an intense immune response and precipitate coronary events. [20] Virus-related CVD Several viruses have been shown to affect the heart. These include the adenoviruses, Coxsackie viruses, hepatitis A virus, and herpes simplex viruses. Adenoviruses include multiple serotypes. These viruses are a major cause of acute respiratory infections, conjunctivitis, and other illnesses. The adenoviruses can cause myocarditis, but do not appear to have a role in CVD.[21] Coxsackie viruses are enteroviruses most commonly associated with hand, foot, and mouth disease. The Coxsackie B viruses are known to cause myocarditis, but the relationship to CVD is unconfirmed. A herpes virus known as Marek's disease virus (MDV) causes a variety of illnesses including lymphoma in its natural host, the chicken. MDV has been recognized for some time as a causal agent for atherosclerosis in chickens, much like that seen in humans.[22] In a study of 391 patients referred for chest pain or other evidence of myocardial ischemia, Zhu et al[23] found that 52% of the patients had IgG antibodies for hepatitis A virus (HAV). The actual prevalence of coronary artery disease was 74% in the patients who were HAV seropositive and 52% in the patients who were HAV seronegative (P < 0.0001). The association remained significant after controlling for other cardiovascular risk factors, including other infectious agents. The authors concluded that HAV might contribute to CAD by eliciting a chronic inflammatory response. While this study established an association, it did not establish causality. Herpes simplex virus 1 (HSV1) and herpes simplex virus 2 (HSV2) have been found in human atherosclerotic plaque.[24, 25] Cytomegalovirus (CMV), a member of the herpes virus family, can infect individuals but does not cause signs and symptoms. Studies have shown both positive[26–28] and negative[29] associations of CMV with coronary artery disease. In summary, several organisms have a potential causative role in the subsequent development of CVD (Table 1). The role of viruses and H. pylori in CVD is not conclusive. Whether viruses and H. pylori act directly in coronary vessels or indirectly, with infection stimulating an immune response, is not clear. Future studies are needed to provide definitive data elucidating the precise role and mechanisms that viruses and H. pylori play. However, there is a strong association between C. pneumoniae and CVD. Table 1. Micro-Organisms With a Potentially Causative Role in the Development of CVD Bacteria Viruses Chlamydia pneumoniae Cytomegalovirus Helicobacter pylori Herpes simplex virus Borrelia burgdorferi Hepatitis A virus Multiple Organisms Periodontitis Treponema pallidum The Role of Antibiotics in Prevention and Treatment Because substantial data exist associating C. pneumoniae with cardiovascular disease, studies over the past decade have begun to focus on the possible benefits of antibiotics in treatment. A number of clinical trials have been done in an attempt to determine whether antibiotics might play a role in the primary prevention of cardiac events or in secondary prevention once a cardiac event has occurred. The presence of C. pneumoniae in atheromatous plaques of humans and coronary events in patients with elevated titers of antibodies to C. pneumoniae have prompted researchers to question whether antibiotic therapy aimed at C. pneumoniae could prevent or attenuate the risk of cardiac events. Data from studies of the use of antibiotics for atherosclerotic disease in animal models support this hypothesis.[30, 31] These studies showed that if antibiotic therapy was given early after inoculation of animals with C. pneumoniae, atherosclerosis could be prevented or its progression slowed; antibiotics given later in the process had a little or no effect on progression. The best treatment for eradicating C. pneumoniae is uncertain at this time. Studies are needed to determine the level of drug needed to penetrate infected tissue, because C. pneumoniae can be found inside fatty plaque within the arteries. C. pneumoniae is sensitive to a number of antibiotics. Macrolides (azithromycin, clarithromycin), tetracyclines (tetracycline, doxycycline, and minocycline), fluoroquinolones (ofloxacin, levofloxacin, and gatifloxacin), and anti-tuberculars (rifapentine and rifampin) are known to be effective against this bacterium.[32] The antineoplastic antibiotics classified as ansamycins are also highly effective.[33] The sulfonamides, penicillins, and cephalosporins are not effective against C. pneumoniae. The early studies in humans seemed to indicate that prophylactic antibiotics might lead to reductions in secondary cardiovascular events in patients with stable coronary heart disease and those with acute coronary syndrome (ACS). The ROXIS (Roxithromycin in Ischemic Syndromes) trial was the first randomized pilot study of an antibiotic to be done in patients with acute coronary syndrome. Gurfinkel et al[34] randomized 202 patients with unstable angina or non-Q wave MI to placebo or 150 mg oral roxithromycin twice daily for 30 days. They found a statistically significant difference between the placebo and treatment group after short-term treatment. Gupta et al[35] studied men post myocardial infarction and stratified them into 3 groups based on level of IgG antibodies to C. pneumoniae. Subjects received either placebo or azithromycin 500 mg/day for 3 days or 2 courses of azithromycin 3 months apart. Subjects in the placebo group who had the highest antibody titers had an approximately 4-fold increased risk of developing recurrent cardiac ischemia compared to subjects without elevated titers. Subjects in the highest antibody titer group who were treated with azithromycin did not have an elevated risk of developing recurrent ischemia. Subjects receiving 1 and 2 courses of antibiotics had similar results. Muhlestein et al[36] initiated a secondary prevention trial of azithromycin in patients with coronary disease and serological evidence of C. pneumoniae. The ACADEMIC (Azithromycin in Coronary Artery Disease: Elimination of Myocardial Infection with Chlamydia) trial examined markers of inflammation and cardiovascular events in 302 patients. Subjects were randomized to either placebo for 3 months or a 3-month course of azithromycin (500 mg/day for 3 days and then weekly). They found no differences between groups for adverse ischemic cardiac events, but the group receiving azithromycin had significantly lower inflammation markers of interleukin-6 and C-reactive protein when compared to the placebo group. The findings of these 2 early studies led researchers to think that the newer macrolides might have an effect on cardiac clinical outcomes or inflammatory markers or possibly have an effect on both. The question that evolved from these early studies was whether the drugs were effective because they eradicated C. pneumoniae or if the beneficial outcomes were due to antiinflammatory properties, because macrolides have anti-inflammatory effects. It was hypothesized that macrolides might subdue inflammation and stabilize atheromatous plaque (preventing rupture and vessel occlusion), which could partially explain some of the benefits in trials involving patients with acute coronary syndrome.[37] Noting that the studies focusing on secondary prevention of cardiac events showed promise, researchers in the late 1990s began to address the question of whether antibiotics could play a role in primary prevention of CVD. Two major studies were conducted that involved large retrospective analyses to determine whether exposure to antibiotics might alter the risk for developing acute MI. Meier et al[38] examined the medical records of 3315 patients who had an acute MI (first occurrence and no previously documented risk factors) and compared them to records of 13,139 controls matched for age, sex, calendar year, and physician practice group. Records were reviewed for documentation of prescription of an antibiotic in the 3-year period preceding the acute MI and for corresponding dates in control subjects. They found a statistically significant difference in the proportion of controls and MI patients taking tetracyclines and quinolones in the 3 years preceding their MI. No differences were seen among groups taking macrolides, sulfonamides, penicillins, or cephalosporins when compared to controls. Daily users of a regular dose of tetracycline, those taking higher doses, those taking 1 or 2 prescriptions of a macrolide in the 3 years prior to MI, and those with 3 or more prescriptions in the 3-year period also had a lower risk of developing MI. The second retrospective study examined 1796 cases of patients with MI (who had previous risk factors for cardiac disease) and compared them with 4882 controls.[39] Researchers documented doxycycline, tetracycline, and erythromycin prescriptions during the 5-year period pre-MI. Unlike the previous study, they found no differences between groups in terms of the percentage experiencing an acute MI. The problem with both the aforementioned studies is that due to the retrospective designs employed, both the positive and negative findings may have been the result of other variables or due to chance. Large randomized clinical trials were needed to determine whether antibiotics could play a role in secondary prevention of cardiovascular events in patients with known CVD. The WIZARD (Weekly Intervention with Zithromax for Atherosclerosis and its Related Disorders) trial enrolled 7724 stable subjects with previous MI and who were seropositive for C. pneumonia.[40] Subjects were randomized to placebo or 3 months treatment with azithromycin at 600 mg/week. Primary end points were a composite of death, MI, hospitalization for unstable angina, or need for repeat revascularization at 3 years. There was only a 7% nonsignificant reduction in the end point in the group receiving azithromycin. Further analyses, however, showed a possible benefit during and shortly after treatment, with a 33% reduction in death or MI at 6 months (P = 0.03). This finding led researchers to question whether a longer period of antibiotics might prevent future coronary events. Another trial, called STAMINA (South Thames Trial of Antibiotics in Myocardial Infarction and Unstable Angina), randomized 325 subjects to a placebo group or 1 of 2 different treatment groups: azithromycin 500 mg/day plus omeprazole 20 mg and metronidazole 400 mg twice daily (for Helicobacter); or amoxicillin 500 mg twice daily plus omeprazole 20 mg and metronidazole 400 mg twice daily. [41] Subjects were followed for 1 year. There were no significant differences among groups for major cardiac events. Yet, when the researchers combined the 2 groups receiving antibiotics and compared them to the placebo group, there were 36% fewer adverse cardiac events at 12 weeks (P = 0.02); the difference continued at 1 year. Seropositivity to C. pneumoniae or H. pylori had no effect on outcomes, so the question again arose as to whether the main factors affecting outcomes were related to the anti-inflammatory properties of the drugs, rather than their antimicrobial properties. A large-scale well-designed trial, PROVE-IT (Pravastain or Atorvastatin Evaluation and Infection Therapy), enrolled 4162 patients hospitalized with acute coronary syndrome and high cholesterol levels.[42] In a double-blind, randomized placebo-controlled design, patients received either 400 mg of gatifloxacin daily for 2 weeks followed by a 10-day course of gatifloxacin every month, or placebo. The mean duration of follow-up was 2 years. Long-term treatment with this bactericidal antibiotic had no effect on reducing cardiovascular events. In a more recent large-scale trial called the CLARICOR study, patients with stable coronary disease were randomized to a 2-week course of clarithromycin 500 mg daily or placebo.[43] There were no differences between groups for the combined end point of cardiac mortality, MI, and unstable angina; however, the group receiving clarithromycin had a significantly higher cardiovascular mortality rate, a very unexpected finding. In view of the conflicting results of antibiotic trials in patients with CVD, several researchers have conducted meta-analyses in an effort to shed light on the question of efficacy of antibiotics in preventing cardiac events. A meta-analysis of studies that used antibiotics effective against C. pneumoniae was conducted by Wells et al.[44] Only randomized controlled trials were included. Nine studies with a total of 11,015 participants met the inclusion criteria. Four studies reported a benefit from antibiotics, while 5 studies found no benefit from antibiotics in the prevention of cardiovascular events in subjects with known ischemic heart disease. The most conclusive results are from a large meta-analysis of studies of antibiotics in patients with coronary disease.[45] These authors searched Medline and the Cochrane Central Register of Controlled Trials for studies that were prospective, randomized, placebo-controlled trials of antibiotic therapy for C. pneumoniae in patients with coronary artery disease. The 11 studies that met pre-established criteria and were included in the review enrolled 19,217 patients and reported all-cause mortality, myocardial infarction, or unstable angina. This meta-analysis documented that the currently available evidence does not show an overall benefit of antibiotics in reducing cardiovascular events or mortality. Despite disappointing results to date, research continues on the topic of antibiotic therapy for C. pneumoniae. A new class of antibiotics, ansamycins, show promise for future studies. One of these ansamycins, benzoxazinorifamycin (marketed as Rifalazil, currently not available in the United States), is 10 to 1000 times more effective against C. pneumoniae than azithromycin.[33] There is currently a multicenter, randomized, placebocontrolled study to determine the effects of weekly Rifalazil given over 12 weeks to patients seropositive for C. pneumoniae.[46] Results are expected later this year. At this time, the available evidence does not support the use of antibiotics for primary or secondary prevention of CVD. Nurse practitioners should continue to work collaboratively with patients to implement interventions that target known risks for CVD including controlling hypertension, treating dyslipidemias, maintaining target blood glucose in diabetics, eliminating smoking, controlling weight, and increasing physical activity. Primary and Secondary Prevention Multiple complex processes are involved in the development of CVD. Currently, no specific guidelines exist for general preventive measures related to infectious diseases as a specific causal factor. Indeed, some authors still debate the sequence of events, and question whether chronic inflammation might predispose some individuals to infection rather than vice versa. However, several general mechanisms known to have a role in atherogenesis may provide clues to the possibility of developing primary or secondary preventive measures in the future (Table 2). Table 2. Considerations for Primary and Secondary Prevention Condition Patients with chronic conditions (SLE, RA) Considerations For Prevention inflammatory Close monitoring of other risk factors, control of inflammation associated with chronic disease Existing periodontal disease Offer definitive dental care Chlamydia pneumoniae infection Early treatment with antibiotics Control of risks associated with exposure to numerous ubiquitous Support healthy immune system infectious agents in environment Patients with existing cardiovascular Patient education risk factors lifestyle modification regarding risk, High risk for exposure to infectious Offer immunization if available diseases Other infectious diseases Early treatment to prevent chronic colonization It is known that systemic inflammation is a factor in the development of atherosclerosis. In addition, patients with significant systemic autoimmune diseases have a higher risk and prevalence of CVD. Observational research has linked CVD with autoimmune diseases such as SLE and RA. Both CVD and autoimmune diseases involve immune system activation and endothelial dysfunction. HMG-CoA reductase inhibitors, also known as statins, are now thought to be useful in modulating inflammatory pathways, as well as lowing cholesterol levels.[47] Thus, statins have potential for use in the reduction of chronic systemic inflammation. Multiple oral pathogens are involved in the development of periodontal disease. These pathogens have been shown in some studies to be linked to subsequent development of CVD. The prevention of periodontal disease through regular dental care is an important area for future research. However, many barriers to the establishment of a dental home exist in the United States, including statutory restrictions limiting provider availability, lack of a supply of pediatric dentists to provide early dental care to children, and the unaffordability of dental care related to the aforementioned statutory restrictions. However, inroads are being made with such programs as the fluoride varnish program, which provides reimbursement for ARNPs, PAs, and MDs in some states for performing this type of primary dental care. Many of the bacterial and viral microbes implicated in the development of CVD are ubiquitous. Therefore, general measures to support a healthy immune system seem prudent, and the ARNP plays a significant role in informing patients and educating them about methods to prevent long-term sequelae of basic lifestyle choices such as rest, nutrition, exercise, hygiene, prevention of exposure to infectious organisms, and avoidance of tobacco use and excessive alcohol use that may impede normal immune system function. Early treatment of infectious diseases to avoid chronic colonization and thus inflammation should also be emphasized. Conclusions and Implications for Practitioners While studies have documented a role of various infectious organisms in the subsequent development of CVD for 2 decades, few steps have been taken to address the role of prevention from these risk factors. This gap between research and practice may be causing significant morbidity and mortality in the United States and other developed countries. Providers should consider several questions in attempting to bridge this gap. One obvious question concerns oral health screening. Should we be screening for periodontitis or other dental diseases in those with other risk factors for CVD? At least one author, Lowe,[48] has recommended a Dental Health Score be used. It seems reasonable for ARNPs to conduct a dental screen during wellness visits and refer clients for decay and other abnormalities. Practitioners can also advocate for greater availability of community dental services. Another question concerns the role of antibiotic use. Antibiotic prophylaxis is indicated for a subset of patients with valvular heart disease, such as those with artificial heart valves. Should some type of antibiotic prophylaxis be recommended in high-risk CVD patients, or at a minimum, those with a previous CVD event? Currently, there is no consistent evidence supporting this, and clinicians should keep in mind the risks of over-prescribing antibiotics. A final consideration is the cost of implementing these or other preventive measures. This cost must be measured against the direct costs of providing tertiary care as well as pain and suffering for someone with a serious cardiovascular event. At a minimum, primary care providers can start with patient education to share these known links and make patients aware that several self-care steps can be taken with regard to these additional measures to avoid much more devastating health care problems in the future. References 1. Mattila KJ, Nieminen MS, Valtonen VV, et al. Association between dental health and acute myocardial infarction. Br Med J. 1989;298:779–781. 2. Loesche WJ. Microbiology of dental decay and periodontal disease. In: Baron editors. Medical microbiology. 4th ed. [online text]. Galveston, TX: The University of Texas Medical Branch at Galveston; 1996. 3. Genco R, Offenbacher S, Beck J. Periodontal disease and cardiovascular disease: epidemiology and possible mechanisms. J Am Dent Assoc. 2002;133:14S–22S. 4. DeStefano F, Anda R, Kahn H, et al. Dental disease and risk of coronary heart disease and mortality. Br Med J. 1993;306:688–691. 5. Beck J, Garcia R, Heiss G, et al. Periodontal disease and cardiovascular disease. J Periodontol. 1996;67:1123–1137. 6. Wu T, Trevisan M, Genco R, et al. Examination of the relation between periodontal health status and cardiovascular risk factors: serum total and high density lipoprotein cholesterol, C-reactive protein, and plasma fibrinogen. Am J Epidemiol. 2000;151(3):273–282. 7. Glurich I, Grossi S, Albini B, et al. Systemic inflammation in cardiovascular and periodontal disease: comparative study. Clin Diagn Lab Immunol. 2002;3:425–432. 8. Haraszthy V, Zambon J, Trevisan M, et al. Identification of periodontal pathogens in atheromatous plaques. J Periodontol. 2000;71:1554–1560. 9. Chong P, Kezele B. Periodontal disease and atherosclerotic cardiovascular disease: confounding effects or epiphenomenon?. Pharmacotherapy. 2000;20(7):805–818. 10. Centers for Disease Control and Prevention. Chlamydia pneumoniae. Disease listing, October 6, 2005. Available at: www.cdc.gov/ncidod/DBMD/diseaseinfo/chlamydiapneumonia_t.htm Last accessed July 21, 2008. 11. Campbell L, Kuo C, Grayston J. Chlamydia pneumoniae and cardiovascular disease. Emerging Infect Dis. Available at: http://www.cdc.gov/ncidod/EiD/vol4no4/Campbell.htm Accessed July 26, 2008. 12. Saikku P, Leinonen M, Mattila K, et al. Serological evidence of an association of a novel chlamydia, TWAR, with chronic coronary heart disease and acute myocardial infarction. Lancet. 1988;2:983–986. 13. Larsen M, Moern B, Fuller A, et al. Chlamydia pneumoniae and cardiovascular disease. Med J Austral. 2002;177(10):558–562. 14. Arcari C, Gaydos C, Nieto F, et al. Association between Chlamydia pneumoniae and acute myocardial infarction in young men in the united states military: the importance of timing of exposure measurement. Clin Infect Dis. 2005;40:1123–1132. 15. Ewald P, Cochran G. Chlamydia pneumoniae and cardiovascular disease: an evolutionary perspective on infectious causation and antibiotic treatment. J Infect Dis. 2000;181(Suppl 3):394–401. 16. Leinonen M. Chlamydia pneumoniae and other risk factors for atherosclerosis. J Infect Dis. 2000;181(Suppl):S414–S416. 17. Pellicano R, Peyre S, Astegiano M, Oliaro E, Fagoonee S, Rizzetto M. Updated review (2006) on Helicobacter pylori as a potential target for the therapy of ischemic heart disease. Panminerva Med. 2006;48(4):241– 246. 18. Manolakis A, Kapsoritakis A, Potamianos S. A review of the postulated mechanisms concerning the association of Helicobacter pylori with ischemic heart disease. Helicobacter. 2007;12(4):287–297. 19. Berrutti M, Pellicano R, Fagoonee S, et al. Potential relationship between Helicobacter phylori and ischaemic heart disease: any pathogenic model?. Panminerva Med. 2008;50(20):161–163. 20. Franceschi F, Niccoli G, Ferrante G, et al. CagA antigen of Helicobacter pylori and coronary instability: insight from a clinico-pathological study and a meta-analysis of 4241 cases. Atherosclerosis. 2008; July 1; Available at: http://www.ncbi.nlm.nih.gov.esearch.ut.edu/pubmed/18599062 Last accessed August 1, 2008. 21. Leinonen M, Saiku P. Evidence for infectious agents in cardiovascular disease and atherosclerosis. Lancet. 2002;2:11–17. 22. Minick C, Fabricant C, Fabricant J, et al. Atheroarteriosclerosis induced by infection with a herpesvirus. Am J Pathol. 1979;96(3):673–706. 23. Zhu J, Quyyumi A, Norma J, et al. The possible role of hepatitis A virus in the pathogenesis of atherosclerosis. J Infect Dis. 2000;182(6):1583– 1587. 24. Gyorkey F, Melnick J, Guinn G, et al. Herpes viridae in the endothelial and smooth muscle cells of the proximal aorta of atherosclerotic patients. Exp Mol Pathol. 1984;40(3):328–339. 25. Nicholson A, Hajjar D. Herpesvirus in atherosclerosis and thrombosis: etiologic agents or ubiquitous bystanders?. Arterioscl Thromb Vasc Biol. 1998;18(3):339–349. 26. Zhu J, Shearer G, Norma J, et al. Host response to cytomegalovirus infection as a determinant of susceptibility to coronary artery disease: sex-based difference in inflammation and type of immune response. Circulation. 2000;102(20):2491–2496. 27. Eryol N, Kilic H, Gul A, et al. Are the high levels of cytomegalovirus antibodies a determinant in the development of coronary artery disease?. Int Heart J. 2005;46(2):205–209. 28. Gredmark S, Jonasseon L, Van Gosliga D, et al. Active cytomegalovirus replication in patients with coronary disease. Scand Cardiovasc J. 2007;41(4):230–234. 29. Rothenbacher D, Hoffmeister A, Bode D, et al. Cytomegalovirus infection and coronary heart disease: results of a German case-control study. Infect Dis. 1999;179(3):690–692. 30. Muhlestein J, Anderson J, Hammond E, et al. Infection with Chlamydia pneumoniae accelerates the development of atherosclerosis and treatment with azithromycin prevents it in a rabbit model. Circulation. 1998;97(7):633–636. 31. Fong IW, Chiu B, Viira E, Fong MW, Jang D, Mahony J. Rabbit model for Chlamydia pneumoniae infection. J Clin Microbiol. 1997;35(1):48–52. 32. Gieffers J, Solbach W, Maass M. In vitro sucseptibility of Chlamydia pneumoniae cardiovascular strains from coronary artery endothelium and smooth muscle cells. Cardiovasc Drug Ther. 2001;15(3):259–262. 33. Fujii K, Saito H, Tomioka H, Mae T, Hosoe K. Mechanism of action of antimycobacterial activity of the new benzoxazinorifamycin KRM-1648. Antimicrob Agents Chemother. 1995;39(7):1489–1492. 34. Gurfinkel E, Bozovich G, Daroca A, et al. Randomised trial of roxithromycin in non-Q-wave coronary syndromes: ROXIS pilot study. Lancet. 1997;350(9083):404–407. 35. Gupta S, Leatham E, Carrington D, et al. Elevated Chlamydia pneumoniae antibodies, cardiovascular events, and azithromycin in male survivors of myocardial infarction. Circulation. 1997;96(2):404–407. 36. Muhlestein J, Anderson J, Carlquist J, et al. Randomized secondary prevention trial of azithromycin in patients with coronary artery disease: primary clinical results of the ACADEMIC study. Circulation. 2002;102(15):1755–1760. 37. Higgins J. Chlamydia pneumoniae and coronary artery disease: the antibiotic trials. Mayo Clin Proc. 2003;78(3):321–332. 38. Meier C, Derby L, Jick S, et al. Antibiotics and risk of subsequent firsttime acute myocardial infarction. JAMA. 1999;281(5):427–431. 39. Jackson L, Smith N, Heckbert S, et al. Lack of association between first myocardial infarction and past use of erythromycin, tetracycline, or doxycycline. Emerging Infect Dis. 1999;5(2):281–284. 40. O'Connor C, Dunne M, Pfeffer M, et al. Azithromycin for the secondary prevention of coronary heart disease events: the WIZARD study: a randomized controlled trial. JAMA. 2003;290(11):1459–1466. 41. Stone A, Mendall M, Kaski J-C, et al. Effect of treatment for Chlamydia pneumoniae and Helicobacter pylori on markers of inflammation and cardiac events in patients with acute coronary syndromes: South Thames Trial of Antibiotics in Myocardial Infarction and Unstable Angina (STAMINA). Circulation. 2002;106(10):1219–1223. 42. Cannon CP, Braunwald E, McCabe CH, et al. Antibiotic treatment of Chlamydia pneumoniae after acute coronary syndrome. N Engl J Med. 2005;352(16):1646–1654. 43. Jespersen C, Als-Nielsen B, Damgaard M, et al. Randomised placebo controlled multicentre trial to assess short term clarithromycin for patients with stable coronary heart disease: CLARICOR trial. Br Med J. 2006;332(7532):22–27. 44. Wells BJ, Mainous AG, Dickerson LM. Antibiotics for the secondary prevention of ischemic heart disease: a meta-analysis of randomized controlled trials. Arch Intern Med. 2004;164(19):2156–2161. 45. Andraws R, Berger JS, Brown DL. Effects of antibiotic therapy on outcomes of patients with coronary artery disease: a meta-analysis of randomized controlled trials. JAMA. 2005;293:2641–2647. 46. Watson C, Alp NJ. Role of Chlamydia pneumoniae in atherosclerosis. Clin Sci. 2008;114:509–531. 47. Abou-Raya A, Abou-Raya S. Inflammation: a pivotal link between autoimmune diseases and atherosclerosis. Autoimmun Rev. 2006;5:331–337. Available from www.sciencedirect.com. Accessed April 5, 2008. 48. Lowe G. Dental disease, coronary heart disease and stroke, and inflammatory markers: what are the associations, and what do they mean?. Circulation. 2004;109:1076–1078.