* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Advances in Environmental Biology Staphylococcus AENSI Journals
Gastroenteritis wikipedia , lookup
Hospital-acquired infection wikipedia , lookup
Human microbiota wikipedia , lookup
Bacterial cell structure wikipedia , lookup
Marine microorganism wikipedia , lookup
Traveler's diarrhea wikipedia , lookup
Staphylococcus aureus wikipedia , lookup
Bacterial morphological plasticity wikipedia , lookup
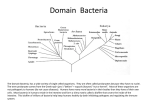
Bacterial taxonomy wikipedia , lookup
Advances in Environmental Biology, 7(11) Oct 2013, Pages: 3549-3554 AENSI Journals Advances in Environmental Biology Journal home page: http://www.aensiweb.com/aeb.html Beta lactamase Producer Staphylococcus species in Iranian Foods Shila Jalalpour Molecular Medicine Research Center, Rafsanjan University of Medical Sciences, Rafsanjan, Iran. ARTICLE INFO Article history: Received 23August 2013 Received in revised form 24 September 2013 Accepted 29 September 2013 Available online 17 November 2013 Key words: Staphylococcus aureus, Coagulase Negative Staphylococci, β-lactamase, Foods ABSTRACT Staphylococcal food poisoning occurs most often in foods that require hand preparation, such as potato salad, ham salad, sandwich spreads, raw foods; unpasteurized milk. S. aureus found on humans (skin, infected cuts, pimples, noses and throats).When S. aureus is allowed to grow in foods, can produce a toxin that causes illness. Although cooking destroys the bacteria, the toxin produced is heat stable and may not be destroyed. Symptoms of Staphylococcus aureus food borne illnesses are severe nausea, fever, abdominal cramps, vomiting and diarrhea. BetaLactamase confers penicillin resistance to various bacterial organisms by cleaving the beta-lactam ring of penicillin's and cephalosporin antibiotics. The subject of this study was survey of the prevalence of Beta lactamase enzyme in Staphylococcus species isolated of foods in Isfahan city in Iran. This laboratory study was performed during 2009-2010 years in Isfahan. In this study, 150 food samples including, ketchup, mayonnaise, biscuits and chocolate were randomly sampled and cultured on Blood Agar; and incubated for 24 hours. Identification of bacteria were based on microbiological methods (staining, biochemical test). Identification of βlactamase, was performed with the Acidometric method with Penicillin G5000000 Unit and Phenol Red. A positive test was indicated by the mixture turning yellow in color. From 150 samples collected, 142(95%) samples were contaminated with Staphylococcus species. According to the acidometric result, the frequency of βlactamase in the Staphylococcus species was 112 (75%). Antibiotic resistance may be intrinsic or result from either mutation of existing genetic material or from acquisition of new genetic material. The results of this study represented vast spread of beta lactamase in Staphylococcus species in food. Beta lactamase enzyme leads to bacterial resistance against beta Lactame antibiotics. © 2013 AENSI Publisher All rights reserved. INTRODUCTION Food borne illnesses are caused by eating food or drinking beverages contaminated with bacteria, parasites, or viruses. Harmful chemicals can also cause food borne illnesses if they have contaminated food during harvesting or processing. Food borne illnesses can cause symptoms that range from an upset stomach to more serious symptoms, including diarrhea, fever, vomiting, abdominal cramps, and dehydration [15]. Most food borne infections are undiagnosed and unreported, though the Centers for Disease Control and Prevention (CDC) estimates that every year about 76 million people in the United States become ill from pathogens, or diseasecausing substances, in food. Of these people, about 5,000 die [3,17,26,27]. Harmful bacteria are the most common cause of food borne illnesses. Some bacteria may be present on purchased foods. Such as raw foods are the most common source of food borne illnesses because they are not sterile; examples include raw meat and poultry that may have become contaminated during slaughter. Seafood may become contaminated during harvest or through processing. One in 10,000 eggs may be contaminated with Salmonella inside the egg shell. Products such as spinach, lettuce, tomatoes, sprouts, and melons can become contaminated with Salmonella, Shigella, or Escherichia coli (E. coli) O157:H7. Contamination can occur during growing, harvesting, processing, storing, shipping, or final preparation. Sources of products contamination are varied as these foods are grown in soil and can become contaminated during growth or through processing and distribution. Contamination may also occur during food preparation in a restaurant or a home kitchen [3,17,26,27]. When food is cooked and left out for more than 2 hours at room temperature, bacteria can multiply quickly. Most bacteria grow undetected because they don’t produce a bad odor or change the color or texture of the food. Freezing food slows or stops bacteria’s growth but does not destroy the bacteria. The microbes can become reactivated when the food is thawed. Refrigeration also can slow the growth of some bacteria. Thorough cooking is needed to destroy the bacteria [4,18,22,23]. Staphylococcus aureus food poisoning is an illness that Corresponding Author: Shila Jalalpour,Molecular Medicine Research Center, Rafsanjan University of Medical Sciences, Rafsanjan, Iran. E-mail:[email protected] 3550 Shila Jalalpour Advances in Environmental Biology, 7(11) Oct 2013, Pages: 3549-3554 results from eating food contaminated with a toxin produced by this bacteria [17]. It’s often caused when a food handler contaminates food products that are served or stored at room- or refrigerator temperature. Common examples of such foods are desserts (especially custards and cream-filled or topped desserts), salads (especially those containing mayonnaise, such as tuna salad, potato salad, and macaroni salad), poultry and other egg products, and casseroles [1,2,22,29]. Staphylococcal food poisoning is caused by eating food contaminated with Staphylococcus aureus. S. aureus is able to grow in a wide range of temperatures, pH (4.2 to 9.3) and sodium chloride (salt) concentrations. These characteristics enable S. aureus to grow in a wide variety of foods and conditions. Often this type of food poisoning occurs when cooked food is allowed to cool slowly and/or sit at room temperature for some time. The warm food allows the S. aureus bacteria to grow. These bacteria produce a toxin enterotoxin that remains in the food even when reheated. The symptoms are caused by the toxin not by the bacteria themselves, hence staphylococcal food poisoning is sometimes called food intoxication' [19,20,24,25,30]. Staphylococci are ubiquitous. These bacteria are present in air, dust, dirt, sewage, water, milk, and food, or on food equipment, environmental surfaces, humans, and animals. Humans and animals are the primary reservoirs. Staphylococci are present in the nasal passages and throats and on the hair and skin of 50 percent or more of healthy individuals. The colonization rate is even higher for those who work with or who come in contact with sick individuals and hospital environments [1,2,21, 29,25]. The bacteria produce a toxin in the food, which causes most of the symptoms. Risk factors include: Eating food that was prepared by a person with a skin infection (these infections commonly contain Staphylococcus aureus bacteria), Eating food kept at room temperature, Eating improperly prepared food, Eating the same food as someone who has symptoms, Symptoms usually appear within 1- 6 hours after eating contaminated food. Usually, symptoms last only 2 days or less, They may include: Nausea, Vomiting for up to 24 hours, Diarrhea, Loss of appetite, Severe abdominal cramps, Abdominal distention, Mild fever [19,20,24,25,30]. The goal of treatment is to replace fluids and electrolytes (salt and minerals) lost by vomiting or diarrhea. Antidiarrheal medications may be used, but are often not needed. Full recovery is expected. Recovery usually occurs in 24 to 48 hours [24,25,30]. To avoid dehydration, you or your child should drink water and electrolyte solutions to replace fluids lost by vomiting. A variety of pleasant-tasting electrolyte solutions are available over-the-counter. Solutions to try for children: Pedialyte and Infalyte, Popsicles or Jello [19,20,24,25,30]. People with diarrhea who are unable to take fluids by mouth because of nausea or vomiting may need intravenous fluids. This is true especially for small children, People taking diuretics (water pills) may need to stop taking them during the acute episode. Ask your health care provider for instructions [19,20,24,25,30]. The antibiotic action is an environmental pressure; those bacteria which have a mutation allowing them to survive will live on to reproduce. They will then pass this trait to their offspring, which will be a fully resistant generation. Antibiotic resistance is the ability of a micro-organism to withstand the effects of an antibiotic. It is a specific type of drug resistance [16]. Antibiotic resistance evolves naturally via natural selection through random mutation, but it could also be engineered. SOS response of low-fidelity polymerases can also cause mutation via a process known as programmed evolution. Once such a gene is generated, bacteria can then transfer the genetic information in a horizontal fashion (between individuals) by plasmid exchange. If a bacterium carries several resistance genes, it is called multiresistant or, informally, a superbug[5]. The beta lactam antibiotics enters the bacterium via the porin and binds to the penicillin-binding proteins (PBP's),and inhibiting cell wall synthesis. There are several ways that the bacterium can side-step this attack, this mechanisms are as follows: 1. Diminished transport into the bacterium; The bacterium on the left has lost the porin that normally transports the antibiotic into the cell. In a normal environment, such a loss would be a disaster for the bacterium as it would lose its competitive edge over other bacteria. 2. An altered binding site; This bacterium has a slightly altered PBP [5,6].The PBP can still carry out its function, but is no longer inhibited by the penicillin, which cannot bind to it. The bacterium carries on unscathed. 3. Enzymes that break down the antibiotic; This is an important method of resistance for many bacteria. Beta lactams are for example broken down by beta lactamases. There is a whole host of beta lactamases, and new ones seem to be discovered every day. Although more attention has been focussed on beta lactamases than on other enzymes that destroy antibiotics, there are many such enzymes that break down aminoglycosides, chloramphenicol, and so on [5,6]. Beta-lactamases are enzymes (EC 3.5.2.6) produced by some bacteria and are responsible for their resistance to beta-lactam antibiotics like penicillins, cephalosporins (are relatively resistant to beta-lactamase), cephamycins, and carbapenems (ertapenem). These antibiotics have a common element in their molecular structure: a four-atom ring known as a beta-lactam. The lactamase enzyme breaks that ring open, deactivating the molecule's antibacterial properties [5-7]. Beta-lactam antibiotics are typically used to treat a broad spectrum of grampositive and gram-negative bacteria. Beta-lactamases produced by gram-positive organisms are usually secreted [5-7]. Penicillinase is a specific type of β-lactamase, showing specificity for penicillins, again by hydrolysing the beta-lactam ring. Molecular weights of the various penicillinases tend to cluster near 50kD (12-14). 3551 Shila Jalalpour Advances in Environmental Biology, 7(11) Oct 2013, Pages: 3549-3554 Penicillinase was the first β-lactamase to be identified: it was first isolated by Abraham and Chain in 1940 from gram-negative E. coli even before penicillin entered clinical use but penicillinase production quickly spread to bacteria that previously did not produce it or only produced it rarely. Penicillinase-resistant beta-lactams such as methicillin were developed, but there is now widespread resistance to even these [5-7]. The subject of this study was survey prevalence Beta lactamase enzyme in Staphylococcus species isolated of foods In Isfahan city in Iran. MATERIALS AND METHODS Sampling: This laboratory study was performed during 2009-2010 years in Islamic Azad University Shahreza branch in Isfahan. In this study, a total of 150 food samples including, ketchup, mayonnaise, biscuits and chocolate were randomly selected. Bacterial strains: The Bacteria were identified on the basis of colony morphology, Gram stain reaction, spore formation, and biochemical tests with the BioMerieux database system. The specimens grew on sheep blood incubated at 37°C under aerobic conditions (5,28). A Gram stain was first performed to guide the way, which showed a typical gram-positive bacteria, cocci, in clusters. The isolates were cultured on mannitol salt agar, which was a selective medium with 7–9% NaCl that allows S. aureus to grow, producing yellow-colored colonies as a result of mannitol fermentation and subsequent drop in the medium's pH. Furthermore, for differentiation on the species level, catalase (positive for all Staphylococcus species), coagulase (fibrin clot formation, positive for S. aureus), DNAse (zone of clearance on nutrient agar), lipase (a yellow color and rancid odor smell), and phosphatase (a pink color) tests were all done. For staphylococcal food poisoning, phage typing were performed to determine the staphylococci recovered from the food [5-7, 28]. Detection Beta Lactamase: Acidometric test is a Diagnostic test for the rapid detection of the β-lactamase in bacteria. This test is based on hydrolysis of the β-lactam ring, which results in the production of penicilloic acid. This process caused acidification of the bacterial suspension, and changed the colour of the acidobasic indicator phenol red. The result of the reaction is very fast. The red color of this indicator represent negative test and the yellow color of this indicator represent positive test (Figure 1) [8-11]. Fig. 1: Beta Lactamase Test Results: In present study that was performed with laboratory method during of 9 month in 2009-2010 years in Isfahan A total 150 food samples including, ketchup, mayonnaise, biscuits and chocolate, randomly selected and were study. Specimen transfer to microbiology laboratory and in sterile condition, cultured on sheep blood incubated at 37 °C under aerobic conditions. According results from 150 food samples, all of ketchup, mayonnaise, biscuits, chocolate samples (100%) was contaminated with Staphylococcus species. 3552 Shila Jalalpour Advances in Environmental Biology, 7(11) Oct 2013, Pages: 3549-3554 According results of this study from 150 sample,142 (95%) sample was contaminated with Staphylococcus species. According to Acidometric result frequency β-lactamase in the Staphylococcus species was 112 (75%). 77% strain of Staphylococcus aureus and 73% coagulase negative Staphylococcus produce β-lactamase.(Diag 1) Respectively 85%, 80%, 70, 70% and 70% of Staphylococcus species isolated from ketchup, mayonnaise, biscuits, chocolate samples, can produce β-lactamase.(Diag 2) Diagram. 1:Beta lactamase in Coagulase negative and positive Staphylococcus isolated from foods Diagram. 2: Beta lactamase in Staphylococcus spp. isolated from foods Discussion: More than 90 percent of the cases of food poisoning each year are caused by Staphylococcus aureus, Salmonella, Clostridium perfringens, Campylobacter, Listeria monocytogenes, Vibrio parahaemolyticus, Bacillus cereus, and Entero-pathogenic Escherichia coli. These bacteria are commonly found on many raw foods. Normally a large number of food-poisoning bacteria must be present to cause illness. Food borne illness can be prevented by controlling the initial number of bacteria present, preventing the small number from growing ,destroying the bacteria by proper cooking and avoiding re-contamination. The onset of symptoms in staphylococcal food poisoning is usually rapid and in many cases severe, depending on individual susceptibility to the toxin, the amount of contaminated food eaten, the amount of toxin in the food ingested, and the general health of the victim [4,23]. It is important to prevent the contamination of food with Staphylococcus before the toxin can be produced. S. aureus is often present on skin, under fingernails, in the nose and throat, in cuts, 3553 Shila Jalalpour Advances in Environmental Biology, 7(11) Oct 2013, Pages: 3549-3554 abrasions, boils, and abscesses. S. aureus can also be found on contaminated surfaces and food preparation utensils. The following can help prevent staphylococcal food poisoning: Washing hands and under fingernails vigorously with soap and water before handling and preparing food; Not preparing food if a person has a nose or eye infection; Not preparing or serving food for others if a person has wounds or skin infections on the hands or wrists; Keeping kitchens and food-serving areas clean and sanitized; Keeping hot foods hot (over 140°F) and cold foods cold (40°F or under); Especially if the food is stored for more than 2 hours; Storing cooked food in a wide, shallow container and refrigerating as soon as possible [4,23] Antibiotic resistance can also be introduced artificially into a micro-organism through transformation protocols. This can be a useful way of implanting artificial genes into the micro-organism [13]. Antibiotic resistance is a consequence of evolution via natural selection or programmed evolution. The antibiotic action is an environmental pressure; those bacteria which have a mutation allowing them to survive will live on to reproduce. They will then pass this trait to their offspring, which will be a fully resistant generation [13,5]. Several studies have demonstrated that patterns of antibiotic usage greatly affect the number of resistant organisms which develop. Overuse of broad-spectrum antibiotics, such as second- and third-generation cephalosporins, greatly hastens the development of methicillin resistance, even in organisms that have never been exposed to the selective pressure of methicillin per se (thus the resistance was already present). Other factors contributing towards resistance include incorrect diagnosis, unnecessary prescriptions, improper use of antibiotics by patients, and the use of antibiotics as livestock food additives for growth promotion (5). Staphylococcal resistance to penicillin is mediated by penicillinase (a form of β-lactamase) production: an enzyme that cleaves the β-lactam ring of the penicillin molecule, rendering the antibiotic ineffective. Penicillinase-resistant β-lactam antibiotics such as methicillin, nafcillin, oxacillin, cloxacillin, dicloxacillin, and flucloxacillin are able to resist degradation by staphylococcal penicillinase (5). Spread of S. aureus (including MRSA) is through human-to-human contact, although recently some veterinarians have discovered that the infection can be spread through pets, with environmental contamination thought to play a relatively unimportant part. Emphasis on basic hand washing techniques are, therefore, effective in preventing the transmission of S. aureus (5). REFERENCES [1] Cenci-Goga, B.T., M. Karama, P.V. Rossitto, R.A. Morgante, J.S. Cullor, 2003. Enterotoxin production by Staphylococcus aureus isolated from mastitic cows. Journal of food protection., 66(9): 1693-1696. [2] Cimolai, 2008. MRSA and the environment: implications for comprehensive control measures. European journal of clinical microbiology & infectious diseases: official publication of the European Society of Clinical Microbiology, 27(7): 481-493. [3] Doyle, M.P., M.C. Erickson, 2007. Reducing the carriage of foodborne pathogens in livestock and poultry.Available at: http://www.poultryscience.org/ps/ paperpdfs/06/ p0660960 .pdf. Retrieved. [4] Food and Drug Administration, 2007.Guidance for Industry and FDA - Letter to State Agricultural Directors, State Feed Control Officials, and Food, Feed, and Grain Trade Organizations . Available at: http://www.cfsan.fda.gov/~dms/graingui.html. Retrieved. [5] Jalalpoor, Sh., R. Kasra Kermanshahi, A. Noohi, H. Zarkesh Esfahani, 2007. Study of -lactamase and Slayer Production in some of Isolated Pathogen Bacteria From Clinical and Environmental Hospital Samples. MSc thesis,Iran, Tehran, Islamic Azad University Science and Research Branch Tehran, 169-207. [6] Jalalpoor, Sh., R. Kasra Kermanshahi, A.S. Nouhi, H. Zarkesh Esfahani, 2008. Comparison of the Frequency β-lactamase Enzyme in Isolated Nosocomial Infectious Bacteria. Journal of Rafsanjan University of Medical Science, 8(3): 203-214. [7] Jalalpoor, Sh., R. Kasra Kermanshahi, A.S. Nouhi, Zarkesh Esfahani, 2008. The comparative frequency of β-lactamase production and antibiotic susceptibility pattern of bacterial strains isolated from staff hands and hospital surfaces in Alzahra Hospital–Isfahan. Iranian Journal of Medical Microbiology, 3(4): 37-45. [8] Jalalpoor, Sh., H. Abousaidi Survey, 2009. Role and Important of Surfaces Structure and β-lactamase of Bacillus cereus in Drug Resistant. Journal of Microbial World., 2(3):169-176. [9] Jalalpoor, Sh., R. Kasra Kermanshahi, A.S. Nouhi, Zarkesh Esfahani, 2010. Survey Frequence of βlactamase Enzyme and Antibiotic Sensitivity Pattern in Isolated Pathogen Bacteria from Low and High Hospital Contact Surfaces. Pajuhandeh Journal., 15(2): 77-82. [10] Jalalpoor, S., R. Kasra-Kermanshahi, A. Nouhi, H. Zarkesh-Esfahani, 2011a. Frequency of β-lactamase enzyme and antibiogram pattern in bacterial flora isolated from staffs hands. Zahedan J Res Med Sci (ZJRMS) 13(7): 44-49. [11] Jalalpoor, Sh., 2011b. Frequency of Beta Lactamase Enzyme in Isolated Pathogen Bacteria from Hospital In-Vivo and In-Vitro Condition. Journal of Isfahan Medical School, 29(131): 1-9. 3554 Shila Jalalpour Advances in Environmental Biology, 7(11) Oct 2013, Pages: 3549-3554 [12] Jalalpoor, Sh., 2011c. Survey beta lactamase production and resistance pattern into beta lactame antibiotics in Bacillus cereus strain isolated from staff hands and hospital environment in Iran. Afr. J. Microbiol. Res., 5(19): 2980-2985. [13] Jalalpour, Sh., 2011d. Emergence of Antibiotic Resistance Nano Enzyme in Staphylococcus species Isolated from Clinical, Biotic and Abiotic Conditions. Biomed. & Pharmacol., J 4(2): 365-371. [14] Jalalpour, Sh., 2011e. Prevalence of Beta Lactamase Nano Enzyme in Bacteria Isolated from Staff Hand (Isfahan-Iran). J. Pure & Appl. Microbiol., 5(2): 1045-1050. [15] Jalalpour, Sh., 2011f. Food Borne Diseases: Healthcare Staff, High and Low Hospital Contact Surfaces. Australian Journal of Basic and Applied Sciences, 5(8): 903-905. [16] Jalalpour, Sh., 2012. Food borne diseases bacteria; frequency antibiotic resistance bacteria in Iranian foods. Afr. J. Microbiol. Res., 6(4): 719-723. [17] Jay, J.M., 2000. Modern Food Microbiology. Gaithersburg, MD: Aspen Publishers. [18] Joffe, A.Z., B. Yagen, 2007. Comparative study of the yield of T-2 toxic produced by Fusarium poae, F. sporotrichioides and F. sporotrichioides var. tricinctum strains from different sources. SAGE. Publications.Availableat:http://het.sagepub. com/cgi/content/ abstract/20/2/84. [19] Liu, G.Y., A. Essex, J.T. Buchanan, V. Datta, H.M. Hoffman, J.F. Bastian, J. Fierer, V. Nizet, 2005. Staphylococcus aureus golden pigment impairs neutrophil killing and promotes virulence through its antioxidant activity. J Exp Med., 202(2): 209-215. [20] Liu, C.I., G.Y. Liu, Y. Song, F. Yin, M.E. Hensler, W.Y. Jeng, et al., 2008. A cholesterol biosynthesis inhibitor blocks Staphylococcus aureus virulence. Science, 31(5868): 391-94. [21] Matthews, K.R., J. Roberson, B.E. Gillespie, D.A. Luther, S.P. Oliver, 1997. Identification and Differentiation of Coagulase-Negative Staphylococcus aureus by Polymerase Chain Reaction. Journal of Food Protection., 60(6): 686-688. [22] Mazur, J. Lynnette, J. Kim, 2007. Spectrum of Noninfectious Health Effects From Molds . American Academy of Pediatrics. Available at: http://pediatrics. aappublications.org/cgi/ content/full/118/6/e1909. [23] Mead, P.S., 1999. Food-related illness and death in the United States. Emerg Infect Dis., 5(5): 607-25. [24] Patel, A.H., P. Nowlan, E.D. Weavers, T. Foster, 1987. Virulence of protein A-deficient and alpha-toxindeficient mutants of Staphylococcus aureus isolated by allele replacement. Infect Immun., 55(12): 31033110. [25] Schneewind, O., A. Fowler, K.F. Faull., 1995. Structure of the cell wall anchor of surface proteins in Staphylococcus aureus. Science journal., 268(5207): 103-106. [26] Food, U.S. and Drug Administration, 2008. Bad Bug Book. Foodborne Pathogenic Microorganisms and Natural Toxins Handbook. Available at: www.cfsan.fda.gov/~ mow/ intro.html. [27] Department, U.S. of Agriculture Food Safety and Inspection Service, 2006. Basics for Handling Food Safely. Available at:www.fsis.usda.gov/PDF/Basics_for_ Safe_Food_ Handling.pdf. Accessed 5/18/08. [28] Washington, C., A. Stephen, W. Janda, E. Koneman, G. Procop, P. Schreckenberger, G. Woods, 2006. Koneman's Color Atlas and Textbook of Diagnostic Microbiology, 6 ed .USA :Lippincott wiiliams and wilkins., pp: 775-779. [29] Whitt, Dixie, D., A. Abigail, 2002. Bacterial Pathogenesis: A Molecular Approach (2nd ed.). USA: ASM Press. ISBN 1-55581-171-X. [30] Zhu, J., C. Lu, M. Standland, 2008. Single mutation on the surface of Staphylococcus aureus Sortase A can disrupt its dimerization. Biochemistry, 47(6): 1667-1674.