* Your assessment is very important for improving the workof artificial intelligence, which forms the content of this project
Download microbiology exam ii - Medical Mastermind Community
Marine microorganism wikipedia , lookup
Schistosomiasis wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Carbapenem-resistant enterobacteriaceae wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Gastroenteritis wikipedia , lookup
Urinary tract infection wikipedia , lookup
Triclocarban wikipedia , lookup
Anaerobic infection wikipedia , lookup
Neonatal infection wikipedia , lookup
Human microbiota wikipedia , lookup
Infection control wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
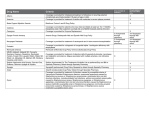
MICROBIOLOGY EXAM II SIMPLE COMPLETIONS Give the BEST answer for the following questions: 1. A Gram stain prepared from an inoculum of S. aureus is overdecolorized. After the completion of the Gram stain procedure, the resulting smear will show: A. Purple cocci -in chains B. Purple cocci in clusters C. Red cocci in clusters D. Red bacilli E. Red cocci in chains 2. Salmonella is easily recognized in the laboratory for its ability to produce on TSI medium. A. Indole B. Urease C. H2S D. Lactose E. Citrate The following clinical specimen has to be sent to the laboratory for immediate processing: A. Blood B. CSF C. Hair samples D. Stool E. Urine 4. A sputum exudate reveals lancet-shaped, gram-positive cocci arranged. in pairs. This morphology is characteristic of: A. Streptococcus pyogenes B. Staphylococcus epidermidis C. Streptococcus pneumoniae D. Klebsiella pneumoniae E. Enterococcus faecalis 5. The ability to clot blood plasma (coagulase +) is one of the most reliable laboratory criteria available for the identification of: A. Escherichia coli B. Streptococcus pyogenes C. Staphylococcus aureus D. Haemophilus influenzae E. Streptococcus agalactiae Page 1 6. The inhibition of growth of alpha-hemolytic colonies by optochin (P disc) provides an excellent screening tool in the identification of: A. Staphylococci B. Meningococci C. Streptococci D. Pneumococci D. Peptococci QUESTIONS 7 AND 8 You are a resident on call at the Emergency room. Your male patient has an urethral purulent discharge, and you suspect gonorrhea. 7. Before collecting the specimen you request a: A. MacConkey agar plate B. Thayer-Martin agar plate C. 5% Sheep Blood agar plate D. CNA agar plate E. Phenyl-ethyl alcohol agar plate 8. The Microbiology laboratory receives your patient's specimen and performs a Gram stain on it. You expect the lab will report the finding of A. Many neutrophils and intracellular gram-negative cocci B. Many neutrophils and intracellular gram-negative rods C. Many neutrophils and gram-positive cocci in pairs D. Many neutrophils and gram-positive cocci in clusters E. No neutrophils or intracellular gram-positive cocci 9. After the heat fixation step when preparing a bacterial smear: A. Cell proteins coagulate B. Bacterial cells are fixed to the slide C. Most bacteria are killed D. All of the above are true 10. Typically, Staphylococcus aureus morphology is that of A. Gram-positive cocci in chains B. Gram positive cocci in clusters C. Gram-negative cocci in pairs D. Gram-negative cocci in clusters 11. A nonmotile, gram-negative rod, isolated from a patient's stool culture is responsible for diarrhea. The probable diagnosis is: A. Typhoid fever B. Cholera C. Staphylococcal food poisoning D. Shigellosis E. Amebiasis Page 2 12. Group A Streptococcus growing on a blood agar plate, shows which of the following: A. Alpha hemolysis, a clear zone surrounding the colonies B. Alpha hemolysis, a green zone surrounding the colonies C. Beta-hemolysis, a clear zone surrounding the colonies D. Beta-hemolysis, a green zone surrounding the colonies E. Gamma-hemolysis a clear zone surrounding the colonies 13. Colonies of Neisseria turn purple when a redox dye is applied. The color change is indicative of the activity of the enzyme: A. Beta-galactosidase B. Oxidase C. Urease D. DNase E. Lysine Decarboxylase 14. The only major category of infectious diseases with which Enterobacteriaceae members have not been definitively associated is that of: A. Urinary tract infections B. Respiratory tract infections C. Skin and soft tissue infections D. Sexually transmitted infections E. Systemic infections 15. Group D streptococci, when present, could most likely be recovered from a stool sample if the primary inoculum was streaked on: A. CNA agar B. MacConkey agar C. Xylose Lysine Decarboxylase agar D. EMB agar E. none of the above 16. The detection of the 13-lactamase enzyme is primarily valuable in infections caused by: A.Streptococcus pyogenes B. Streptococcus agalactiae C. Nocardia asteroides D. Hemophilus influenzae E. Klebsiella pneumoniae 17. You are conducting an epidemiologic survey for the detection of upper respiratory carriers of Group A. The optimal type of specimen to be obtained for culture is: A. A throat swab B. Saliva C. A buccal cavity swab D. Sputum E. None of the above Page 3 18. What is the time interval required for laboratory identification and antibiotic susceptibility testing of common, pathogenic, gram positive cocci? A. 24 hours B. 48 hours C. 72 hours D. 4 days E. 5 days 19. Once isolated in the laboratory, Staphylococcus can be easily distinguished from Streptococcus on the basis of: A. The catalase reaction B. The oxidase reaction C. The lactose fermentation reaction D. The glucose fermentation reaction E. The colony pigmentation reaction 20. A Kirby-Bauer susceptibility test, and a beta-lactamase detection test are indicated if an organism isolated from an infected wound turns out to be: A. Streptococcus agalactiae B. Streptococcus pyogenes C. Staphylococcus aureus D. Alpha-hemolytic streptococcus 21. The use of chemical agents on skin or living tissue to inhibit or eliminate microbes is known as: A. Sterilization B. Antisepsis C. Disinfection D. Pasteurization E. Cleansing 22. Which of the following will make a sputum a "Q0" specimen? A. Saliva contaminated the specimen B. The specimen did not contain enough neutrophils C. The specimen contained too many squamous cells D. All of the above statements 23. You obtain a blood specimen from a patient who is being treated with IV penicillin. Pathogenic microorganisms can still be isolated from this patient's blood cultures if. A The lab incubates the cultures longer than usual B. The cultures are incubated at a higher temperature than usual C. The cultures are shaken for one hour prior to incubation D. You alert the laboratory that the patient received antibiotics before you collected the specimens Page 4 MATCHING Match the BEST possible answer with each question. Answers can be used once, more than once, or not at all. QUESTIONS 24-28 24._____ Microorganism that grows in the presence of O2 25. _____Microorganism that grows in the absence of O2 26. _____Medium used to distinguish between bacterial species or groups. 27. _____ Medium containing substances that stimulate a single organism or groups of organisms to grow more readily. 28. _____ Medium that allows the growth of certain bacteria while inhibiting the growth of others. (A) Anaerobic (B) Selective (C) Differential (D) Enriched (E) Aerobic QUESTIONS 29-31 29. _____ Mycobacterium tuberculosis 30. _____ Encapsulated microorganisms 31. _____ Enterobacteriaceae (A) Rapid agglutination test (B) Kinyoun stain (C) India Ink (D) Bile-esculin and 6.5% salt medium (E) Carbohydrate fermentation QUESTIONS 32-36 For each diagnostic procedure, select the most appropriate laboratory result. 32. _____ Differentiation of Group D enterococci from Group D non-enterococci. 33. _____ Differentiation of Streptococcus agalactiae from other streptococci. Page 5 34. _____ Identification of S. aureus. 35. _____ Screening of pathogenic enteric gram-negative rods. 36. _____ Differentiation of Streptococcus pyogenes from other streptococci. (A) Inhibition of growth by bacitracin (B) Fermentation of lactose (C) Production of CAMP factor (D) Growth in 6.5% salt broth (E) Agglutination with anti-protein A antibodies QUESTIONS 37-49 TRUE OR FALSE Choose the best possible answer. A= True B= False 37. _____ The NEC is a determination of the least amount of an antimicrobial agent that will inhibit the growth of a microorganism in vitro. 38. _____ In the Kinyoun stain, tergitol is used to help the penetration of carbolfuchsin into the acid-fast bacteria. 39. _____ A negative coagulase test (both slide and tube methods) for an isolate of staphylococcus, alerts the physician that the organism is most likely a contaminant and can be ignored. 40. _____ Phage typing of Staphylococcus aureus is used to investigate outbreaks of impetigo. 41. _____ A sputum specimen acceptable for bacterial culture usually contains more neutrophils than squamous cells. 42. _____ Urinary tract infections are more prevalent in males. 43. _____ Differentiation among Enterobacteriaceae is based on the Gram stain. 44. _____ Clean-catch urine samples usually contain low numbers of microorganisms from skin. 45. _____ The most common clinical specimens taken from patients infected with E. coli come from the upper respiratory tract. 46. _____ In the Kirby-Bauer test, Gram-positive bacteria usually appear as resistant to Vancomycin. 47. _____ When isolated in the laboratory, Streptococcus pyogenes does not require antimicrobial susceptibility tests. 48. _____ Sterilization is the total destruction of all microorganisms, including the most resistant forms. Page 6 49. _____ A urine culture result showing 106 CFU/ml indicates a urinary tract infection. PART II - LECTURE EXAM, QUESTIONS 51-150 MATCHING: For each medium list below, select the BEST. lettered response. Answers may be used once, more than once, or not at all. QUESTIONS 50-52: A. Brucella abortus B. Brucella suis C. Brucella melitensis 50. _____Causes mild disease with rare suppurative complications. 51. _____Is associated with destructive lesions and a prolonged course of infection. 52. _____ Is the most common cause of brucellosis, causing severe disease with a high incidence of serious complications. QUESTIONS 53-56: For Legionella, A. Presumptive Identification. B. Definitive Identification. 53. _____ Demonstration of a typical colonial morphology. 54. _____ Specific staining with fluorescein-labeled antibodies. 55. _____ Gram stain showing weakly staining, pleomorphic, thin, gram-negative bacilli. 56. _____ NA hybridization tests. SIMPLE COMPLETIONS: Each of the questions or incomplete statements in this group is followed by four or five suggested answers or completions. Select the one which is BEST in each case and mark the corresponding letter on the answer sheet. 57. Which of the following factors is NOT important for establishment of meningococcal disease due to Neisseria meningitidis? A. the ability of N. meningitidis to colonize the nasopharynx. B. the production of siderophores for iron scavenging. C. systemic spread without antibody-mediated phagocytosis. Page 7 D. the expression of toxic effects mediated by lipooligosaccharide endotoxin. Questions 58-60: A patient presents with small skin lesions on the trunk and lower extremities. In some cases, these-have coalesced to form larger hemorrhagic lesions. The patient complains of an abrupt, severe headache and fever. 58. You culture the cerebrospinal fluid, expecting to find: A. gram negative cocci clustered as grapes. B. gram positive rods within phagocytes. C. gram negative diplococci associated with polymorphonuclear leukocytes. D. gram negative, comma-shaped bacilli. 59. You question the patient about close contacts, recommending that previously exposed persons: A. leave the country. B. be vaccinated. C. be examined for a purulent urethral discharge. D. Initiate prophylactic sulfonamide or rifampin therapy. 60. The bacterium responsible for the symptoms described above may also cause: A. Waterhouse-Friderichsen Syndrome. B. Toxic Shock Syndrome. C. Reye's Syndrome. D. Swimmer's Itch. 61. Legionella are able to avoid intracellular killing because: A. They multiply only extracellularly. B. They inhibit phagolysosomal fusion. C. Once they penetrate the cell by endocytosis, they immediately kill host cells by secreting proteolytic enzymes, phosphatases, lipases, and nucleases. D. Humoral immunity, not cellular immunity, is the principle host defense response. 62. Among renal transplant and adult cancer patients, Listeria monocytogenes is the leading cause of: A. tonsillitis B. otitis media C. conjunctivitis D. sinusitis E. bacteria meningitis 63. Recovery from and immunity to listeriosis depend on the development of: A. an effective IgG response by the host. B. an effective IgA response by the host. C. an effective IgM response by the host. D. an effective cell-mediated immune response by the host. E. an effective humoral and cell-mediated immune response by the host. Page 8 64. The treatment of the disease tuberculosis: A. is initiated with a single first-line chemotherapeutic agent. B. usually requires prolonged bed rest and surgery. C. in adults should be continued until the tuberculin test reverts to negative. D. always results in negative sputum cultures and clinical cure within 3 weeks. E. always necessitates the use of combined drug therapy. 65. Which of the following species synthesizes a bacterial protein with adenylate cyclase activity, which plays a role in pathogenesis? A. Bordetella- pertussis B. Bacillus anthracis C. Vibrio cholerae D. a and b E. b and c 66. Which of the following organisms is incorrectly matched with the disease it most commonly causes? A. Viridans streptococci - endocarditis B. Staphylococcus- saprophyticus - urinary tract infections C. Streptococcus pyogenes - pharyngitis D. Enterococcus faecalis - neonatal meningitis 67. Which of the following organisms when isolated in the blood requires the synergistic activity of penicillin plus an aminoglycoside for appropriate therapy? A. Streptococcus pyogenes B. Enterococcus faecalis C. Staphylococcus aureus D. Streptococcus pneumoniae 68. Which of the following has/have little, if any, activity against gram-negative bacteria? A. ampicillin B. arninoglycosides C. cephalosporins D. oxacillin 69. Resistance to which of the following is caused by a "by-pass" mechanism (that is, the synthesis of an alternative target site)? A. gentamicin B. rifampin C. vancomycin D. ciprofloxacin Page 9 70. Which of the following are causes of inheritable mutations in bacteria? A. Mistakes during translation of mRNA. B. Mistakes during DNA replication. C. Mistakes during transcription of mRNA. D. All of the above. E. None of the above. 71. Which of the following is/are genotypic, not phenotypic, properties? A. Aerotolerance. B. Spore formation. C. Chromosomal G+C content of different bacterial species. D. Cellular staining characteristics in the light microscope. E. Colony morphology. 72. The process by which bacteriophage P1 packages random phage-genome-sized pieces into phage heads and thereby allows transfer of pieces of the bacterial chromosomal DNA between bacteria is called: A. Generalized transduction. B. Nongeneral transposition. C. Specialized transduction. D. High-frequency recombination. E. Reverse conjugation. 73. Transformation is important in bacterial pathogenicity because: A. It allows uptake of DNA that can homologously recombine into the bacterial chromosome and change virulence characteristics. B. It kills recipient cells and prevents future cell invasion. C. It enhances site-specific recombination that turns on virulence factor genes. D. It causes transpositions to occur at high frequency that can kill virulent bacteria. 74. Bacterial cell membranes are primarily composed of: A. lipids and proteins B. phospholipids and proteins C. lipids and carbohydrates D. phospholipids and carbohydrates E. none of the above 75. A virulence factor for Helicobacter pylori in the causation of ulcers is the enzyme urease, which may help to neutralize the HCl at a localized region of bacterial attachment to the gastric mucosa. Which metal would most likely be important in enhancing the activity of this virulence factor? A. Fe B. Ni C. Zn D. Na E. Ca Page 10 76. A heterotroph as applied to bacteria is one in which: A. organic nitrogen is the sole source of nitrogen B. vitamins must be provided externally in the growth medium C. organic carbon is the sole source of carbon D. complex carbohydrates are essential to cell survival E. all of the above 77. The proton motive force, pmf, has as a component the: A. Na+ concentration inside the cell versus that outside the cell B. difference in pH outside the cell versus that inside the cell C. K+ concentration outside the cell versus that inside the cell D. Ca2+ concentration inside the cell versus that outside the cell E. none of the above 78. A first-year student develops a "boil" in his nose. Which ONE of the following is not a true statement (which one is false)? A. It The student should receive antibiotics. B. Blood cultures are nearly always positive in the condition. C. The causative organism is probably Staphylococcus aureus. D. A nose culture is not needed to make the diagnosis. E. The proximity of the infection to the brain is a concern. 79. A 70-year-old woman with diverticulitis develops fever and pain in the left lower abdominal quadrant. A CT scan reveals a well localized intra-abdominal abscess. Which of the following are likely to be causing the abscess? A. Clostridium difficile and Streptococcus pneumoniae B. Klebsiella pneumoniae and Staphylococcus aureus C. Bacteroides fragilis and Escherichia coli D. Neisseria gonorrhoeae and Chlamydia trachomatis E. Staphylococcus aureus and Candida albicans 80. Which ONE of the following is the most pathogenic species? A. Anaerobic streptococcus B. Shigella sonnei C. Bacillus spp. D. Staphylococcus faecalis E. Candida albicans 81. Which ONE of the following is an antiphagocytic virulence property of E. coli important in neonatal (newborn) meningitis? A. Spreading factors (e.g., collagenase) B. M protein C. 140 megadalton invasion plasmid D. KI antigen E. Colonization factor antigen Page 11 82. The disease Rocky Mountain Spotted Fever is: A. confined to the northern Rocky Mountain region in the United States B. often diagnosed by a classic rash beginning on the wrists and ankles, quickly spreading to the trunk, and involving the palms and soles C. transmitted by the rat flea D. treated with penicillin plus supportive care 83. General characteristics of rickettsia include which of the following? A. A life cycle involving extracellular replication but cyst formation within eukaryotic cells B. rapid (24-48 hours) culture from clinical specimens on routine sheep blood agar C. single gram positive cocci surrounded by a capsule visualized in tissue specimens D. except for Rochalimaea/Bartonella, entry into cells by endocytosis with replication in the cytoplasm or in vacuoles in eukaryotic cells 84. The etiologic agent of epidemic typhus (louse-borne typhus) is: A. Coxiella burnetii B. Rickettsia typhi C. Rickettsia akari D. Rickettsia prowazekii 85. Although rickettsial infections are often diagnosed clinically, confirmation of the diagnosis is usually by: A. serology B. culture of the organism from blood samples C. culture of the organism from endothelial cells D. PCR (polymerase chain reaction) of circulating blood cells 86. Q fever is a disease which is: A. diagnosed primarily in large urban cities in the northeastern United States B. usually transmitted by inhalation or ingestion of organisms, not by a vector C. manifested by a characteristic rash with vesicles (blisters) beginning on the face and spreading to the trunk D. caused by Rochalimaea/Bartonella henselae 87. Characteristics of mycoplasma and ureaplasma include: A. the presence of a thin gram positive-like cell wall with no cell membrane B. rapid growth on MacConkey's agar, slow growth on basic nutrient agar C. the presence of only a cell membrane with no cell wall D. rapid growth on MacConkey's medium routine blood agar plates 88. Endotoxin: A. is produced by Gram-positive bacteria. B. has profound biological effects due to the Lipid A moiety. C. has important enzymatic activities. D. is composed of protein. E. is usually found in secreted rather than cell-associated form. Page 12 89. Endospore formation is a property of: A. Escherichia soli B. Staphylococcus aureus C. Clostridium botulinum D. Treponema pallidum E. Mycobacterium tuberculosis 90. The protective vaccine against Hemophilus influenzae is derived from this organism's: A. Pili B. Fimbriae C. Capsule D. Cell wall E. Cell membrane 91. Of the following age groups, meningitis due to H. influenzae type B occurs more frequently in: A. Neonates B. Children under 6 years of age C. Adolescents D. Adults under 60 years of age E. Adults over 60 years of age 92. Regarding the paroxysmal stage of pertussis: A. It begins with coryza, sneezing and diarrhea. B. It is characterized by a violent, repetitive cough. C. It lasts for less than a week. D. The bronchial epithelium is normal during this stage. E. There is no sign of hypersensitivity to the proteins of the bacteria. 93. Which of the following does NOT apply to the endotoxin of the enteric organisms? A. derives from 0-antigen B. derives from lipid A C. pyrogenic in humans D. secreted by many different Enterobacteriaceae members 94. Which Escherichia coli type is commonly associated with chronic diarrhea in infants and nursery outbreaks in the United States? A. Enterohemorrhagic E. coli, EHEC B. Enteropathogenic E. coli, SPEC C. Enteroaggregative E. coli, EAggEC D. Enterotoxigenic E. coli, ETEC E. Enteroinvasive E. coli, EIEC Page 13 95. Which Escherichia coli type is most like Shigella in its virulence plasmid and mode of infection: A. EHEC B. EPEC C. EAggEC D. ETEC E, EIEC 96. Which organism is most likely to be isolated from septicemic blood? A. EAggEC B. Shigella flexnerii C. EIEC D. Salmonella enteriditis 97. Which of the following species, among Enterobacteriaceae, is the most common cause of urinary tract infection? A. Escherichia coli B. Salmonella typhimurium C. Salmonella typhi D. Shigella sonnei 98. Hemolytic uremic syndrome is a sequela to infection with which type of E. coli? A. ETEC B. EHEC C. EIEC D. EPEC E. all of the above 99. Zoonotic infections are those that humans acquire from non-human animals. Which of the following is most associated with zoonotic infections? A. ETEC B. Chlamydia trachomatis C. Yersinia pestis D. Shigella flexneri 100. Klebsiella pneumoniae exhibits which distinguishing virulence characteristic? A. abscess formation B. the presence of a capsule C. a characteristic toxin D. strongly invasive property 101. Generally, Enterobacteriaceae DO NOT exhibit: A. motility B. nitrate reductase C. gram-negative bacilli D. cytochrome oxidase Page 14 E. glucose fermentation 102. Healthy adult travelers visiting Peru are cautioned against eating uncooked vegetables and unpeeled fruits, and against drinking unbottled water. However, they are already resistant to cholera because of: A. a gastric barrier, due to stomach acids. B. the gamma globulin shots they received before their trip. C. their ability to avoid contaminated food due to its acidic smell. D. their consumption of large prophylactic amounts of bicarbonates. Questions 103-104: The mayor of a small Gulf Coast town called the local hospital microbiology lab and asked for an identification of the infectious agent that was causing an outbreak of gastroenteritis in the town. A rumor has been spreading of a cholera epidemic and everyone is worried about its effect on the local economy, which is based on tourism. 103. The microbiologist is aware that the gastroenteritis outbreak is associated with the consumption of raw seafood at a local restaurant. She considers it may be due to a number of vibrios EXCEPT: A. V. parahaemolyticus B. V. alginolyticus C. V. cholerae non 01 D. V. Jluvialis 104. To determine to which species the infectious agent belongs, the microbiologist performs some tests on colonies cultured from stool samples. These tests include the following EXCEPT: A. growth on thiosulfate-citrate-bile-sucrose (TCBS) agar B. fermentation of sucrose C. growth at different NaCl concentrations D. serotyping based on somatic O antigens 105. The pathogenic mechanisms that make Helicobacter pylori the causative agent of gastritis include the following EXCEPT: A. urease production B. invasive abilities C. motility D. microaeophilism 106. Campylobacter jejuni gastroenteritis is associated with consumption of contaminated water or foods which include the following EXCEPT: A. milk B. chicken C. clams D. hamburger Page 15 107. Antigenic variation in relapsing fever Borrelia species is due to: A. changes in the chromosomal DNA B. post-translational modifications of proteins C. conjugative transfer of plasmids D. switching of genes from a storage plasmid to an expression plasmid E. lousy gene transcription (different gene expression in lice and humans). 108. A patient in a rural area of New York had a 5 cm red rash with an expanding margin, on his back, that lasted for about a month and then went away. Later, the patient had episodes of partial facial paralysis and painful joints. Which of the following is the most likely infectious agent in this case? A. Borrelia hermsii B. Borrelia burgdorferi C. Leptospira interrogans D. Treponema pallidum subsp. pallidum E. Spirillum minor 109. Which of the following statements regarding Treponema pallidum is FALSE? A. It is routinely cultured from early lesions by clinical laboratories. B. It is too thin to be observed by standard light microscopy. C. It has several subspecies that cause different diseases. D. It ranges from 6 to 20 micrometers (µm) in length. E. It is an obligate parasite of humans. 110. The definitive diagnosis of syphilis is based on: A. detection of antibodies against cardiolipin. B. detection of antibodies against the causative agent. C. presence of circular, ulcerated lesions 1-2 cm in diameter. D. presence of the causative agent by darkfield microscopy. E. All of the above. 111. Which of the following statements is TRUE regarding syphilis? A. Asymptomatic infection is rare. B. Houston is a low incidence area. C. Gummatous syphilis is caused by the rapid outgrowth of large numbers of organisms, which directly damage the surrounding tissue. D. The disease is not transmissible at the secondary stage. E. Congenital syphilis is preventable with appropriate screening. 112. Penicillins are ineffective against Chlamydia because Chlamydia: A. lack ribosomes. B. have two different cell types. C. lack peptidoglycan. D. are able to escape phagolysosome fusion. Page 16 113. One characteristic that distinguishes the elementary body from the reticulate body cell type of Chlamydia is that only the elementary body: A. is infectious. B. is capable of cell division. C. is osmotically fragile. D. contains ribosomes. E. is bacterial in origin. 114. The metabolically active stage in the chlamydial life cycle is the: A. lysosome. B. exocytic particle. C. elementary body. D. cytoadsorption body. E. reticulate body. 115. All but one statement is true of Mycobacterium tuberculosis. Which one is UNTRUE? A. Obligate aerobe B. Produces few, if any toxins C. Grows rapidly compared with a staphylococcus D. Requires an enriched media E. DNA probes are useful in identification 116. Which one of the following is the greatest risk factor for tuberculosis? A. middle aged adult B. Scandinavian C. alcoholism D. stockbroker E. female 117. The one most reliable procedure in the definitive diagnosis of pulmonary tuberculosis is: A. acid-fast stain B. PPD skin test C. culture of sputum D. chest x-ray E. histology of a biopsy 118. Which one of the following statements is UNTRUE? Droplet nuclei: A. are the chief means of transmitting pulmonary infection with tuberculosis. B. are usually produced by coughing or sneezing. C. may float in air for several hours. D. are not an important source of infection in the emergency center of city/county hospitals. E. become small enough to bypass the normal upper airway defenses. Page 17 119. The most common source of infection for Mycobacterium tuberculosis in the U.S. is: A. sputum B. urine C. wound D. milk E water 120. Which of the following is TRUE of non-tuberculous mycobacteria? A. positive skill tests are rare. B. person-to-person spread occurs commenly. C. clinical illness is more common in the immunocompromised host. D. does not grow in soil. E. never produces pigment. 121. Those with AIDS (Acquired Immunodeficiency Syndrome) are most likely to have a severe infection with which one of the following organisms? A. Actinomyces israelii. B. Mycobacterium marinum. C. Mycobacterium avium-intracellulare. D. Mycobacterium smegmatis. E. Nocardia asteroides. 122. Assuming a positive skin test, who has the highest risk for illness with M tuberculosis? A. a patient with AIDS whose roommate recently has been diagnosed with cavitary pulmonary tuberculosis B. males over 45 C. normal chest x-ray D. a patient treated for 9 months with INH and Rifampin E. a 40-year old male with a partial gastrectomy 123. Which of the following statements is UNTRUE? The tuberculin skin test: A. is positive at 15 mm in duration or greater. B. may be falsely negative in severe immunocompromised. C. may be falsely positive in those with hepatitis. D. positive in about six weeks after becoming infected with the organism. E. done with a purified protein derivative (PPD) of killed organisms. 124. Of the organisms listed below, which one is the MOST frequent colonizer of endoscopes, respirators and other hospital equipment? A. Hemophilus influenzae B. Klebsiella pneumoniae C. Pseudomonas aeruginosa D. Enterobacter aerogenes E. Streptococcus pyogenes Page 18 TRUE OR FALSE Choose the best possible answer. A = True; B = False 125. _____ The Gram stain is the method of choice for diagnosis of Neisseria that is isolated from mucosal surfaces other than the conjunctiva and the male urethra. 126. _____ Generation of variant pilin forms by Neisseria spp. naturally occurs through intragenic recombination. OUESTIONS 127-130: The following drugs are antifolates: 127. _____ trimethoprim. 128. _____ gentamicin 129. _____ ciprofloxacin 130. _____ aztreonam 131. _____ Antibiotic resistance is an important clinical problem in day care centers. 132. _____ Antibiotic resistance is an important clinical problem in animal feed lots. 133. _____ Bacteroides fragilis elaborates endotoxin and can cause a syndrome nearly identical to the septic shock due to aerobic gram-negative bacilli. 134. _____ Bacteroides fragilis is commonly found in mixed anaerobic/aerobic bacterial infections that arise from bowel flora, because Bacteroides fragilis quantitatively accounts for the majority of Bacteroides species found in bowel flora. 135. _____ Although Clostridium tetani are frequently seen when they infect puncture wounds, they are difficult to identify because of variable staining characteristics and the absence of spores seen in clinical specimens. QUESTION 136: A woman had an illegal abortion, developed an infection of her uterus, and was also noted to be severely anemic and jaundiced. 136. _____ This clinical presentation could be due to infection by a Clostridium perfringens elaborating an alpha toxin. 137. _____ Vancomycin has cidal activity against gram-positive anaerobes. 138. _____ A candle jar does NOT generate an environment to support the growth of extremely oxygen sensitive (e.o.s.) organisms. Page 19 139. _____ Gas noted grossly on the x-ray of an infected foot of a diabetic patient might mean the presence of infecting Clostridium species, but more likely indicates gas produced by facultative Enterobacteriaceae. 140. _____ Clostridium docile causes food poisoning because it produces an enterotoxin that causes a secretory diarrhea that lasts only 24-36 hours. 141. _____ Actinomycosis can be strongly suspected based on the findings of "sulphur granules" in a clinical specimen. 142. _____ Lymphogranuloma venereum (LGV) is caused by Chlamydia trachomatis. 143. _____ Interstitial pneumonia in neonates is caused by Chlamydia pneumonia acquired via an infected maternal birth canal. 144. _____ Replacement of electrolytes is the hallmark of therapy for diarrhea, especially for severe cases of cholera. 145. _____ Shigella serotyping is based on O and H antigens. 146. _____ Pseudomonas aeruginosa is commonly isolated from the respiratory secretions of patients with cystic fibrosis. 147. _____ Antibiotic resistance is an important clinical problem in animal feed lots. Page 20 ANSWERS: 1. C 2. C 3. B 4. C 5. C 6. D 7. B 8. A 9. D 10. B 11. D 12. C 13. B 14. D 15. A 16. D 17. A 18. B 19. A 20. C 21. B 22. D 23. A 24. E 25. A 26. C 27. D 28. B 29. B 30. C 31. E 32. D 33. C 34. E 35. B 36. A 37. A 38. A 39. B 40. A 41. A 42. B 43. B 44. A 45. B 46. B 47. A 48. A 49. A 50. A 51. B 52. C 53. A 54. B 55. A 56. B 57. B 58. C 59. D 60. A 61. B 62. E 63. D 64. E 65. D 66. D 67. B 68. D 69. C 70. B 71. C 72. A 73. A 74. B 75. B 76. C 77. B 78. B 79. C 80. B 81. D 82. B 83. D 84. D 85. A 86. B 87. C 88. B 89. C 90. C 91. B 92. B 93. D 94. B 95. E 96. D 97. A 98. B 99. C 100. 101. 102. 103. 104. 105. 106. 107. 108. 109. 110. 111. 112. Page 21 B D A B D B C D B A E E C 113. 114. 115. 116. 117. 118. 119. 120. 121. 122. 123. 124. 125. 126. 127. 128. 129. 130. 131. 132. 133. 134. 135. 136. 137. 138. 139. 140. 141. 142. 143. 144. 145. 146. 147. A E C C C D A C C A C C B A A B B B A A A B B A A A A B A A B A B A A