* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download SE7-3
Survey
Document related concepts
Transcript
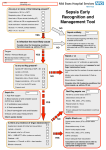
ED Skills Review Important Points for Level 1, Sepsis Monitor, CVP/Arterial Lines, Chest Tubes, HACA, & RSI/Procedural Sedation Level 1 - - - - - This is to be run by 1 dedicated RN (it is outside the tech scope to set it up or run this piece of equipment) Fluids can be run in 1 of 2 ways: o Warmed (104F constant temperature) o Warmed AND rapid All bags that are hung must be air free o To remove air, spike the bag, turn it upside down and squeeze the air to the top of the bag. When fluid appears, you can put the spike back in the bag. Always hang 3 bags of fluid (each one should be 1 liter)-2 can be on the pressure compartments and one is free hanging o Number the bags as you hang them so you can track the total amount of fluid infused o Under pressure, the Level 1 infuses a full liter in about 90 seconds. When the bag has the final 50-100 mL in it, clamp the tubing, open the free hanging bag not under pressure to keep fluid flowing and no air into the system, and change out the bags For rapid infusions: should use a central line but in a true emergency, can use a large bore IV in the AC Blood, FFP, and cryo may be given via the Level 1 o The filter is good for 4 units of blood product; after 4 units, change the filter and/or the tubing [if more than 4 units is being given, consider activating the MASSIVE TRANSFUSION PROTOCOL] o NEVER give platelets though a blood filter-the platelets are too small and will catch in the filter The machine occasionally needs to be refilled with distilled water. You can obtain distilled water from Lab (they have a spigot; we can fill a 24 hour urine container with more than enough) CVP/Arterial Line - The red plug cable is needed to measure CVP/art lines Use a 500 mL bag of NS (never heparin!) in a pressure bag to ensure patency of the line o Always get the air out of the bag prior to connecting the tubing to the patient! The transducer needs to be zero’d to ensure the readings are accurate After being zero’d, the transducer needs to be at the phlebestatic axis (4th intercostal space, mid-axillary line)-tape it to the patient’s chest to ensure continued accuracy CVP: measure of intravascular volume; 6-10 is considered normal Arterial line: measure of intra-arterial blood pressure Chest Tubes - There should be no bubbling in the Atrium (bubbling is always indicative of an air leak) - There should be 2 cm of sterile water in the Atrium water seal (if not enough or too much, use the needle port on the back to put more in or take some out) - The Atrium has one way valves so if it is tipped over, fluid will not leak out - Stripping or milking chest tubes is STRICTLY PROHIBITED - Chest tubes are NEVER directly connected to wall suction! o The chest tube should connect to the Atrium which is connected to wall suction - For a simple pneumothorax, consider a Heimlich valve o You can use an Atrium but it does not need to be connected to suction - For a hemopneumo or drainage of pleural fluids, the Atrium should be connected to suction per provider orders o It is OK to have suction off for a period of time (e.g., transport across town) o If the patient has an Atrium, a RN needs to go on the transport (whether upstairs within SFMC or across town) HACA - Always protect skin from cold (whether it is cold packs or the cooling blankets) with a sheet or towel - The nurse must document a very thorough skin exam to ensure any skin breakdown is well documented prior to admission - Shivering is to be prevented at all costs (it causes the basal metabolic rate to rise which defeats the purpose of HACA) o Putting socks on the feet and hands can help prevent shivering o Might need to consider increasing the amount of paralytics - 2 L of cold saline is the MAX (if patient comes in via EMS, always ask how many liters they gave of cold saline and document it) o Our 2 L of cold saline is in the main med room Pyxis fridge Sepsis - - What can cause sepsis: Infection or trauma; both of these conditions cause immune system response and release of leukotrienes which causes systemic inflammatory response Some people do fine with this response and recover OK while others head down the sepsis path First stop on the sepsis path: SIRS (Systemic Inflammatory Response Syndrome) SIRS causes microvascular leakage which depletes circulating volume which then causes occult global tissue hypoxemia (less circulating volume means less Hgb which means less O2 to cells and the start of end organ damage due to hypoxia even though the pulse ox might be WNL) o Quick assessment for possible sepsis (shock index): HR/SBP. If the ratio is close to or greater than 1, the patient should be a high urgent/emergent triage for possible sepsis work-up. Get staff to think: Blood culture order means there should be a lactate order (or at least ask the provider if a lactate order is indicated)! Interventions: Fluids, fluids and more fluids (sometimes 6 L in the 1st 8 hours!) o Sepsis cath: A specialized triple lumen catheter that measures the oxygenation of the blood returning to the heart (remember the microvascular leakage causes less Hgb which causes less O2 to the cells); normal limits are 70+ o If no sepsis cath, central line should still be considered due to massive amounts of volume replacement. Where is it best to place the central line? The right subclavian. Why? Because the tip of the central line is actually in the superior vena cava (remember, the big vessel that brings all our body’s blood back to the heart!) so you can get an accurate CVP. Why would we want a CVP? To see just how extensive the microvascular leakage is so that can adequately direct our volume replacement. (You could put the central line in the left subclavian but the tip will not actually enter the superior vena cava so then you will get funky readings because of the back-pressure on the left subclavian valve emptying into the superior vena cava.) o Once we do fluid replacement, we next want to do antibiotic therapy. We might also consider blood replacement (depending on H/H levels), again, because microvascular leakage causes loss of Hgb into the interstitial tissue. - Scenario: 28 year old male comes into the ED, chief complaint of difficulty breathing. Vitals signs: RR-22, Temp-99.6F, HR-100, SBP-90, Pulse ox-93% room air. History of cystic fibrosis. o Septic? Possibly. The HR/SBP is 1.1 ratio so strong likelihood of at least SIRS. o Medical plan of care: Put in sepsis cath and prep CVP set-up o Sepsis cath reading is 68-70. CVP is 3-4. o Interventions? Fluid, fluid, fluid, probably about 3 L. o Concern: cystic fibrosis. This patient’s CVP is low so he is very dry and has quite a bit of fluid leakage from intravascular area to interstitial tissues. Getting his CVP back to a normal baseline, regardless of his medical lung history, is not a primary concern at this point. o Pressor support? Giving pressors to someone who is ‘dry as a chip’ causes the pump (the heart) to work much harder at pumping depleted volumes. This is more likely to throw the patient into some type of cardiac event instead of correcting the underlying issue of not enough volume to pump. Sepsis Monitor - - Set up should ALWAYS be on the right side of the chest o Goal: Get the tip of the sepsis catheter into the superior vena cava o Readings: Anything over 70 is considered normal o The monitor is measuring the oxygen content of the blood returning to the heart. Sepsis causes microvascular leakage which decreases intravascular volume which in turn depletes the oxygen in the remaining volume. Sepsis typically causes extensive intravascular dehydration so the next step to be anticipated by the nurse is to measure CVP, hence the need to be in the superior vena cava (placing the catheter in the left subclavian gets the tip just far enough away from dropping into the SVC and can cause false CVP readings from backflow) Ensure a Biodisk is placed prior to putting an opsite over the catheter Ensure the lumens are capped off with the blue buff caps It is best to calibrate the catheter when it is in the package (in vitro) o Push start AFTER the lumens have been flushed and capped! PROCEDURAL SEDATION REFERENCE CHECKLIST **See IDP S-01-e and ES P-01-a for specific information/updates 1. Every patient must have a pre-procedure assessment documented. a. Part one of this assessment is a physical assessment which is based on the American Society of Anesthesiologists (ASA) classifications. i. RNs may provide sedation for Class 1 & 2 patients. ii. Class 3 & 4 patients are outside the RN scope. We may not sedate but can monitor; in these situations, there needs to be 2 physicians available who can intubate should the patient condition decompensate. 1. Patients who have a formal OSA diagnosis should be considered Class 3. ASA Physical Status 1 - A normal healthy patient ASA Physical Status 2 - A patient with mild systemic disease ASA Physical Status 3 - A patient with severe systemic disease ASA Physical Status 4 - A patient with severe systemic disease that is a constant threat to life b. 2. 3. 4. Part two is to always have the difficult airway cart bedside for each sedation and document you did! Every sedation, regardless of which medications are given, must have capnography utilized (and the readings documented with the vital signs). Propofol & Etomidate: RNs may NOT push this medications for procedural sedation. The RN must document which MD administered the medication. Vital signs: Vital signs for a procedural sedation must be documented in the Moderate Sedation treatment in Meditech (or the Moderate Sedation Re-assessment). a. Vital signs are to be done pre-procedure and documented, preferably in the Moderate Sedation treatment in Meditech. b. Vital signs should be taken throughout the procedure and an Aldrete score documented with each set. c. A patient may NOT be discharged from procedural sedation monitoring until the Aldrete score is either a 9 or a 10. **If a patient ever has an ADVERSE EVENT (such as needs BVM, requires intubation because of procedural sedation, or reversal of procedural sedation medications) an OCCURRENCE REPORT must be completed! Capnography Capnography, on the other hand, is a indirect monitor and helps in the differential diagnosis of hypoxia to enable remedial measures to be taken sexpeditious before hypoxia results in an irreversible brain damage. Capnography provides information about CO2 production, pulmonary perfusion, alveolar ventilation, respiratory patterns, and elimination of CO2 from the anesthesia circuit and ventilator. Capnography has been shown to be effective in the early detection of adverse respiratory events. Capnography and pulse oximetry together could have helped in the prevention of 93% of avoidable anesthesia mishaps according to ASA closed claim study. Capnography has also been shown to facilitates better detection of potentially lifethreatening problems than clinical judgment alone (Cote et al). Reading low: Indicates impaired gas exchange at cellular level (i.e., shock) Reading high: Indicates too much CO2 is being exchanged (i.e., slow but deep respirations, metabolic issues)