* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download digestion - Learning Central
Survey
Document related concepts
Transcript
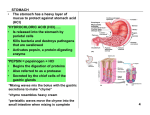
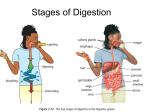
Wales College of Medicine, Biology, Life and Health Sciences School of Nursing and Midwifery Studies DIGESTION Most foods are complex compounds that cannot be utilised by the body in their original form. After ingestion, the process of digestion enables these complex structures to be broken down into their more easily metabolised molecules. While this session mainly deals with the fate of carbohydrates, proteins and fats, do not forget the dietary importance of fluids, vitamins and minerals. Mechanical processes assisting in digestion. Following ingestion, food is ground down by the teeth (mastication) and mixed with saliva by the tongue. The food is formed into a ball (bolus) before being pushed across the roof of the mouth to the pharynx to be swallowed (deglutition). Muscular waves (peristalsis) within the walls of the oesophagus move the bolus on to the stomach, entering via a muscle ‘ring’ (cardiac sphincter). The longitudinal, circular and oblique muscles within the stomach wall churn the food, mixing in the gastric juices, until liquid chyme is released via a second muscle ‘ring’ (pyloric sphincter). FUNDUS Relatively thin muscle wall providing gentle contractions BODY ANTRUM 30ml capacity. Each relaxation of the pyloric sphincter ejects just 3 ml chyme. The remaining 27 ml is ‘thrown back’ for further mixing. With approximately 3 contractions per minute, the stomach will usually empty in 4 hours (6 hours with a high fat content). The small intestine continues to mix chyme via localised contraction and relaxation of adjacent segments (segmentation). Digestion and absorption are maximised by overall gut length and the presence of structural modifications that increase surface area: circular folds creating a slow ‘spiral’ movement of chyme along the lumen, villi, Microvilli. The gastro-intestinal tract is prepared for its role in digestion by both nervous and hormonal control. The thought, sight or smell of food triggers parasympathetic stimulation of salivary glands and gastric gland pits, resulting in early production of both saliva (up to 1.5 litres daily) and gastric juices (2-3 litres daily). This is further enhanced by the presence and/or taste of food in the mouth, the latter triggering production of the hormone gastrin from endocrine tissue within the stomach lining. Digestion and the mouth Parotid (25%) – secretion mostly water Sublingual (5%) – secretion mostly mucous Submandibular – (70%) – contains water and mucous. Consisting of up to 99.5% water, saliva keeps the mouth moist. This helps prevent infection and ulceration, aided by a protective bacterial flora, bacteriostatic enzymes and antibodies. It contains the electrolytes sodium, potassium and chloride and, importantly, a high concentration of bicarbonate to neutralise the acids produced by the flora. This neutralisation also minimises tooth decay while calcium salts prevent passive dissolution of tooth calcium. Mucous, containing mucin (a water-soluble protein), aids in the swallowing of food. Sympathetic induced vasoconstriction to salivary glands may reduce the water content of saliva, increasing the mucin concentration and causing breath odour (halitosis). Digestion is limited in the mouth with salivary amylase (pH 6.35-6.85) commencing the breakdown of starch (polysaccharide). Recent suggestions are that a salivary lipase is also present. Digestion and the stomach Apart from water, the major component of gastric juice is hydrochloric acid (HCl). Secreted by the parietal cells, along with the polypeptide intrinsic factor, it creates a stomach pH <2. Acid production is also influenced by levels of histamine released by ECL cells. To protect itself against the low pH, gastric juice also produces mucous (from goblet cells) and bicarbonate (from surface epithelial cells). Stomach activity is influenced by other hormonal secretions. Serotonin (also from ECL cells) increases stomach contraction while somatostatin inhibits stomach emptying. Once in the stomach, chyme is subjected to the many influences of gastric juice. HCl has a range of functions including: ‘denatures’ proteins – weak bonds creating tertiary structures are weakened; activates pepsinogen, an inactive (….ogen) proteolytic enzyme stored in, and secreted by, the chief cells; deactivates salivary amylase remaining in the chyme. Active pepsin breaks down the now redundant salivary amylase and also commences the breakdown of ingested proteins into smaller polypeptides. The intrinsic factor is needed to ‘mark’ vitamin B12 for absorption in the terminal ileum. Digestion and the gut The microvilli, projections of the mucosal cells often referred to as the brush border, contain many digestive enzymes […ase]. Goblet cells, secreting mucous, are found throughout its length though they too are more specialised in the duodenum. Here they are referred to as Brunner’s glands and secrete a thick, alkaline mucous to combat the acid chyme from the stomach. In addition enteroendocrine cells secrete controlling hormones while Peyer’s patches (lymphoid tissue) add a defence against ingested organisms. Between the villi are deep gland pits (crypts of Lieberkuhn) secreting a watery intestinal juice. The base of the crypts is the site for the formation of the goblet, endocrine and lining epithelial cells. These gradually move to the tips of the villi before being worn away. Thus, the lining is replaced every 5-6 days. The intestinal juice therefore contains small amounts of mucous, hormones and enzymes from the cell remnants. In the duodenum, the presence of fats and/or proteins in the chyme triggers the release of the intestinal hormones cholycystokinin/cck (increases gall bladder contraction and pancreatic enzyme production) and secretin (bile and pancreatic juice). Bile and pancreatic juices (up to 1.5 Litres each daily) are released into the duodenum via the ampulla of Vater, ‘controlled’ by the sphincter of Oddi. Bile and pancreatic juice is mixed with the chyme by segmentation. Most fats (triglycerides) are too complex to allow easy digestion. Bile, released from the gall bladder, acts as an emulsifier (saponification) – a similar action to detergent to split the fats into smaller droplets. This increases the surface area of the fats, allowing the fat enzymes to work more effectively. Pancreatic lipase breaks these down into fatty acids and monoglycerides. Pancreatic juice is highly alkaline (pH 8), further ‘buffering’ the acid chyme and inactivating pepsin. As well as triggering the release of cck and secretin, the presence of food in the duodenum also stimulates the intestinal wall to secrete the enzyme enterokinase. As previously seen in the stomach, all protein enzymes are stored and secreted in an inactive form to prevent autodigestion of the body’s own organs. Enterokinase is the activator of the pancreatic protein enzymes. Initially trypsinogen is activated to trypsin which in turn activates chymotrysinogen to chymotrypsin. Together, they break down the peptide bonds (endopeptidases), within the protein chains, to form smaller peptides. Additionally, carboxypeptidase strips amino acids from the end of the chains (aminopeptidase). Similarly, aminopeptidases within the intestinal wall complete the breakdown into smaller amino acids, dipeptides and tripeptides. Ingested DNA and RNA are broken down by nucleases Carbohydrate digestion continues with more amylase from the pancreas. This continues the conversion (see below) of polysaccharides to smaller disaccharides (twin sugars). Polysaccharides (i) Disaccharides (ii) Monosaccharides (Pancreatic Amylase) maltose fermentation sugar (maltase) glucose fruit/honey sugar sucrose cane/beet sugar (sucrase) fructose fruit sugar + glucose lactose milk sugar (lactase) galactose + glucose As nutrients are absorbed across the intestinal wall they come into contact with brush border enzymes. Lipase continues the digestion of monoglycerides during their absorption into the central lacteals of the villi. The enzymes maltase, sucrase and lactase act on their respective disaccharide (double sugars) to complete (see above) the final digestion of carbohydrates to monosaccharides (single/simple sugar). A.Matthews/07/05