* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
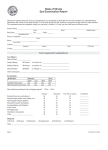
Download MBBS Programme Phase 3 Student Logbook 2012-13
Survey
Document related concepts
Transcript
School of Medicine If found please return to: Phase 3 Undergraduate Officer Academic Centre Henriette Raphael House Guy’s Campus SE1 1UL MBBS Programme Phase 3 Student Logbook Rotation A: Basic adult medicine and surgery including gastroenterology, urology, nephrology, and endocrinology 2012-13 Student name __________________________________________ You must submit your completed Logbook to the Academic Centre by Term 1: 4pm Monday 17th December 2012 Term 2: 4pm Monday 25th March 2013 Term 3: 4pm Monday 15th July 2013 A completed Logbook, with all clinical skills signed and all professional development, firm head and clinical adviser sections signed for each Rotation, is a requirement for progression from Phase 3 into Phase 4. A student who fails to submit a completed Logbook by the due date will be required to take the end-of-year OSCE Please ensure you photocopy the pages for skills sign-ups and clinical adviser meetings before submitting the Logbook, and keep a copy for your own reference. END-OF-ROTATION IN-COURSE ASSESSMENT (ICA) MARKS Grand Round Marks and Firm head marks are all recorded in this logbook on p.31 and p.32. GP marks are submitted directly to the Academic Centre by the GP. It is your responsibility to ensure these marks are completed. PLAGIARISM Your attention is drawn to the College statement on plagiarism, a copy of which you will have signed at enrolment. A copy will also be available on the Virtual Campus. This statement covers all work that you will submit for assessment (including all completed SSC submissions in later years where you will be required to sign a statement confirming that you have not plagiarised any of the material contained therein). You are strongly reminded that any breach of these rules by you will be the subject of the College’s disciplinary procedures and could result in the termination of your studentship. Furthermore, an act of plagiarism is by its very nature dishonest and could bring into question your fitness to practise. FALSIFYING A LOGBOOK SIGN-UP IS FRAUDULENT AND SHALL LEAD TO DISCIPLINARY ACTION The information contained within this Logbook is correct at the time of going to press although the details may change before or during the academic session. Contents Part 1 – Important Information 1. Introduction p. 2 2. Educational Contract for Phase 3 p.5 3. Confidentiality Code p.7 4. Clinical Adviser Visits p.8 5. Digital Professionalism p.9 6. Feedback p.10 7. Career Reflections p.11 8. An Important Notice about Infection Control p.12 9. Code of Practice for Student Examination of Patients p.18 10. Fitness to Practise p.24 11. Simulated and Interactive Learning (SaIL) p.25 Part 2 – Skills and Sign-ups 12. In-Course Assessment of Clinical Skills: Guidance for Students • • In-course marking scheme and performance descriptors In-course Assessment Marksheets p.27 p.28 p.31 13. Sign-Ups p.33 14. Additional Mandatory Experiences • Basic Life Support (BLS) • Pathology and Therapeutics • Interprofessional Education • Ethics Report • Patient Educator Sessions p.57 15. Patients Clerked p.61 16. Phase 3 Core Patient Cases p.63 17. Integrated Skills List p.68 18. Quick contacts list p.74 1 1 – Introduction This is one of a series of Logbooks for the MBBS course that aims to link skills training across all Phases and prepare for your early professional career as a doctor. The Logbook provides a record of the competences you achieve in the essential skills in this rotation, sign-up of the KCL School of Medicine Student and Doctor, Educational Contract for Phase 3, Confidentiality Code, professional development, and visits to your clinical adviser. You will be asked to hand in your Logbook at the end of the year for inspection of satisfactory completion of skills and authenticity of signatures. Because each year Logbooks are mislaid, you are advised to photocopy all pages with skills sign-ups and clinical adviser visits regularly and before handing in. Gaining competence in skills Skills are an important part of the work of a doctor. The best way to learn skills is to progress through a cycle of learning by observing an expert perform a skill, perform it under supervision, and then practise several times on your own. When you feel competent, ask to be observed for your sign-up. If your assessor believes you are not competent for sign-up, you will need further practice and reassessment later in the rotation. You should revisit skills during the medical course to maintain your competence. They are assessed in subsequent years’ OSCEs. Keeping your skills up-to-date Clinical practice is constantly changing. New skills are introduced and others change in technique or equipment used. It is your responsibility to keep up-to-date with changes and to modify your skills technique accordingly. This is especially important for skills such as BLS. In subsequent OSCEs, you will be assessed on the updated skills techniques not the method you initially learnt. Specific learning outcomes in Phase 3 During Phase 3 students should learn to perform a general clinical assessment of an adult patient, comprising: full history (including review of systems), general physical examination and specific examination of associated systems, and mental state and cognitive state examinations. In addition, students should learn about selecting and interpreting tests and investigations, performing clinical procedures, and presenting their findings. They should learn to evaluate clinical and pathological information to generate a differential diagnosis and use this to initiate clinical management (including practical management such as resuscitation, and medical treatment with medication). Students must be able to check the correctness of existing prescriptions for medication; they must also be able to write simple prescriptions (including ascertaining allergies and drug sensitivities, and drug dosage, contraindications and interactions using the British National Formulary). Students should be able to explain to patients (or their carers) the nature of their diagnosis, any investigations or procedures they may require, and the common treatments (medical, surgical or psychological) they might receive. Most students should expect to achieve basic competence in these tasks by the end of the first term, and all students may be tested on any aspect of these tasks during the third term. The sign-up skills constitute the minimal skills to be learned in Phase 3: they are necessary but not sufficient for the complete clinical assessment and management of the adult patient. Therefore they do not constitute a syllabus for the incourse OSCEs nor the end-of-year OSCE. 2 1 – Introduction Sections 2-3 – Educational Contract for Phase 3; Confidentiality Code (pp. 5-7) This section contains important documents that you must read carefully and discuss with your clinical adviser. They must be signed (and countersigned by your clinical adviser where necessary) before you commence your first clinical placement. Section 4-5 – Clinical Adviser Visits; Digital Professionalism (pp. 8-9) This is a record of visits to your clinical adviser. You should see him or her at least once per term. Your adviser is invited to write notes on any points to be followed up at future visits, including your reflections on careers. Please take your Logbook with you to these visits. They must also sign that you have completed the on line Digital Professionalism module. Section 9 – Code of Practice (pp. 18-23) This section contains guidelines for general examination and intimate examination of patients. You should be aware of these guidelines and comply with them at all times. Sections 12-13 – Marksheets, Skills and Sign-ups (pp. 31-56) Grand Round Marks and Firm head marks are all recorded in this logbook. This is the official record of your sign-up of skills for your year. In Phase 3 there are three Logbooks one for each rotation. You should get your clinical skills and your attendance at special clinical sessions signed up by the end of each rotation by a doctor or other clinician (such as a nurse specialist) appropriate to the specialty and approved by your firm head. A copy of the integrated skills list for all years of the MB BS programme is on the Virtual Campus. Section 14 – Additional Mandatory Experiences (pp. 57-60) Basic Life Support Pathology and Therapeutics Interprofessional Education, Ethics Patient Educator Sessions Section 15 – Patients Clerked (pp. 61-62) This is a record page for you to list clinical cases you have clerked and examined. It should be used for discussion with your firm head and for revision. Patients vary, so you should aim to clerk several patients within each diagnostic category, and a minimum of two patients each week. You should ensure you clerk patients whose diagnosis is not known to you, so that you can develop your differential diagnostic skills. Section 16 – Core Patient Cases (pp. 63-67) Core cases and procedures form the basis of adult clinical medicine encountered in Phase 3. You should try to clerk patients with each of these conditions or undergoing the named procedures in order to build up your clinical knowledge and skills. You should observe the management of emergencies and the performance of clinical procedures – you will see some of these only on acute “take”. Whenever you have clerked a patient with one of these conditions, or observed a procedure, you should read about it so that you understand it fully. You must also attend post-mortem examinations regularly throughout the year. 3 1 – Introduction Attendance and satisfactory sign-up You are expected to attend all teaching whether lectures, practicals, tutorials, symposia or clinical teaching. During clinical placements, clashes may occur between scheduled clinical (i.e. involving patients) and nonclinical (e.g. formal lectures or symposia) teaching: normally, clinical teaching takes priority, but you must follow your firm head’s instructions. Your firm head will take your attendance into account when signing-up your satisfactory completion of the rotation in your Logbook. Genuine mitigating circumstances such as illness or official absence will also be taken into account. Attendance of at least 90% is expected at all course components and attendance of at least 75% is required to pass any course component. Name Badges You are expected to wear your School of Medicine ID badge at all times in hospital and GP premises, in community settings and on home visits. Dress Code NHS trusts operate mandatory dress codes that must be followed at all times when on NHS sites. See the Virtual Campus for more details on the dress codes required by each trust. 4 2 – Educational Contract for Phase 3 Name of student: Your firm head has overall responsibility for your placement, timetable organisation, and your clinical supervision. The site/campus Sub-Dean and Head of Phase 3 have overall responsibility for placements. At the outset of the attachment you will be given information about the expectations of the attachment, including on-call periods. If you have any commitments that conflict with these you must make them known to your firm head and agree how this will be managed. You should comply with all aspects of the KCL School of Medicine Student and Doctor (see Handbook), particularly: develop skills by: • • • • • • attending and participating in learning opportunities reflecting on and addressing personal learning needs learning to communicate effectively with patients, relatives and professionals working cooperatively with patients, peers, teachers and healthcare staff becoming proficient in essential clinical examination skills becoming proficient in essential practical procedures and demonstrate appropriate attitudes by: • • • • • • treating patients with politeness and consideration, learning to involve them in decisions about their care acting honestly with patients, peers and staff showing respect for patients, relatives and colleagues that encompasses, without prejudice, diversity of background, language, culture and way of life recognizing the rights of patients and acting in their best interests, particularly with regard to confidentiality, informed consent, autonomy and dignity recognizing the need for guidance and supervision and the limits of personal competence and health respecting the professional values of competence in performance, reliability and conduct. Guidance on meeting the requirements of the Educational Contract 1. Patients: you will be expected to take histories and examine patients in inpatient, outpatient and community settings throughout the attachment with a minimum of two patients clerked and examined fully every week. 2. Skills: you will be expected to learn and practise the skills listed in the Logbook before having your competence validated by an appropriate health professional. 3. Identity: during interactions with patients and staff you should always wear you name badge and identify yourself as a Medical Student. 4. Dress Code; you must abide by the dress code and infection control procedures for the NHS Trust to which you have been allocated. 5 2 – Educational Contract for Phase 3 Name of student: 5. Patient records and consent: all entries you make in patient records must be signed, dated, and your name and status as “medical student” printed legibly. The patients whom you will look after will be asked to give their permission for your involvement. It is always a patient's right to decline to be seen by a medical student. 6. Ill health: if you are unable to attend because of ill health, you should inform your firm head as soon as possible. The School of Medicine will expect you to submit to the Academic Centre a suitable sickness certificate (self-certification for less than five working days, medical certificate for five days or longer). There is no holiday leave during the attachment; holidays are built in to the Phase 3 timetable. 7. Potential complaints: if you are in a situation where you have any reason to think a complaint might be made against you, you are concerned by a patient’s comments, or believe you may have acted inappropriately, you should discuss this with your firm head, another senior clinician or your clinical adviser as soon as possible. Resolving a problem quickly shows respect for your patient (and is much less likely to result in a formal complaint being made). 8. Education supervision: if you have any concerns over the supervision you are receiving, you should take this up with your firm head, the site Sub-Dean, the Head of Phase 3 or if the advice you seek is of a more personal nature, with your Clinical Adviser. 9. Professional indemnity: the School of Medicine requires all student to be a member of a medical defence organisation during the whole undergraduate course including Phase 3. If you follow the guidance in this contract it is difficult to envisage any legal action which would not be covered vicariously through your consultant. However, the defence organisations would cover you if this unlikely event arose and also provide additional support. You should be aware that the medical school has no responsibility to provide cover for students in such situations. I accept and agree to abide by the conditions of the Educational Contract Student: Signed………………..…………………….…..… Date……………….. Clinical Adviser: Signed………………..…………………….…..… Date……………….. GMC no./Designation…………………………………………... Rotation 1 firm head: Signed…………………………………………..… Date……………….. GMC no./Designation………………………………………….. Rotation 2 firm head: Signed…………………………………………..… Date……………….. GMC no./Designation………………………………………….. Rotation 3 firm head: Signed………………..………….……………..… Date……………….. GMC no./Designation…………………………………………. 6 3 – The School of Medicine Confidentiality Code Name of student: You MUST sign the declaration below AT THE START of the first term, in discussion with your Clinical Adviser; this is required by the NHS trusts before you are permitted to see patients. Why is patient confidentiality important? Confidentiality is central to the trust between patients and doctors and is part of the professional code. Patients have a right to expect that medical students and doctors will not pass on confidential information without their consent except to other health professionals who care for them. Confidentiality should be maintained for all time even after a patient's death. What is confidential information? How should you protect it? Confidential information includes all personal details by which a patient is identifiable such as name, address and full postcode. Such data should not be transmitted verbally, in writing, or online r without a patient’s consent. Confidentiality extends to casual social conversation, including emails, blogs and social media. Do not discuss patient details in public places such as hospital lifts, cafeterias, and public transport. Confidential information used for teaching, projects, research or audit must be anonymized. Confidentiality may only be breached in exceptional circumstances. Discuss this with your tutor. Anonymizing data. What should you do? Patient identifiable information is anonymized by removing the patient's name, address, post-code, date of birth, NHS number, telephone number or other information that allows access to the patient. For electronic processing, do not enter patient identifiable information onto your PC. Data entered in a clinical setting, such as hospital or GP practice, must be password protected. Destroy all personal information if not needed. Delete on PCs and on handheld mobile internet enabled devices. For paper, consign to a bin designated for disposal of confidential information. These are located in Academic Centre or in clinical departments. Do not photocopy clinical notes for projects, presentations, or for other reasons. All information removed from a clinical area must be anonymized and secured in a folder or case. Obtaining patient consent. What does this mean in clinical practice? If it is for the patient’s benefit, information can be shared with the multidisciplinary team caring for the patient. This does not extend to research, teaching or unqualified staff. Always obtain the patient’s consent orally or in writing before you give personal information to a third party such as family or friend who is attending with the patient. You must obtain written informed consent from patients before taking photos. The patient must be unidentifiable and you should not take photos of patients using a mobile phone. Obtaining patient consent. What does this mean for projects and presentations? If you use patient data for projects never include patient identifiable information. If you use clinical material, explain to the patient how data will be used and assure him or her that information will be anonymized. If you photograph a patient for a project, explain how the photo will be used, obtain written consent and that of your supervisor’s. For presentation or publication, the patient's eyes must be occluded. Carefully consider whether metadata on any images you have taken break patient confidentiality. Remember • • • Every patient has a right to confidentiality Every student has an obligation to respect that right Breaching confidentiality is a College disciplinary offence NB: To be signed at the start of the first rotation in discussion with your Clinical Adviser I have read and understood the School of Medicine Confidentiality Code Signature of student …….………………………………………………...….. Date …………………… Signature of clinical adviser ……………………………………………...… Date …………………… GMC no./Designation………………………………………………………………………… 7 4 – Clinical Adviser Visits Name of Clinical Adviser: Name of student: You are advised to see your clinical adviser following your mid-rotation interview with your firm head to discuss the following Term 1 Campus: □ Confidentiality Code signed – Rotation 1 (p7) □ Skills sign-ups reviewed (may not be complete) □ List of patients clerked and reviewed (optional) □ Attendance / Health □ SSCs (Poster Presentation phase 5 only) □ Responsible use of social media □ Foundation Programme application discussed (phase 5) □ Career ambitions discussed □ Consent issues (Code of practice for examination of patients - see p18-23) □ Exam performance and OSCE feedback □ Professional development (including interprofessional education) □ Fitness to Practise concerns □ Educational Contract discussed and signed □ Transfer/ returning students: issues Clinical Adviser: Signed …….………………………………………………...….. Date …………………… GMC no./Designation………………………………………………………………………… Comments: Term 2 Campus: □ Skills sign-ups reviewed (may not be complete) □ List of patients clerked and reviewed (optional) □ Attendance / Health □ SSCs & electives □ Discuss an ethical experience from Term 1 (p.59) □ Ethical report (phase 3 only) □ Review clinical grades □ Professional development (including interprofessional education) discussed □ Foundation Programme application discussed (phase 4 and 5) □ Career ambitions discussed □ Fitness to Practise concerns □ Educational Contract signed Clinical Adviser: Signed …….………………………………………………...….. Date …………………… GMC no./Designation………………………………………………………………………… Comments: Term 3 Campus: □ Skills sign-ups reviewed (may not be complete) □ List of patients clerked and reviewed (optional) □ Attendance / Health □ Educational Contract signed □ Professional development (including interprofessional education) discussed □ Review clinical grades □ Foundation Programme application discussed (phase 4) □ Career ambitions discussed □ Fitness to Practise concerns □ Exam performance, OSCE feedback and revision □ Electives (phase 3 &4) Clinical Adviser: Signed …….………………………………………………...….. Date …………………… GMC no./Designation………………………………………………………………………… Comments: 8 5 – Digital Professionalism Evidence must be shown that the module has been completed during Phase 3. I have seen evidence that the student has completed the on line Digital Professionalism module at http://virtualcampus.kcl.ac.uk/vc/tel/social_media_guidance Signature of Clinical Adviser .…………………………………………………… Date …………………………………………………………………………………… 9 6 – Feedback Receiving feedback from your course tutors and other teachers Throughout the medical course, you will receive feedback on your work and clinical performance. Feedback if used constructively helps improve your standards. The GMC’s guidance in Good Medical Practice states that “you must reflect regularly on your standards of medical practice and respond constructively to the outcome of appraisals and performance reviews”. <www.gmc-org.uk>. Why is feedback important? Feedback and self-critical appraisal on your performance helps gauge your progress. Knowing what you do well and how you could improve will build self-confidence. Feedback on your performance in assessments will help identify your strengths and weaknesses and enable changes to be made. Receiving and accepting feedback constructively will be important throughout medical school and in your professional life. How can I ask for feedback in the clinical environment? There are several sources of potential feedback on your performance. Decide what you would like feedback on. Be specific on the points you feel need improving, then ask for feedback from an observer. Patients, peers and your clinical tutors are a useful source of feedback. Use the skills performance criteria in the Logbooks to assess your own performance. Useful questions: • • • How do you think I did with my history taking/ examination/ specified skill? Am I up to standard in this skill or procedure? How can I improve in this skill? How should I react to receiving feedback? Ways of giving feedback vary. Indeed giving constructive feedback is a difficult skill. Receiving feedback requires a professional attitude that you need to develop as a student in readiness for your medical career. So… • • • • • Listen carefully. Be sure you have understood the feedback. If not, clarify. Thank your teacher or observer for their feedback. Avoid being defensive. Ask for an explanation if you feel the comments are too critical. Ask yourself if you reacted appropriately? It is unprofessional to argue with the tutor giving feedback and to reject their comments. Use the feedback to improve your performance. Your feedback and sign ups The sign-ups section in this book includes space for the clinician assessing each skill to comment on your strengths and areas for improvement. You are encouraged to make use of this opportunity for receiving feedback and to record comments in the space provided. 10 7 – Career Reflections Reflecting on the range of career options in medicine Drawing on your experience of the different specialities in your course, start to think about the options for your medical career and your aptitude for each speciality. Use this page to make notes and refer to them in discussion with your clinical adviser. In relation to each speciality ask yourself the following questions: • • • • • What aspects did I enjoy and why? What aspects did I dislike and why? What information have I found out on careers in this speciality? What more do I want to find out about this speciality? How will I do it? Am I suited to working in this speciality? You are strongly encouraged to look at the Medical Careers website: http://www.medicalcareers.nhs.uk/medical_students/introduction.aspx 11 8 - An Important Notice About Infection Control In Clinical Practice The exact infection control regulations enforced in hospitals vary from Trust to Trust, but the following infection control guidelines should be acceptable at all hospitals. Each Trust will have its guidelines on its ward computer system (intranet). Students (and staff) can readily become colonised with pathogenic bacteria and viruses during close contact with patients. Even a brief examination can be responsible for the spread of MRSA, coliforms and enteric viruses. These can cause severe harm to patients. Also, occasionally students and staff may be infected by these pathogens, and, very rarely, Hepatitis B, C HIV and HTLV 1. These brief guidelines are intended to help you to know what to do in different clinical settings. Note also that infection control practice is an integral part of many OSCE assessments. If you are unwell – e.g. diarrhoeal illness, severe cold or any febrile illness – do not go on the wards. If you have a mild cold without fever – do not visit immunocompromised patients. Ask a senior member of the ward staff, or the Hospital Infection Control & Prevention team, if in doubt. Important organisms that may be transmitted in health care Main means of spread Hepatitis B & C, HTLV-1 and HIV Inoculation injuries with sharps and exposure from splashing of body fluids onto mucous membranes Respiratory route/close contact. Are you immune? Hands, faeco-oral route, food Varicella zoster virus (chickenpox & shingles) Diarrhoeal diseases e.g. Norovirus, Rotavirus, Salmonella, Shigella Resistant Gram negative bacteria e.g. Klebsiella (especially ‘ESBL’ strains) Environmental organisms e.g. Pseudomonas Mycobacterium tuberculosis Clostridium difficile colitis Methicillin-resistant Staphylococcus aureus (MRSA), sensitive Staph aureus, Group A streptococci Hand/patient contact Via hands or via equipment e.g. instruments left wet overnight Respiratory route Environmental & hand spread (+antibiotics) Via staff carriers, hands, environment Practical Guidelines for Day-to-day Infection Control White Coats etc Please refer to the dress code on page 18 and of the Trust where your firm is located. Hand washing with Soap & Water at a ward or Clinic Sink using the seven stage technique. • • • • • • At the beginning of the day Before and after examining a patient After doing a procedure which might have contaminated your hands (including glove removal) If your hands look dirty e.g. oil/ink staining On a ward round if patient examined/hands contaminated/cubicles visited. If the patient has known or suspected infection with Clostridium difficile or Norovirus (alcohol is ineffective against spores and most enteric viruses). 12 8 - An Important Notice About Infection Control In Clinical Practice Hand Disinfection with Aqueous Chlorhexidine (or Iodine) or Alcoholic Preparations such as Hibisol, or Alcohol Gel Sink using the seven stage technique. First remove any visible contamination (if present) with soap & water • • • • • If you have contaminated your hands with blood and body fluids Before and after dealing with immunocompromised patients (especially in Protective Isolation) and with patients in Standard or Strict Isolation Before doing clinical procedures e.g. venepuncture, IV line insertion, catheterisation Alcohol preparations as an alternative to soap and water washing if no sink is available. See note above about not using alcohol for patients with Clostridium difficile & Norovirus 13 8 - An Important Notice About Infection Control In Clinical Practice 14 8 - An Important Notice About Infection Control In Clinical Practice In the Operating Theatres Ask for advice if in doubt. Change out of outdoor clothing except for underwear (remove socks/stockings) Change into theatre top + trousers, or tunic; clogs, head covering (balaclava-style if long hair) and filtering mask. Remove watch and jewellery, & wash hands. Put up mask on entering operating area of theatre. Now you are part of the “circulating team”. If asked to scrub up: nail brushing; three-minute surgical wash with aqueous chlorhexidine or povidone iodine up to & just above the elbows (do not scrub the skin with a nail brush). Don’t touch anything non-sterile with sterile gloved hands. Then put on green sterile gown and gloves. Now you are part of the “scrub team”. Entering Side Rooms with Patients in Isolation Note instructions sign on the door. If relevant, take off white coat & leave outside; put on plastic pinafore and gloves; mask for particularly infectious cases (ask!). Dispose of mask and apron into the orange plastic sack, as you are leaving the room, then wash hands before leaving the room (removing protective clothing can contaminate the hands). Use alcoholic hand rub afterwards (outside the room), or wash at a sink again if none present. Barrier Nursing on a main ward (“Cohort nursing”) This is sometimes required when there are no side rooms or if several patients have for example MRSA or a multi-resistant Gram negative pathogen. Gloves and a plastic apron may need to be worn with attention to hand hygiene afterwards. If in doubt ask a senior nurse. Needles & Sharps Used disposable needles & sharps: They always go in a sharps bin. Always dispose of sharps, & needle holder if used, at the point of use.BEWARE OF OVER FILLED SHARPS BINS. DO NOT CARRY EXPOSED SHARPS THROUGH THE WARD. If possible use a mobile sharps container and tray, and take these to the patient. DO NOT RE SHEATH NEEDLES. [If a needle must be re-sheathed, e.g. re-sterilisable steel cannula, use a single handed technique.] It is your responsibility to dispose of your own sharps. Never leave them on a tray for someone else to dispose of. Reusables: e.g. surgical instruments: Place in plastic tray on trolley or as directed by assistant. These re-usable instruments must never be cleaned by you (high risk of injury) but placed in a special bin for return to the central sterilisation department. Ask if in doubt. Gloves Sterile for surgery & invasive clinical procedures; non-sterile are OK for dressing changes and other ‘dirty’ procedures. Latex and vinyl gloves are available on all wards and departments in small, medium and large sizes. Ill-fitting gloves can be a hazard during procedures. Allergy to latex does occur; get advice from Occupational/Student Health. Plastic Bags These are ORANGE for clinical waste i.e. items stained with blood or body fluids, and double-bagged YELLOW for certain specialist items like dialysis equipment. CLEAR or BLACK for domestic-type waste i.e. drinks cans, paper packaging, hand towels used after social (soap & water) hand drying. NEVER put broken glass, sharps & needles in plastic bags or laundry bags. Use SHARPS BINS. There are special bins for non-contaminated broken glass. 15 8 - An Important Notice About Infection Control In Clinical Practice Spillages of Blood & Body Fluids If No Broken Glass Involved: Get someone who knows what to do. Each ward has a yellow spillage kit. Mark off the area and prevent people walking through it. Open a window if possible because chlorine-based disinfectants can give off chlorine. Wearing plastic apron & gloves, clear up the majority of the spillage with paper towels (place them straight into an orange bag). Sprinkle NaDCC (i.e. sodium dichloroisocyanurate – which is similar to hypochlorite or bleach) granules onto the spillage area. Leave 3 minutes then clear up with scoop & paper towels, rinse area with water. (ALTERNATIVE: use 1% NaDCC solution (1 in 10 neat NaDCC, = 1 in 10,000 ppm available chlorine) poured onto paper towels. 3 minutes later clean up with more paper towels. Everything goes into an orange plastic bag for incineration. The local cleaning contractor should clean the disinfected area to remove excess residue of NaDCC. TOO MUCH BLEACH & SPILLAGE FLUID = CHLORINE GAS HAZARD! – always open windows before starting to clear up the spillage; Caution: bronchospasm risk for asthmatics. If Broken Glass is Present in the Spillage: Disinfection as above: Get help. Never never never pick up broken glass with fingers, even if wearing gloves - sharps injury will occur! Use a plastic scoop provided in the spillage kit. Discard broken glass into a sharps bin. Then proceed as above. Resources: Ask any trained nurse or clinician about hand disinfection. Infection control nurses are present in all hospitals. An infection control CAL program (‘ICTAP’) shows good hand disinfection technique and much more, it is available on the KCL server; similar e-learning programs are available at most Trusts. 16 8 - An Important Notice About Infection Control In Clinical Practice What to do if you have a percutaneous or mucosal exposure to potentially HIVinfected blood or other high-risk body fluid: In all cases – whether the patient is known to be high risk for any infection or not • Encourage the wound to bleed, ideally by holding it under running water • Wash the wound using running water and plenty of soap • Don’t scrub the wound while you are washing it • Don’t suck the wound • Dry the wound and cover it with a waterproof plaster or dressing • Mucosal splash (eye, mouth): rinse with a lot of sterile water or saline for 10 minutes • Note name number and location of ‘donor’ patient, if known. Notify a senior person in the ward or clinic. • Attend Occupational Health IMMEDIATELY AND ALWAYS WITHIN AN HOUR IF AT ALL POSSIBLE. OUT OF HOURS attend ACCIDENT & EMERGENCY; report a ‘needlestick injury’ and you will be seen quickly. • The Occupational Health Department or the A & E Department (via the Virologist. Medical Microbiologist, or HIV/Infectious Disease Physician on duty) should arrange for the patient's blood to be tested for HIV (and HBV and HCV) with the informed consent of the patient. • Fill out an incident form (later). Keep a copy of the accident report. • When advised to do so, take a single dose of the anti-HIV drugs as soon as possible, ideally within one hour of the incident. There is unlikely to be any benefit if HIV PEP is started >72 hrs after the incident. This one dose is unlikely to give side effects. If the exposure is to blood or body fluids/tissues from a patient shown to be or strongly suspected of being HIV positive, you should continue to take the anti-HIV drugs for four weeks, according to the prescription details, with monitoring. You will need to be followedup by the Occupational Health Department, a senior HIV/Infectious Disease Physician, or a Medical Microbiologist or Virologist. • If you have been at risk of acquiring HIV infection, you should use condoms and refrain from donating blood until a blood test at 6-7 months confirms that you are uninfected. 17 9 - Code of Practice for Examination of Patients by Students Basic professional requirements for students on clinical practice (see Educational Contract) Interviewing patients Dress Code Each NHS trust has its own dress code, but the following principles apply in most trusts. Dress should be professional and appropriate to the specialty. Dress code excludes excessively casual clothing such as jeans, shorts, baseball caps and trainers. Avoid wearing revealing clothing as this may embarrass patients. Most commonly health care workers wear uniforms or tunics, or short-sleeved shirts/blouses and no ties. (If the medical firm or hospital where you work still requires white coats, make sure your white coat is always clean - change it regularly.) Ties (if worn) should be tucked into the shirt about half-way down. If you don’t have short-sleeved shirts/ blouses, roll up the sleeves above the elbows for surgical cleansing and procedures. Wrist watches, wrist bands and jewellery should be removed before work (bare below the elbows). Nails should be kept short and clean, with no nail varnish or false nails. Long hair should be tied back. Clothing should be of a type that can be hot-washed, i.e. above 60oC, so any pathogens are killed off. It is unprofessional to chew gum, eat, or drink in the patient’s presence. Special Groups of Patients Nervous patients Nervous or embarrassed patients may be apprehensive about being interviewed. Students should be alert to signals of distress from patients; you should apologise and discontinue under these circumstances. Adults with cognitive impairments or learning difficulties Adults with cognitive impairments or learning difficulties should be treated as fully consenting with the capacity to decide whether to consent or refuse. As with all patients, it is essential to show respect and privacy. Children and adolescents When interviewing a child or adolescent under age 16 years, always obtain permission from the parent or guardian and ask them to be present throughout the interview. Children are easily upset and need reassurance from their family; they are taught not to talk to strangers and are generally suspicious of unfamiliar faces. Be aware that child abuse or mishandling is a real fear for parents; students should avoid situations where their intentions can be misinterpreted. Ethnic, cultural and religious groups Expectations vary according to individual circumstances, but remember that some Muslim and Hindu women may have have a clear preference for women practitioners when intimate examinations are necessary due to their strong religious beliefs. Male students examining women from these cultural groups should have a chaperone at all times. The Islam, Hindu and Orthodox Judaism religions have specific beliefs regarding menstruation so a gynaecological examination during menstruation may be considered unacceptable except in an emergency. Verbal consent for any physical examination is imperative regardless of creed. Visiting patients at home Tutors are asked to consider your safety and security whenever you are visit patients at home. You may be paired with another student or alternative arrangements should be agreed with a member of staff. Discuss with your tutor if you have any concerns. Recommended reading General Medical Council. “Good Medical Practice”. www.gmc-uk.org 18 9 - Code of Practice for Examination of Patients by Students Protocol for Intimate Examinations of Patients by Students in Healthcare Professions The recommendations of the protocol apply in most NHS trusts in which you will study. You should check the details with your firm head. For all patients, capacity to give consent must comply with the Mental Capacity Act 2005. Introduction Consultations with healthcare professionals, examinations and investigations are potentially distressing for patients when involving intimate areas of the body. Acceptable professional behaviour, good communication, and respect for patients’ rights to be fully involved in decisions about their care will reassure patients and avoid misunderstanding. Complaints are not infrequently made that health professionals have behaved improperly or roughly when undertaking intimate examinations or invasive procedures. Students in healthcare professions are at similar risk. For your patients’ and your own protection, you should follow this protocol when performing intimate examinations. These include: • • • • vaginal examination and inspection of the perineum rectal examination of both sexes examination of female breasts examination of external male genitalia Requirements for intimate examinations First practise the examination on a model, mannequin, or a patient educator. Before examining a patient, you must have approval from your clinical supervisor at the time of the examination. For all vaginal and rectal examinations and first examinations of female breasts or male external genitalia, you must examine the patient in the presence of your supervisor The patient must have a chaperone. You should obtain the patient’s permission and explain that this will be recorded in the patient notes, as follows; • • Verbal permission for examination with the patient awake Written permission for examination under anaesthesia, using a student form Patient consent for examinations and invasive procedures It is a requirement of clinical practice that consent for any procedure is obtained from patients by the clinician with responsibility for their care and that the patient is adequately informed about the procedure, possible risks and consequences, and alternative management options. This is known as informed consent. Giving consent requires the patient to have sufficient mental capacity. Consent can be verbal or written and must be given voluntarily. Students in training are not legally qualified to obtain informed consent from patients but must obtain the patient’s agreement for history taking and examination. Preparing patients for an intimate examination Having obtained the patient’s consent, explain what is involved and whether the patient has previous experience of the examination, whether the experience was painful and if so discuss with your supervisor. Offer an opportunity for questions and discussion, and supplement with an information leaflet if availableremember patients need time to reflect on information. Explain that patients have choices and that declining an examination will not adversely affect care. Explain that your supervisor will be present during the examination. Requests for gender specific practitioners are often based on cultural beliefs and should be respected. Avoid examining women during menstruation except in an emergency. You should also be sensitive to the 19 9 - Code of Practice for Examination of Patients by Students potential for embarrassment or misunderstanding in other circumstances such as examining the chest of a female with exposure of the breasts, or examining the eyes by fundoscopy in a dimly lit room. Keeping good clinical records You should record the examination in the patient’s notes, state that the patient gave permission, whether your supervisor was present, whether the patient was chaperoned and if so by whom. Date and sign your entry with your name and student status clearly printed. Final year students assessed as competent in the examination should record their clinical findings as a contribution to team-care. Who should chaperone the patient? When students perform intimate examinations, the patient must have a chaperone who should be the same sex as the patient. A chaperone could be a member of staff, your supervisor, or a friend or a relative accompanying the patient.. Studies have shown that adults of both sexes prefer a nurse as chaperone, and teenagers prefer a parent. If staff are unavailable, another student may be acceptable if the same sex as the patient. If no one is available, postpone the examination rather than examine the patient alone. If asked to be a chaperone stand or sit by the patient unobtrusively and observe the procedure. If the patient is distressed, report this to the examiner and suggest the examination is discontinued. Patient examination under anaesthesia (EUA) Permission for students to gain experience during EUA must be obtained from the patient. The procedure should be explained prior to the administration of a sedative medication and the patient asked to give written agreement. Ideally this should be done in outpatients or the ward rather than in the operating theatre, but practicalities on the day of the procedure may preclude this. In some trusts, student consent forms may be available in the operating theatres, outpatients, wards, or on the trust intranet. These forms are different from the standard NHS forms used by staff when obtaining patient consent to a surgical procedure. As a student, it is your responsibility to check with your supervising clinician that the patient has agreed to the examination. It is your supervisor’s responsibility to explain the procedure and obtain the patient’s signature. Consent may be obtained in this way for up to two anonymous students for each examination or procedure. The consent form must be countersigned by your supervisor before surgery and filed in the patient notes. If student consent forms are not available, permission should be verbal and should be recorded in the patient notes. If permission has not been obtained from the patient, you must not proceed with EUA. If pressed to do so, explain to your supervisor that it is a School requirement to obtain permission. Intimate examinations during pregnancy and childbirth Student midwives and medical students are expected to participate under supervision in the care of pregnant women. This may involve vaginal examination and inspection of the perineum. The most appropriate time to discuss student involvement is during the antenatal period and should be done by the midwife or obstetrician with clinical responsibility for the patient. Written information about this may be included in the patient-held antenatal records. Giving consent is an on-going process throughout the period of maternity care. During labour and the post-natal period, it is essential that the patient is asked for permission for a named student to perform vaginal or perineal examination, and that examinations are recorded in the patient notes. Intimate Examinations of special groups of patients Some patients may not have the capacity to give consent. Students should not perform intimate examinations on the following groups: 1. 2. 3. 4. 5. Patients with severe mental illness Adults with severe learning difficulties Children and adolescents under age 16 years Non-English speaking patients Patients at home, when medical students are not accompanied by their GP tutor 20 9 - Code of Practice for Examination of Patients by Students Examination of patients at Teaching Campus Hospitals (TCH) and General Practice The same professional and ethical principles apply at TCH and in General Practice as at campus hospitals. There will be slight differences in availability and wording of student consent forms. If you are concerned about what you are being asked to see or do, discuss with your clinical supervisor or Sub-Dean. If you are not satisfied, you should raise your concerns with your clinical adviser. If you feel ill at ease about performing an intimate examination, do not proceed. Before performing an examination, check that your patient has given verbal permission. For intimate examinations, your GP tutor or clinical supervisor must accompany you. The patient should have a chaperone of the same sex, unless by mutual agreement, the patients’ partner agrees to chaperone. After the examination, record in the patient’s written or computerised notes that you examined with the patient’s permission, state; your supervisor, the arrangements for and name of the chaperone, your findings, and date and sign your entry, stating your course and year of training. Electives and clinical attachments at home and abroad The same rules and etiquette apply on clinical attachments or electives abroad. Customs and professional etiquette vary in different countries. You should be aware of local practice. In countries where healthcare is scarce, you may feel under pressure to exceed your role. Check that you have professional supervision and recognize your clinical limitations. Record, date and sign your examination, stating permission was obtained, and giving the name and status of your chaperone. Procedures in Clinical Practice Basic professional requirements for students on clinical practice1,2 Always provide privacy for the patient to undress and dress. Draw the curtains around the examination couch, checking that it is covered with clean paper. Explain which garments should be removed and where they should be placed. Do not observe the patient undressing. Ask your patient to let you know when they are ready to be examined. Explain the position for the examination. Provide a cover for exposed body areas. Keep discussion relevant to the examination; avoid personal or humorous comments. You should discontinue if you feel ill at ease, or, if the patient is uncomfortable, distressed, aroused, makes inappropriate comments, or withdraws consent. Protocol for vaginal examination (patient awake) 1. Learn and practise vaginal or speculum examination on a simulator or a gynaecology teachingassistant. These are women who train students on themselves and agree to be examined. You must be signed up for this in your Logbook before transferring the technique to a patient. When you perform vaginal examination, your clinical supervisor must be present throughout. Introduce yourself to the patient; explain your student status, course and year of study. 2. Explain the examination to the patient and obtain verbal permission. Discuss the need for a chaperone with your supervisor and if male, arrange for a female chaperone. Allow patient privacy for undressing. Explain the position for the examination. You should first examine the abdomen to put the patient at ease and to detect abnormal pathology. It is usual for the patient to be examined lying on her back (dorsal position) although occasionally, you may see a patient examined on her side (usually the left lateral position). 1 General Medical Council. Good medical practice. www.gmc-uk.org 2 Royal College of Obstetricians and Gynaecologists. Gynaecological Examinations. RCOG. London. 2002 21 9 - Code of Practice for Examination of Patients by Students 3. Before you start, check the examination tray for equipment for a vaginal speculum of correct size, lubricant jelly, examination gloves, and tissues for wiping body areas after the examination. Check the examination light is working and is in the correct position. 4. Wear surgical gloves on both hands. 5. Proceed with the vaginal examination as instructed, observing clinical etiquette. Inform your patient when you have finished, explain your findings and thank your patient. Ask your supervisor for feedback. 6. Record, date and sign the examination in the patient’s notes, stating that permission was obtained, and giving the name of your supervisor, and name and status of the chaperone. Protocol for ano-rectal examination 1. Learn and practise rectal or proctoscopic examination on a manikin before you transfer to a patient. Medical students should learn the technique at the Phase 3 Introductory Course. 2. When you perform ano-rectal examination, your clinical supervisor must be present throughout. 3. Introduce yourself to the patient; explain your student status, course and year of study. 4. Explain the examination to the patient and obtain verbal permission. Discuss the need for a chaperone with the patient and your supervisor. If your supervisor is of different sex from the patient, arrange for a chaperone of the same sex as the patient. 5. Allow patient privacy for undressing. Explain the position for the examination. You should start with an abdominal examination to detect pathology and put the patient at ease. It is usual to examine the rectum with the patient lying on the left side (lateral position) with knees flexed and drawn towards the chest. 6. Before you start, check the examination tray for surgical gloves, lubricant jelly, tissues for wiping body areas after the examination, and a proctoscope if needed. 7. Wear surgical gloves on both hands. 8. Proceed with the rectal examination as instructed by your supervisor, treating your patient gently, and observing clinical etiquette throughout. Inform your patient when you have finished, explain your findings, and thank your patient. Ask your supervisor for feedback. 9. Record, date and sign the examination in the patient’s notes, stating that patient permission was obtained, and giving the name of your supervisor, and name and status of the chaperone. 22 9 - Code of Practice for Examination of Patients by Students Protocol for examination of female breasts 1. Learn and practise breast examination first on a mannequin or a volunteer patient in a group teaching session before transferring to a patient. When you first perform breast examination, your clinical supervisor must be present throughout. 2. Introduce yourself to the patient; explain your student status, your course, and year of study. Explain the examination to the patient and obtain verbal permission. If your supervisor is male, arrange for a female chaperone. 3. Allow patient privacy for undressing. Explain the position for the examination starting with the patient in a supine position with the head end of the couch elevated to 45 degrees, and then rolling to the side. 4. Proceed with the breast examination as instructed, observing carefully and palpating gently. Inform your patient when you have finished, allow her to cover herself, explain your findings, and thank your patient. Ask your supervisor for feedback. 5. Record, date and sign the examination in the patient’s notes, stating that consent was given, and giving the name of your supervisor and name and status of your chaperone. Protocol for examination of male external genitalia 1. For your first examination of male external genitalia, your clinical supervisor must be present. You should examine male external genitalia with great sensitivity and with no more than two students present one of who should be male if possible. 2. Introduce yourself to the patient; explain your student status, your course, and year of study. Explain the examination to the patient and obtain verbal permission. If you are examining alone, you must arrange for a chaperone who should be of the same sex as the patient. This could be a fellow student. Your hands should be warm. Do not rub them together in front of the patient! 3. Observe clinical etiquette throughout the examination. Start with the patient standing fully exposing his groins, and your eyes level with the area being examined. Observe the area and ask the patient to cough. Palpate the scrotum to determine the presence of two normal testes and any abnormal mass, and then palpate the inguinal and femoral areas for cough impulses. If you notice a swelling of the groin in the upright position, do not try to reduce it. 4. For the second part of the examination, ask the patient to lie down. The student should gently reduce any swelling. You should examine for hernia, palpate the femoral vessels, and scrotum. Inform your patient when you have finished, explain your findings, and thank the patient. 5. Record, date and sign the examination in the patient’s notes, stating that permission was obtained, and giving the name of your supervisor, and name and status of your chaperone. 23 10 – Fitness to Practise Medical students are entering a profession where appropriate standards of professional behaviour are expected by the public and this is regulated by the General Medical Council. King's College London has a Fitness to Practise Committee which deals with misconduct (under the terms of the College's Misconduct regulations) and matters of behaviour and health that raise issues of fitness for registration and practice. The School of Medicine also has an internal Fitness to Practise Advisory Committee that advises the Head of School on these matters. Students must inform the School through the Academic Centre of any issues of personal health or behaviour (e.g. blood borne virus infection, mental health issues, police cautions, convictions, proceedings, infringement of social media) which might affect their fitness to practise status. The GMC documents "Good Medical Practice" (http://www.gmc-uk.org/guidance/good_medical_practice.asp) and “Medical students: professional values and fitness to practise” (http://www.gmcuk.org/education/undergraduate/professional_behaviour.asp) are essential reading for undergraduate medical students. Medical students also have a duty to report issues that relate to the fitness to practise of other students or staff of the College or associated NHS trusts. This can be done in confidence to a senior member of the College such as a year head, personal or senior tutor, clinical or senior clinical advisor. Taking this action is an important duty for the safety of patients, staff and students" The KCL information ‘Regulations concerning students’ can be found at http://www.kcl.ac.uk/aboutkings/governance/regulations/students.aspx KCL information on ‘Fitness for Registration and Practise Regulations’ (B5) is to be found at http://www.kcl.ac.uk/college/policyzone/index.php?id=425 High standards of behaviour are expected at all times. You should be courteous to all staff including teaching, Academic Centre and clerical staff as well as other health professionals. Rudeness to staff, whether verbally or in writing is unprofessional and may lead to disciplinary action. 24 11 - Simulated and Interactive Learning (SaIL) The Chantler Clinical Skills Centre offers newly refurbished Simulated Learning Facilities for practical and clinical communication skills teaching for over 4,000 Medical, Nursing and Midwifery students. The centre includes a mock GP room, home environment, ward areas and clinical skills classrooms. Throughout the year additional Kings College clinical skills revision sessions are put on at the centre which can be found on our website: http://www.kcl.ac.uk/health/study/facilities/clinicalskills/index.aspx The Independent Learning Room (ILR) based within The Chantler Clinical Skills Centre: room 1.9 on the first floor of the Centre. The Independent Learning room is an unsupervised resource set up for both medical and nursing students to practise skills. To use the room you are required to sign in at the reception desk so we know who is using the resource. During busy periods the ILR is operated on a sign up basis with two hourly slots for you to sign up to via our website. The room is set up with equipment including blood pressure monitors, venepuncture arms, catheterisation models etc. If additional equipment is required please ask at the reception desk, if available you will be asked to sign for the equipment for use in the ILR only. Rules for use of The Chantler Clinical Skills Centre. For us to be able to operate a resource that works as an unsupervised facility you asked to behave professionally, read and adhere to the ILR rules. Please use the following link for more information on how to access the facilities and the rules for use:http://www.kcl.ac.uk/health/study/facilities/clinicalskills/teaching/ilroom.aspx SaIL at St Thomas’ House, hosts a mock GP consulting room, a six-bedded ward, an operating theatre/2bedded ICU ward, a home environment and a surgical simulation room. For more information please go to their website below: http://www.guysandstthomas.nhs.uk/healthprof/education/simulation_centre/simulation.aspx Clinical skills facilities are also available at other sites and at the teaching campus hospitals. Please see your site administrator for more information. 25 11 - Simulated and Interactive Learning (SaIL) Whilst these skills are not compulsory during Phase 3, you are advised strongly to take the opportunity to practise these at this stage. If your practice is observed by a member of staff you may obtain an additional sign-up that you should show to your Firm Head. This may be taken as evidence of your motivation and commitment to learn when your in-course assessment marks are being considered. Skill Date Practice observed by Suture a skin wound Insert an intravenous cannula Set up drip/infusion Give I-V injection Write up fluid chart Give intramuscular injection Insert a nasogastric tube Administer oxygen therapy 26 12 - In-Course Assessment of Clinical Skills: Guidance for Students You will have learned to perform a basic general clinical interview and examination during the Introductory Course for Phase 3. The core clinical skills listed here develop and extend the general clinical interview and examination for use in specific clinical contexts. You are required to be competent in the core skills listed under each rotation. In addition, resuscitation (basic life support/CPR) is a basic emergency skill introduced in Phases 1 and 2 and students are expected to remain competent throughout the course. Each skill has minimum performance criteria, similar to those used in the in-course and end-of-year OSCE assessments. These are included in the Logbook for each rotation and are also available on the Phase 3 web page of the Virtual Campus. You should practise each skill until you feel competent. Some skills are suitable for assessment on manikins or models and may be assessed in the Clinical Skills Centre. At this stage ask your firm head or tutor to observe and assess your performance and to sign this Logbook. Do not be distressed if your performance is unsatisfactory: seek feedback from your assessor (see p. 10). Practise the skill using the tutor’s feedback before requesting a repeat assessment later in the rotation. It is your responsibility to arrange for assessments. At the end of each rotation, ask your firm head to sign the section on professional development. This is a two way process in which student and supervisor discuss whether attendance, punctuality and courtesy to staff and patients have been satisfactory and if not how this can be remedied. You must be signed up for each of the Phase 3 skills in order to complete Phase 3 MBBS successfully. At the end of each rotation you must hand in your Logbook to the Academic Centre. It will be inspected for satisfactory completion of skills. Your Firm Head may inspect your Logbook at any time. In addition, random audits of Logbooks take place throughout the year. Usually a Campus administrator approaches a firm and photocopies a sample of Logbooks. These are checked – including signatures of staff who have signed up skills. It is a serious offence to forge a signature (see your Phase 3 Handbook for further details). You should meet your clinical adviser at least three times during Phase 3. Please ensure that he or she signs section 4. In case you lose your Logbook, photocopy and file the relevant signed pages at the end of each block and keep in a safe place. 27 12 - In-Course Assessment of Clinical Skills: Guidance for Students Phase 3 In-Course Marking Scheme & Expanded Performance Descriptors For use by Firm Head / GP Assessor for formative feedback to students Grade Exceptional Outstanding performance A minority of students only Good Student is above the requirements Pass Student has met requirements A broad range encompassing the majority of students Borderline History Taking (including communication skills) Excellent history taking with some aspects demonstrated to a very high level of expertise and no flaws at all Descriptors Clinical Examination Clinical knowledge (including mental state exam) (including clinical reasoning) Thorough, accurate and Comprehensive and detailed comprehensive clinical knowledge in most topics with no examination demonstrating gaps excellent skills throughout Professional development (including contribution to the Firm) Highest standards of conduct at all times; highly organized; excellent attendance and enthusiastic member of firm Consistently good history taking with some aspects demonstrated to a high level of expertise and few flaws Thorough, accurate and detailed clinical examination demonstrating good skills throughout with minimal errors Detailed and accurate knowledge in most topics with no significant gaps High standards of conduct and organization at all times; enthusiastic participation in all firm activities Well structured, methodical and sensitive history taking; no significant errors or omissions Comprehensive and proficient examination with no significant errors or omissions Good knowledge of most topics with depth in some areas, and no significant gaps High standards of conduct and organization most of the time; full attendance and participation Adequately structured, methodical, sensitive; no important omissions Able to perform examination covering all the essential aspects of case Satisfactory knowledge with few gaps Maintains appropriate standards of conduct, attendance and organization at all times Barely adequate in structure, but without major errors or omissions. May improve with effort Barely adequate examination, with some errors or omissions. May improve with effort Barely adequate level of knowledge, with several errors or gaps. May improve with effort Occasional lapses in conduct or organization that must be improved. Must improve with effort Poor and badly structured history Inadequate examination, with Inadequate knowledge, with Clearly below the required Fail with significant omissions poor technique and significant several significant errors or standards of professional conduct Student has not met suggesting lack of practice errors or omissions omissions and behaviour requirements A minority of students only: Very poor and incomplete. Rudimentary examination with Rudimentary knowledge with Displays serious lack of the student should be Unlikely to be capable of passing serious errors or omissions. many serious errors or omissions. professional standards (e.g. rude, informed how he or she Unlikely to be capable of Unlikely to be capable of passing disorganized). Unlikely to be this rotation might improve with effort passing this rotation this rotation capable of passing this rotation Non-attendance Insufficient evidence Insufficient evidence Insufficient evidence Seriously inadequate attendance and participation Excessive absence not permitting award of a grade In an average firm of 8 students, a firm head should rarely award an “Exceptional” grade. The majority of students should be expected to achieve a “Pass” grade. Only a small minority of students are likely deserve a “Fail” grade. These, and any whose attendance does not permit a grade to be awarded, should be reported directly to the Academic Centre and Head of Phase 3. 28 12 - In-Course Assessment of Clinical Skills: Guidance for Students Name of student: Rotation Student Grand Rounds Sign-up criteria • Students must attend and contribute actively to ALL student grand rounds during the Rotation. • Students should present at least two cases at student grand rounds in each rotation. • The tutor in charge of the student grand rounds will award a grade based on these two presentations (or on the best two if more than two cases are presented). • Tutors may take into account the complexity of the case presented. • Tutors will take account of the student’s overall attendance and participation in all student grand rounds in the Rotation. • It is the student’s responsibility to ensure that the tutor is fully aware of their attendance and participation in grand rounds. Students should consider the following criteria carefully when preparing a grand round presentation Tutors may refer to these criteria in awarding grades 1 Presentation skills including clarity, conciseness, and use of visual aids or handouts 2 Description of clinical and pathological features 3 Use of relevant tests and investigations 4 Assessment of principal clinical problems and differential diagnosis 5 Development of management plan 6 Evaluation of associated problems (e.g. ethical or public health issues) 7 Use of clinical sciences and literature review to illustrate case 8 Handling of questions and discussion 9 Reflective elements of this case for the student In each rotation, students will be awarded one of the following grades by the firm head or grand round tutor Grade Outstanding presentations, demonstrating personal knowledge and Exceptional involvement with clinical case and clear understanding of the clinical and non-clinical issues. Consistently useful contributions to grand round Outstanding performance discussions. At least 2 presentations of good quality. Personal assessment and knowledge of the cases. Understanding of the Good clinical and non-clinical issues Frequent useful contributions to discussion. Pass At least 1 presentation of good quality and one other of adequate quality. Adequate assessment and knowledge of the cases. Regular useful Student has met contributions to discussion. requirements Borderline At least 2 presentations of adequate quality. Acceptable assessment and knowledge of the cases. Occasional contributions to discussion. Fail Student has not met requirements Non-attendance Excessive absence not permitting award of a grade Very poor presentations, without evidence of personal effort in clerking patients and researching background. Inadequate presence at the grand rounds to be awarded a grade. The Tutor should enter the grade awarded on the student’s mark sheet 29 12 - In-Course Assessment of Clinical Skills: Guidance for Students Name of student: Rotation A: Academic Clinical and Professional Development Based on attendance, performance and participation in firm activities, courtesy to staff and patients, punctuality, acceptance of advice and feedback, confidentiality Mid-rotation Review of Progress: Satisfactory Unsatisfactory (if so, why) Comment on strengths and areas for improvement (For formative assessment see Expanded Performance Descriptors) * I have no concerns about this student's fitness to practise * I have the following concerns about this student's fitness to practise and I have referred this student to Head of Phase 3 or Senior Clinical Adviser The matrix on p.28 may be used by the Firm Head to give mid-rotation formative feedback and encourage improvement. Firm Head Name …………………………………..…… GMC no ……………. Signature ……..…………………………………………. Date ………………… 30 12 - In-Course Assessment of Clinical Skills: Guidance for Students Name of student: King’s College London School of Medicine Phase Three in Course Assessment Mark sheet 2012/13 Name:_______________________________ Student Number:__________ Firm: _______________________________ Rotation: A Term: 1 / 2 / 3 (please circle as appropriate) Grand Rounds FINAL GRADE AWARDED (please sign in ONE BOX ONLY as appropriate): Grade Exceptional Good Pass Borderline Fail Non-attendance Signature Where any grade other then “Pass” is awarded, the reasons should be documented in the section for Additional Comments. Note that in an average firm of 8 students, a firm head should rarely award an “Exceptional” grade. Name (Print): GMC no./Designation: Date: Feedback: 31 12 - In-Course Assessment of Clinical Skills: Guidance for Students Firm Head End-of-rotation FINAL GRADE AWARDED (please sign in ONE BOX ONLY as appropriate): Grade Exceptional Good Pass Borderline Fail Non-attendance Signature Where any grade other then “Pass” is awarded, the reasons should be documented in the section for Additional Comments. Note that in an average firm of 8 students, a firm head should rarely award an “Exceptional” grade. Name (Print): GMC no./Designation: Date: Feedback: * I have no concerns about this student's fitness to practise * I have the following concerns about this student's fitness to practise and I have referred this student to Head of Phase 3 or Senior Clinical Adviser 32 13 – Sign-Ups ROTATION A: Basic adult medicine and surgery including gastroenterology, urology, nephrology, endocrinology and related topics Skills must be signed by an experienced clinician who has been approved by the firm head PREPARATION Name of Student: Cleanse hands in the clinical environment See Logbook section 5: Infection control in clinical practice Importance of hand cleansing in control of cross infection in the ward and clinic Hand cleansing or washing to be performed before and after each physical examination of procedure Use of water, soap, nail brush Use of alcohol gel cleansing agent Correct technique: palms and dorsal surfaces; each finger individually; finger tips and nails Correct duration of washing/cleansing Hand drying if washed in water Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 33 13 – Sign-Ups Name of student: Set up a sterile field Cleanse hands Collect a dressing trolley and clean with a antiseptic wipe, over all flat edges and legs Collect all equipment needed and place on the bottom of the trolley Clean hands with alcohol gel Put on a disposable plastic apron Open the outer cover of the sterile dressing pack and slide the contents onto the top shelf of the trolley. Open the sterile field using an aseptic non-touch technique Open all of the equipment into the field using a aseptic non touch technique Open cleaning solution using aseptic non touch technique and pour into receiver Clean hands with alcohol gel Put on sterile gloves Maintain asepsis throughout procedure I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 34 13 – Sign-Ups Name of student: Sterile glove technique Perform hand hygiene before an “aseptic procedure” by handrubbing or hand washing Check the package for integrity. Open the first non-sterile packaging by peeling it completely off the heat seal to expose the second sterile wrapper, but without touching it Place the second sterile package on a clean, dry surface without touching the surface. Open the package and fold it towards the bottom so as to unfold the paper and keep it open Using the thumb and index finger of one hand, carefully grasp the folded cuff edge of the glove Slip the other hand into the glove in a single movement, keeping the folded cuff at the wriest level Pick up the second glove by sliding the fingers of the gloved hand underneath the cuff of the glove In a single movement, slip the second glove on to the ungloved hand while avoiding any contact/resting of the gloved hand on surfaces other than the glove to be donned (contact/resting constitutes a lack of asepsis and requires a chance of glove) If necessary, after donning both gloves, adjust the fingers and interdigital spaces until the gloves fit comfortably Unfold the cuff of the first gloved hand by gently slipping the fingers of the other hand inside the fold, making sureto avoid any contact with a surface other than the outer surface of the glove (lack of asepsis requiring a change of gloves) The hands are gloved and must touch exclusively sterile devices or the previously disinfected patient’s body area Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 35 13 – Sign-Ups Name of student: Sterile scrub technique and gowning Removes jewellery, except wedding ring Dons a theatre cap and mask in theatre Lays out gown and gloves in aseptic manner Opens scrub brush before wetting hands Turns on taps ensuring optimal water temperature Scrubs with appropriate skin disinfectant Scrubs from fingertips and washes to elbows, concentrating on glove area Uses scrubbing brush appropriately Rinses from fingertips to elbows keeping fingers higher than elbows Uses elbows to turn off taps Dries hands Picks up gown and inserts arms, ensuring outside is not touched Stands still while assistant fastens gown Puts on gloves in sterile manner Keeps hands above waist Maintains sterility throughout Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 36 13 – Sign-Ups ASSESSMENT Name of student: Interview a patient to elicit a full clinical history (including the history of the presenting complaint) Cleanses hands Introduces him/herself to patient Identifies patient positively (name, date of birth and wrist-band for inpatient; name and date of birth for outpatient) Puts patient at ease and establishes rapport Asks patient to describe presenting complaint in his/her own words Ensures all presenting symptoms are elicited Explores and clarifies vague symptoms For each presenting symptom, asks about: • mode of onset • severity, location and other characteristics • duration and evolution over time • provoking, exacerbating and relieving factors Asks about associated symptoms in any system (including psychiatric) Asks about impact of symptoms on patient’s life Uses direct questioning to elicit symptoms in other systems (review of systems) Asks about previous medical (including psychiatric) history and treatment Asks about medication and allergies Asks about smoking, alcohol and illicit drugs Asks about family medical history Asks about social circumstances Asks about personal history (including developmental, academic, occupational, psychosexual, forensic) Obtains collateral history when appropriate (e.g. carer, friend, neighbour) Uses appropriate language Appropriate use of questions; open, closed and clarifying Encourages patient’s questions and deals with them appropriately Acknowledges patient concerns Appropriate summary and analysis of history. Use the information obtained from the history to formulate a differential diagnosis Record details of the history in the patient’s clinical record Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 37 13 – Sign-Ups Name of student: Interview a patient who complains of abdominal pain Cleanses hands Introduces him/herself to the patient Identifies patient positively (name, date of birth and wrist-band for inpatient; name and date of birth for outpatient) Establishes rapport with patient Asks about location of pain Asks about the onset and duration of pain Asks about nature of pain Asks about radiation Asks about provoking and relieving factors Asks about associated symptoms i.e. N&V, urinary symptoms, diarrhoea/constipation, rectal bleeding etc Asks about other common symptoms (review of systems) Asks about past medical history including previous pain Asks about family history Asks about medications and allergies Asks about smoking and alcohol Asks about social history Uses appropriate language Appropriate use of questions; open, closed and clarifying Encourages questions from patient and deals with them appropriately Acknowledges patient’s concerns Appropriate summary and analysis of history. Use the information obtained from the history to formulate a differential diagnosis Record details of the history in the patient’s clinical record Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 38 13 – Sign-Ups Name of student: Interview a patient with a urological complaint Cleanses hands Introduces him/herself to patient Identifies patient positively (name, date of birth and wrist-band for inpatient; name and date of birth for outpatient) Establishes rapport with patient Enquires about main complaint Asks about pain including duration, periodicity, radiation and provoking factors Asks about prostatic symptoms Asks about haematuria Asks about dysuria Asks about urethral discharge and sexual contacts Asks about other common symptoms (review of systems) Asks about previous medical history Asks about medication and allergies Asks about family history Asks about social history and diet Uses appropriate language Appropriate use of questions, open, closed and clarifying Encourages questions from patient and deals with them appropriately Acknowledges patient’s concerns Appropriate summary and analysis of history. Use the information obtained from the history to formulate a differential diagnosis Record details of the history in the patient’s clinical record Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 39 13 – Sign-Ups Name of student: Examine the abdomen Introduces him/herself to the patient Identifies patient positively (name, date of birth and wrist-band for inpatient; name and date of birth for outpatient) Establishes rapport with patient Explains examination and gains permission to examine Ensures adequate privacy for the examination Cleanse hands with alcohol gel Positions the patient appropriately and exposes maintaining dignity Examines the hands Examines the eyes and mouth Examines the neck for nodes Inspects the abdomen Asks to cough looking for hernias Asks if anywhere hurts Palpates generally Palpates each quadrant systematically Examines liver, spleen and kidneys appropriately Feels for aortic swelling Examines inguinoscrotal areas (see below) Checks femoral pulse appropriate Suggests rectal examination Encourages questions from patient and deals with them appropriately Acknowledges patient’s concerns Assists replacing patient’s clothing/bedclothes Appropriate summary and analysis of findings. Use the information obtained from the examination to formulate a differential diagnosis Record details of the examination in the patient’s clinical record Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 40 13 – Sign-Ups Name of student: Examine the inguinal region including hernial orifices and lymph nodes Introduces him/herself to patient Identifies patient positively (name, date of birth and wrist-band for inpatient; name and date of birth for outpatient) Establishes rapport with patient Explains examination and ensures consent Cleanse hands with alcohol gel Positions patient appropriately and exposes, maintaining dignity of patient Warms hands Gets patient to cough and looks for hernias Examines femoral triangle Examines inguinal canal Feels for cough impulse in femoral and inguinal hernias Examines femoral pulses Restores patient clothing Encourages questions from patient and deals with them appropriately Acknowledges patient’s concerns Assists replacing patient’s clothing/bedclothes Appropriate summary and analysis of findings. Use the information obtained from the examination to formulate a differential diagnosis Cleanse hands with alcohol gel Record details of the examination in the patient’s clinical record Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 41 13 – Sign-Ups Name of student: Examine the male external genitalia (may be practised on a model) Introduces him/herself to patient Identifies patient positively (name, date of birth and wrist-band for inpatient; name and date of birth for outpatient) Establishes rapport with patient Asks permission to examine and explains examination (normally follows examination of the abdomen) Cleanses hands with alcohol gel. Warm hands. Inspects patient standing (or lying on the couch): note gynaecomastia and distribution of body hair Inspects groin and genitalia with patient lying on the couch Examines skin of penis. Retracts foreskin and examines glans and external urethral meatus (express discharge) Examines scrotum: note both testes; and presence of lumps Palpate each testis, epididymis and vas deferens; and any lumps Tests for translucency of any lump Test for cough impulse Suggests standing to assess for varicocoele or saphenofemoral varix Palpates inguinal lymph nodes in the inguinal crease Respects patient’s dignity throughout Encourages questions from patient and deals with them appropriately Acknowledges patient’s concerns Cleanses hands with alcohol gel Appropriate summary and analysis of findings. Use the information obtained from the examination to formulate a differential diagnosis Record details of the examination in the patient’s clinical record Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 42 13 – Sign-Ups Name of student: Perform a rectal examination (should be practised on a model) Introduces him/herself to patient Identifies patient positively (name, date of birth and wrist-band for inpatient; name and date of birth for outpatient) Explains examination and ensures consent (normally follows examination of the abdomen) Cleanses hands with alcohol gel. Warm hands; wears gloves Positions patient appropriately: left lateral position at edge of couch, knees drawn up to chest Separates buttocks, inspects anus and skin Asks patient to strain and inspects mucosa Inserts lubricated finger gently into anus and rectum. Assesses anal tone Rotates finger to palpate internal surface of anal canal and rectum Palpates prostate in male (or cervix in female) patient Notes consistency of faeces Withdraws finger and inspect for faeces, blood and mucus Wipes anal area clean of lubricant and faeces Disposes of gloves and soiled material Respects patient’s dignity throughout Encourages questions from patient and deals with them appropriately Acknowledges patient’s concerns Cleanses hands with alcohol gel Appropriate summary and analysis of findings. Use the information obtained from the examination to formulate a differential diagnosis Record details of the examination in the patient’s clinical record Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 43 13 – Sign-Ups Name of student: Examine the neck Introduces him/herself to patient Identifies patient positively (name, date of birth and wrist-band for inpatient; name and date of birth for outpatient) Establishes rapport with patient Asks about relevant symptoms Asks permission to examine and explains examination Cleanse hands with alcohol gel Ensures appropriate position to examine patient Exposes neck adequately and observes lump Asks about pain and tenderness Asks about changes in size of lump Palpates lump and tests if lump moves on swallowing or protruding tongue Examines lymph nodes Assesses tracheal position Auscultates over lump Restores patient clothing Encourages questions from patient and deals with them appropriately Acknowledges patient’s concerns Appropriate summary and analysis of findings. Use the information obtained from the examination to formulate a differential diagnosis Cleanse hands with alcohol gel Record details of the examination in the patient’s clinical record Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 44 13 – Sign-Ups INVESTIGATION Name of Student: Perform a BM glucose test Introduces him/herself to patient Identifies patient positively (name, date of birth and wrist-band for inpatient; name and date of birth for outpatient) Establishes rapport with patient Explains procedure and ensures consent Ensures patient is sitting or lying down Assembles equipment Inserts strip and calibrates machine appropriately Chooses an appropriate place for test and ensures warm and well perfused Cleanse hands with alcohol gel and puts on gloves Takes autolet and inserts sharply into skin drawing blood Obtains a hanging drop of blood without undue squeezing of puncture site Drops blood onto test strip Waits until machine records a reading Disposes of sharp safely Checks haemostasis Disposes of strip and gloves Reads correctly and records Acknowledges patient concerns and deals with questions from patient Appropriate interpretation of value. Use the information obtained from the test results to formulate a differential diagnosis Lists factors which might contribute to an inaccurate recording Record details of the procedure in the patient’s clinical record Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 45 13 – Sign-Ups Name of Student: Test urine and interpret results Identifies patient positively (name, date of birth and wrist-band for inpatient; name and date of birth for outpatient) Givens patient correct instructions to pass mid-stream urine sample Puts gloves on Checks container for correct stick and expiry date Opens container and takes out single stick, closes bottle Decants urine over lab stick into bowl Taps off excess urine Holds strip horizontal until test is complete Reads stick after appropriate time Records result Disposes of stick and gloves Cleanse hands with alcohol gel Interprets results appropriately. Use the information obtained from the test results to formulate a differential diagnosis Acknowledges need to send urine to laboratory for an MSU Record details of the procedure in the patient’s clinical record Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 46 13 – Sign-Ups Name of Student: Nutrition (BMI) Introduce him/herself to the patient and identifies the patient positively (name, date of birth and wristband for in patient: name and date of birth for outpatient) Familiarise him/herself with nutritional assessment tools utilised by the NHS Cleanse hands with alcohol gel Obtains a nutritional history of the patient’s daily dietary intake. Asks about unintentional weight loss or weight gain in the past 3-6 months Explore any indicators for clinical concern of nutritional status Discuss the procedure for assessing a BMI Position patient correctly in the stadiometer (stand erect, footwear removed, facing away from wall, heels to wall, head such that external auditory meatus is on same horizontal as lateral canthus) Move reading arm of stadiometer to touch patients head firmly Read and record height correctly For weighing, check patient in indoor clothing and footwear removed Check balance (steelyard type not bathroom scales)correctly zeroed With patient on platform, adjust weight to achieve balance Read and record weight calculate BMI score Explains the results of the BMI to the patient and provide advice on nutritional intake, exercise and support as appropriate Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 47 13 – Sign-Ups Name of Student: Examine a plain abdominal x-ray in the adult Use of plain abdominal X-ray as extension of the examination of abdomen Identify patient: name, date of birth, hospital number, date of X-ray Position of patient: straight or rotated? Bony skeleton: identify and check integrity of components of skeleton in abdomen and pelvis Identification of major structures and organs Presence of air or fluid levels in the hollow viscera Presence of air under the diaphragm Presence of calcification of soft tissues, e.g. aorta. Record details of the examination in the patient’s clinical record. Use the information obtained to formulate a differential diagnosis Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 48 13 – Sign-Ups Name of Student: Interpretation of clinical chemistry test results Choosing clinical chemistry tests and investigations in adult patient Identify patient: name, date of birth, hospital number, date of tests Making use of reference ranges to interpret test results Interpretation of routine tests e.g. urea and electrolytes; cardiac enzymes; liver function tests. Interpretation of endocrinological tests e.g. thyroid function tests; glucose and HbA1c Interpretation of metabolic tests (e.g. cholesterol and triglycerides; calcium, phosphate, alkaline phosphatase) Interpretation of immunological tests: immunoglobulins; etc Record details of the test results in the patient’s clinical record. Use the information obtained to formulate a differential diagnosis Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 49 13 – Sign-Ups TREATMENT Name of Student: Checking patients’ prescription charts Identifies patient positively (name, date of birth, hospital number) Allergies stated (allergies to be written in red ink) Correct drug name Correct dosage Correct route e.g. oral/i-v/i-m/rectal Drugs written in correct area of drug chart Correct frequency and timing of dosage Duration of treatment stated if required Name and signature of prescriber Date of signing Aware of different prescription charts used in different settings e.g. Inpatient, inpatient TTO, outpatient (HP10), GP/community (FP10). Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 50 13 – Sign-Ups Name of Student: Complete a replica inpatient prescription chart (downloaded from the Virtual Campus) (only to be completed after “checking patients’ prescription charts” skill signed off) Phase 3 students are not expected to be familiar with prescribing for children nor prescribing a controlled drug Read “How to write a prescription chart” on the VC (download a sample chart for practice) http://virtualcampus.kcl.ac.uk/vc/medicine/coursebooks/coursebooks.aspx?course=year3 Be familiar with the British National Formulary (BNF) Write all entries legibly Sign all entries correctly (full signature, not initials, and print name) Identify patient positively (name, date of birth, hospital number, address). Use a patient sticker if available State location of patient (ward, unit, etc) Write consultant details including hospital code as appropriate Identify self fully (name, medical student) Date new chart started (dd/mm/yyyy) Allergies: identify and list all allergies and drug reactions (allergies to be written in red ink). Sign and date entry. Amend if new reaction occurs Prescribe each medication according to BNF guidance: Print drug name Correct dosage (patient’s age, pregnancy, hepatic and renal function) Correct route (oral/i-v/i-m/s-c/rectal/inh) Correct frequency and timing of doses Duration of treatment (esp. for antibiotics) Sign (and print name) and date (dd/mm/yyyy) Complete once only (“stat”) medication section Complete regular medication section Complete as required (“PRN”) medication section Complete oxygen administration section Check all entries written in correct area of prescription chart Aware of different prescription charts used in different settings e.g. Inpatient, inpatient TTO, outpatient (HP10), GP/community (FP10) Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 51 13 – Sign-Ups Name of Student: Administer a subcutaneous injection e.g. Insulin Introduces him/herself to patient Identifies patient positively (name, date of birth and wrist-band for inpatient; name and date of birth for outpatient) Establishes rapport with patient Explains procedure and ensures consent Checks patient details against prescription chart Checks for allergies on prescription chart & with patient Checks drug prescription on chart Cleanse hands with alcohol gel Puts on fresh gloves Checks ampoule contains correct drug & correct concentration Checks drug expiry date Assembles appropriate equipment Checks any specialist syringe used matches concentration of drug (if appropriate) Decontaminates surface of multi-dose vial with alcohol (if appropriate) Draws up correct dose Cross-checks drug dose with staff Changes needle to subcutaneous needle (if appropriate) Selects appropriate site for injection Decontaminates site with alcohol Inserts needle subcutaneously & injects at appropriate speed Safely disposes of sharps Records drug administration on prescription chart Acknowledges patient concerns and deals appropriately with questions/concerns Record details of the procedure in the patient’s clinical record Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 52 13 – Sign-Ups Name of Student: Insert a urinary catheter into a male patient (breakdown of the skill) Confirms patients identity, explains the procedure and obtains verbal consent (remember to check for any allergies i.e. latex, local anaesthetic) Collect equipment and place on the bottom of a clean trolley Catheter pack Appropriate size catheter Syringe for balloon inflation Water for injection for balloon inflation Cleaning solution Local anaesthetic gel (11mls) Clinical waste bag Sterile Gloves x2 Catheter bag Wash Hands and put on a disposable apron Open catheter pack using sterile technique. Carefully open onto the sterile field the supplementary equipment Open the syringe from package and remove carefully, only touching the handle-end of the syringe. Twist the cap off the water for injections and draw up volume according to manufactures instructions. lay syringe on the side of sterile field with the handle-end positioned off the sterile field as this part is now un-sterile Correct positioning of patient and expose the patient, maintaining privacy and dignity Cleanse hands with alcohol gel and apply gloves (or double gloves) Lay sterile drape over the patient so genitalia are exposed Holding the penis upright with a gauze swab cleanse penis from urethral meatus down the shaft. Only cleaning in one direction. Retract foreskin if present when cleaning Insert all the local anaesthetic gel into the meatus. Wait 3-5 minutes Remove outer pair of gloves carefully or change gloves, decontaminating hands Position kidney dish/tray between the patients thighs to catch any spillages Remove tip of plastic wrapper around the catheter. Hold the penis upright with a sterile gauze swab, insert catheter tip into the urethral meatus, advance slowly feeding the catheter out of the remaining paper Negotiate the prostatic bend. On entering the bladder urine should start to drain. Advance the catheter fully to ensure the balloon is in the bladder Inflate balloon with correct volume of water for injection via the catheter port. If patient experiences any pain then stop Once the balloon is inflated gently withdraw catheter until resistance is felt. Do Not Pull on the catheter Attach sterile drainage system (catheter bag) Reposition foreskin to prevent paraphimosis Clean and redress patient as necessary. Address any concerns Clean up, removes gloves and apron and put all waste in clinical waste bin. Wash hands Record in the patients notes; Date and Time, reason for catheter, size and make of catheter, batch No, Balloon size, residual urinary volume and sign Feedback given I have observed this student display a level of competence appropriate to Phase 3 Signed: Name(Print) GMC no./Designation Date Feedback comments (recorded by clinician or student): 53 13 – Sign-Ups Name of Student: ROTATION A ON CALL SHIFTS You must spend at least one on call shift with a junior or other suitable doctor during this rotation. Participating in more than one shift may be taken as evidence of your motivation and commitment to learn when your in-course assessment marks are being considered. Practice observed by: Name(Print): GMC no./Designation Date Practice observed by: Name(Print): GMC no./Designation Date Practice observed by: Name(Print): GMC no./Designation Date 54 13 – Sign-Ups Name of Student: Rotation A Scenario - record of completion Students should attend all Scenario teaching sessions where provided. PLEASE ATTACH YOUR PRINTED CONFIRMATION OF COMPLETION BELOW _____________________________________________________________________________________ Rotation A Online Firm Feedback confirmation Shortly before the end of your clinical rotation you will receive an email asking you to complete an online feedback form for your firm. THE ONLINE FIRM FEEDBACK IS MANDATORY PLEASE ATTACH YOUR PRINTED CONFIRMATION OF COMPLETION BELOW _____________________________________________________________________________________ 55 13 – Sign-Ups Name of Student: Feedback Training Workshop – record of completion Students must attend a Feedback Training Workshop during Phase 3. PLEASE ATTACH YOUR SIGNED PRINTED CONFIRMATION OF COMPLETION BELOW _____________________________________________________________________________________ 56 14 – Additional Mandatory Experiences Name of Student: Basic Life Support Session At the start of Phase 3 you will be required to attend a Basic Life Support session either in the 2nd introductory week on your allocated site, or in the first few weeks of your rotation. This is compulsory. Record of attendance Please ensure you complete the below after your session Date and Venue Student Sign Print Pathology and Therapeutics Attendance at Post-Mortems You must attend at least one post-mortem examination at any time during the year. Please enter the details below: Date: Hospital: Rotation: Indication for PM: Hospital: Rotation: Indication for PM: Brief findings: Date: Brief findings: Shadow a Ward Pharmacist You should ask a Ward Pharmacist if you may shadow him/her for a ward round in order to view drug charts and discuss issues of prescription writing. This must be done at least once at any time during the year. Date: Hospital: Ward: Rotation: Name of Pharmacist: 57 14 – Additional Mandatory Experiences Name of Student: Visit a Pathology Laboratory Offer to take one or more urgent samples to the Pathology laboratories and note the laboratory procedures for in-hours and out-of-hours urgent & non-urgent sample collection and submission. It may be possible for you to visit the laboratories, please contact one of the local Pathologists. This must be done at least once at any time during the year. Date: Hospital: Laboratory Rotation: Type(s) of sample: Gordon Museum visit You are required to visit the Gordon Museum at least once during each rotation in Phase 3 to study the pathological specimens relevant to the rotation. Signed by Gordon Museum staff: Print name: Date: Rotation/s visited: 58 14 – Additional Mandatory Experiences Name of Student: Interprofessional Learning in Practice (ILP) As part of your clinical experience in Phase 3 you may be invited to participate in an interprofessional learning seminar. Health care students that are based in the Trust are invited to attend. The seminar will be patient focused and will involve either talking with a patient about their experiences or working with a patient in the clinical area. As far as possible the patients’ health care needs will be related to the rotation you are in. Students will discuss their differing responsibilities and perspectives of the patient and thereby learn more about each other’s roles and responsibilities. If you are included you will be notified and provided with preparatory information. You will be expected to join the other students in attending the session. Time spent will count towards your professional development and you will receive a certificate of attendance. You will be expected to reflect upon what you have learnt from the session and record your reflections on the certificate of attendance. The GMC places great importance on interprofessional learning. If you are requested to attend you should do so. Record of attendance Please ensure that the facilitator verifies your participation in this exercise Date and Venue Facilitator Sign Print Ethics Report For your second meeting with your clinical adviser towards the end of your first rotation, you are required to submit to your clinical adviser, in advance, a reflective account of some aspect of clinical practice which you found interesting. The reflective account should be typed, and about 800 words in length. You should briefly describe the clinical situation (keep the names of patients and staff anonymous). You should then reflect on the practice you encountered, identifying those aspects that you found interesting and why you found it so. You should draw upon the relevant literature, in particular the GMC's Good Medical Practice. Your reflective practice account will form part of the discussion with your clinical adviser. Clinical adviser will forward to the Head of Year and the Senior Adviser in Medical Ethics those accounts that they consider worthy of a prize. 59 14 – Additional Mandatory Experiences Name of Student: Patient Educator Sessions You must attend at least one patient educator session during the year. If you sign up online for a patient educator session you must attend that session. On completion of the session the student will have: Practised a complete physical examination of the system stated below using the appropriate guide/checklist Demonstrated patient-centred communication skills in an integrated fashion before, during and after the examination Received and responded appropriately to feedback and related this to personal learning needs. NB. Failure to attend a session you have signed up for may be regarded as unprofessional conduct and lead to reprimand by the head of Phase 3. System: Patient Educator: Name ……………………………………………….… Signature ……..………………………………………………………………Date ………………….. System: Patient Educator: Name ……………………………………………….… Signature ……..………………………………………………………………Date ………………….. System: Patient Educator: Name ……………………………………………….… Signature ……..………………………………………………………………Date ………………….. 60 15 – Patients Clerked Name of Student: At least 2 patients must be clerked and examined fully (i.e. all systems) and recorded in the Logbook each week Patient information should be anonymized Anonymized Patient Identifier Brief Clinical Summary Dates Seen Further involvement Reflection (tick box) □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ 61 15 – Patients Clerked Anonymized Patient Identifier Brief Clinical Summary Dates Seen Further involvement Reflection (tick box) □ □ □ □ □ □ □ □ □ □ □ □ □ □ □ Notes 62 16 – Phase 3 Core Patient Cases The core cases and procedures form the basis of adult clinical medicine encountered in Phase 3. You should try to clerk patients with each of these conditions or undergoing the named procedures in order to build up your clinical knowledge and skills. You should observe the management of the emergencies and the performance of clinical procedures – you will see some of these only on acute “take” or during your on-call shifts. Whenever you have clerked a patient with one of these conditions, or observed a procedure, you should read about it so that you understand it fully. You must also attend post-mortem examinations regularly throughout the year. In the Phase 3 student Handbook, you will see that many of these cases are linked to weekly topic teaching on the firms. It is your responsibility to ensure that you see and clerk these patients. By the end of Phase 3, you should be able to understand the basic science and pathology underlying these conditions, their diagnosis and their management. You should also understand their social and psychological impact on the patients, their implications for public health, and any ethical issues they raise for the patient, the doctor or society at large. Level of knowledge expected (see Miller’s hierarchy of clinical competence) 1. Knows of: you should have some knowledge of all the cases and their associated procedures listed here. In Phase 3 you should be able to state the main clinical features of each case, and know the indications for the procedures listed. 2. Knows about or how to: you should be able to describe the presentation or procedure, be able to use clinical information to build up a differential diagnosis, and be able to present this to a member of staff. In Phase 3 you should observe procedures so that you are able to describe them in detail (e.g. ECT or bronchoscopy) and others in outline only (e.g. echocardiography, psychosurgery). You should be able to explain diagnoses and their treatments (medical, surgical or psychological) to a patient. 3. Shows how to: you should be able to perform the procedure or manage the condition. In Phase 3 you should be able to perform those procedures (skills) listed in your Logbook and use them to diagnose and manage common conditions. Differential diagnosis You must apply clinical reasoning to clinical information from the patient’s history or examination, pathological information from tests and investigations, and collateral information from the patient’s carers or family in order to formulate a differential diagnosis Both positive and negative findings must be considered. The following schema may assist in organizing information to arrive at a differential diagnosis. Clinical, pathological or collateral information Differential diagnoses Supporting this diagnosis Neither supporting nor opposing this diagnosis Opposing this diagnosis Diagnosis 1 Probable/most likely Diagnosis 2 Possible/less likely Diagnosis 3 Improbable/least likely 63 16 – Phase 3 Core Patient Cases RESPIRATORY TOPICS Emergencies Acute respiratory failure Acute asthma Acute pulmonary oedema Pulmonary embolism Procedures / operations Aspiration of pleural effusion Blood gas estimation Bronchoscopy Chest drain CT Scan Respiratory function testing Smoking cessation advice Ultrasound Ventilation-perfusion tests Cases Acute exacerbation of COPD AIDS Asthma Atopy Bronchiectasis Bronchitis Carcinoma of the bronchus COPD Cough Cystic fibrosis Emphysema Fibrosing alveolitis Hay-fever Infection in the immuno-compromised patient Lung abscess Pleural effusion Pneumonia Pneumothorax Pulmonary secondaries Sleep disorders Tuberculosis Coronary arteriography Doppler ECG Echocardiography Exercise testing GTN spray Insertion of a CVP line MRI Scan Rehabilitation post-CABG or MI Resuscitation (basic life support/CPR) Thoracotomy Valve replacement Cases Aneurysms: aortic / popliteal / other Angina Arrhythmias Arterio-venous fistulae, congenital abnormalities & trauma Arteritis, Buerger’s disease Atheroma Blue, gangrenous or dead leg Cardiomyopathy Congestive cardiac failure Cor pulmonale Deep vein thrombosis Embolism Heart block Hypertension Left and right heart failure Painful, swollen or paralysed leg Pericardial disorders Post myocardial infarction Post-phlebitic limb Raynaud’s / vasospasm Thrombosis Varicose veins Venous ulcers CARDIAC AND VASCULAR TOPICS Emergencies Anaphylaxis Arrhythmias Cardiac arrest Cellulitis Endocarditis Haemorrhage Malignant (accelerated) hypertension Myocardial infarction Shock (cardiogenic / hypovolaemic) Unstable angina Procedures / operations Amputation Angiography CABG Cardioversion GENERAL MEDICAL AND MULTI-SYSTEM TOPICS Emergencies Alcohol related emergencies (intoxication, delirium tremens, hepatitis, rum fits) Drugs overdose Septicaemia Sickle cell crisis Procedures / operations Gastric lavage Haematological tests Incision and drainage of abscess Local anaesthesia Muscle relaxants Pain relief / analgesia Cases Alcohol related problems 64 16 – Phase 3 Core Patient Cases Anaemias (iron, B12, folate, chronic disease) Arthritides (including osteoarthritis) Carcinomas (prostate, breast etc.) Carcinomatosis Chest wall problems Clotting disorders Gout Leukaemias Lymphomas Rheumatoid and seronegative arthropathies Vasculitic and granulomatous disorders (SLE, giant cell arteritis, Wegener’s) Oesophageal stricture Peptic ulcer disease Reflux oesophagitis GENERAL SURGICAL TOPICS Emergencies Abdominal sepsis Abdominal trauma Acutely ill surgical patient Ruptured abdominal viscus Procedures / operations General anaesthesia Pre-operative preparation Post-operative management (pain / analgesia / fluid balance) Suturing Wound healing Cases Hernia - inguinal - femoral - incisional - umbilical Lumps, bumps and abscesses LOWER GASTROINTESTINAL TOPICS Emergencies Abdominal ultrasound Acute appendicitis Acute diverticulitis Acute inflammatory bowel disease Large bowel obstruction Peritonitis Rectal bleeding Procedures / operations Appendicectomy Barium enema Colectomy Colonoscopy Formation of a stoma Proctoscopy Sigmoidoscopy Cases Anal problems - haemorrhoids - abscess - fissure - fistula Carcinoma of the colon Constipation Diarrhoea Diverticular disease Inflammatory bowel disease Stomas UPPER GASTROINTESTINAL TOPICS Emergencies Acute gastritis Exacerbation of peptic ulcer GI Haemorrhage / haematemesis Small bowel obstruction Procedures / operation Abdominal ultrasound Barium meal Gastroscopy Emergency endoscopy Cases Achalasia Carcinoma of the oesophagus Carcinoma of the stomach Cirrhosis Dysphagia Hepatitis Hiatus hernia Malabsorption Nausea Oesophageal motility disorders HEPATO-PANCREATO-BILIARY TOPICS Emergencies Acute cholecystitis / biliary colic Acute pancreatitis Hepatic encephalopathy Procedures / operations CT scan ERCP HIDA scan Laparoscopic cholecystectomy MRI scan Ultrasound Cases Carcinoma of the pancreas Cholecystitis Chronic pancreatitis Cirrhosis Gallstones and complications Hepatitis Liver tumours Obstructive jaundice Portal hypertension 65 16 – Phase 3 Core Patient Cases RENAL / UROGENITAL TOPICS Emergencies Acute electrolyte disturbances Acute renal failure Acute retention of urine Torsion of testis Ureteric colic Urinary tract infection Procedures / operations Catheterisation (male and female) Cystoscopy Haemodialysis Hernia repair Intravenous urogram Isotope scanning Nephrectomy Peritoneal dialysis Prostate radiology (U/S) Renal transplantation Renal ultrasound TURP Urinalysis Urodynamics Cases Bladder tumours Carcinoma of the kidney Carcinoma of the prostate Chronic renal failure Chronic retention Epididymal cyst Haematuria Hydrocele Hydronephrosis Nephritis Nephrotic syndrome Polycystic disease of kidneys Prostatic hypertrophy Renal and ureteric stones ENDOCRINE / METABOLIC TOPICS Emergencies Acute hypoglycaemia Addisonian crisis Hyperglycaemic coma Procedures / operations Blood glucose estimation Glucose tolerance test Nuclear medicine and ultrasound Thyroidectomy Cases Cushing’s syndrome Diabetes mellitus (types 1 and 2, and complications) Hypercholesterolaemia Hyperparathyroidism Hyperthyroidism Hypothyroidism Lumps in the neck Metabolic bone disorders (Paget’s, osteomalacia, osteoporosis) Parathyroid disease Pituitary disorders Salivary gland disorders NEUROLOGICAL TOPICS Emergencies Cerebrovascular accidents (including cerebral infarction) Coma Head injury Meningitis, encephalitis & brain abscess Raised intracranial pressure Status epilepticus Subarachnoid haemorrhage Subdural haemorrhage Transient ischaemic attacks Procedures / operations EEG / evoked potentials EMG Evoked potentials MRI PET Cases Blackouts Brain tumours Epilepsies Headache, migraine, facial pain Infections of the nervous system Inflammatory diseases of the nervous system Limb sensorimotor dysfunction Movement disorders incl. gait and tremor Multiple sclerosis Neuropathies Parkinson’s Wilson’s PATHOLOGY TOPICS Procedures Description of pathological specimens (“pots”) Chemical pathology investigation Haematology investigation Histopathology investigation Microbiology investigation Post mortem examination Cases Pathological basis of core cases See separate Pathology course handbook PSYCHIATRIC TOPICS Emergencies Acute brain syndromes (delirium) 66 16 – Phase 3 Core Patient Cases Attempted suicide / suicidal intent Deliberate self harm Drug overdose Mania Serotonergic syndrome Neuroleptic malignant syndrome (malignant hyperthermia) Violent behaviour Procedures / operations Cognitive state examination (including simple screening tests such as Mini-mental state examination, Abbreviated mental test score) Depot injection ECT Mental capacity act Mental health act (“Sections”) Psychosurgery Cases Acute and transient psychoses Adjustment disorders Alcohol misuse / dependence Amnesic syndromes Anxiety (including generalized anxiety disorder) Asperger’s syndrome Autistic spectrum disorders Bipolar disorders (including cyclothymia) Chronic brain syndromes and cognitive impairment (dementias) Delirium Delusional disorders Dementias (Alzheimer’s, Creutzfeldt-Jakob, Lewy body and vascular) Depressive disorders (including dysthymia) Developmental disorders and learning difficulties Dissociative disorders Drug misuse disorders Eating disorders Habit and impulse disorders Insomnia Neuroleptic-related syndromes (akathisia, parkinsonism, tardive dyskinaesia, metabolic syndrome, cardiac dysrhythmias) Obsessive-compulsive disorder Panic disorder Personality disorders Phobic anxiety Post-traumatic stress disorder (PTSD) Psychosexual dysfunction (including gender identity) Schizophrenia Sleep disturbance Somatoform disorders (somatization, hypochondriacal disorder) OPHTHALMOLOGICAL TOPICS Emergencies Acute glaucoma Acute red eye Eye trauma (including foreign body) Retinal detachment Sudden loss of vision Procedures / operations Electroretinogram Eye drops / ointment Fundoscopy Slit lamp examination Visual evoked potentials Cases Cataract Glaucoma Gradual loss of vision Ptosis Sticky eye Unequal pupils Visual disturbance (including diplopia) OTOLARYNGOLOGICAL TOPICS Emergencies Acute severe throat infection Otitis media Procedures / operations Auditory evoked potentials Otoscopy Tympanometry Cases Dizziness and vertigo Dysphagia Epistaxis Facial pain (see also Neurology) Hearing loss Hoarseness and voice change Lump in the neck Nasal obstruction Otalgia Otorrhoea Vertigo THERAPEUTICS TOPICS Emergencies Acute poisoning Drug allergy Drug interactions Drug sensitivity Procedures / operations Prescription checking Prescription writing Use of the British National Formulary Cases Clinical pharmacology and therapeutics of core cases See separate Therapeutics course handbook 67 17 – Integrated Skills List To progress to Phase 4, students must be competent in the skills indicated from 1 – 3: Skills Practice Available denotes which skills can be practiced outside of normal teaching. The key is as follows IL - Independent Learning C – Curriculum teaching SU – Sign up skills PT - Peer teaching PE - Patient Educator teaching Further information on the availability of those sessions relevant to your year will be forwarded to you throughout the year. Please note – This list is not exhaustive. The skills may change during the medical course and it is your responsibility to keep up to date with these changes. Integrated Skills List 1. Fundamental skills 1.1 Numeracy 1.2 Presentation - Oral 1.3 Presentation - Poster 1.4 Professional Development 1.4.1 Courtesy to staff and patients 1.4.2 Punctuality 1.4.3 Accepting advice from tutors 1.4.4 Obtaining consent from patient 1.4.5 Confidentiality: Respect and protect patient information 1.4.6 Know about, understand and respect the roles and expertise of other healthcare professionals 1.5 Communicate with patients 1.6 Take and record a patients history, including their family history 1.6.1 Introduce yourself to patient 1.6.2 Put a patient at ease and build rapport 1.6.3 Ask about activities of daily living 1.6.4 Elicit a patient's concerns, ideas and expectations 1.6.5 Check a patient's understanding 1.6.6 Make a problem list after clerking a patient 1.6.7 Gather information from notes and other sources 1.6.8 Write a distillation of problems 1.6.9 Present a clinical history to tutor 1.7 Perform a full physical examination and a mental state examination 1.8 Participate as a member of the healthcare team 1.9 Document clinical details in patient notes 1.10 Handwashing and infection control 2. Communication skills 2.1 Adapt history taking to specialty inc. psychiatry, gynaecology, urology, dermatology, musculo-skeletal Year Introduced Year first signed-up or tested 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 1 3 2 2 1 1 1 2 2 3 3 3 3 2 2 2 2 2 2 3 3 3 3 3 3 3 1 3 5 5 2 3 3 Skills Practice available C, IL 68 17 – Integrated Skills List Integrated Skills List 2.2 Present clinical cases at grand rounds 2.3 Take a drug history e.g. aetiology of skin rashes 2.4 Discuss information with patient and relative e.g. child and parents 2.5 Give health advice on relevant lifestyle/risks e.g. smoking, sun 2.6 Take a history from third party e.g. parent/child; carer/elderly 2.7 Explain a common complaint to a child 2.8 Take a history from a patient with a serious illness as in A&E 2.9 Make a genogram from a patient with significant genetic history 2.10 Make a management plan for a patient 2.11 Communicate effectively with a person from a different culture 2.12 Present findings, conclusions and management plans to a professional 2.13 Record concise and accurate history in patients' notes 3. Assessment of special groups of patients 3.1 Take a history from a patient with chest pain 3.2 Take a history from a patient with breathlessness 3.3 Take a history from a patient with abdominal pain 3.4 Take a history from a patient with depression 3.5 Assess the mental state and cognition of an adult 3.6 Assess psychotic symptoms (delusions & hallucinations) 3.7 Assess alcohol intake (AUDIT) 3.8 Assess a suicidal patient 3.9 Make a preoperative anaesthetic assessment 3.10 Assess the mental state of an older patient 3.11 Observe the assessment of an unconscious patient 3.12 Observe the assessment of a patient requiring pain relief 3.13 Assess a newborn baby including screening 3.14 Assess an infant/child to include growth and development 3.15 Assess a pregnant woman 3.16 Assess a patient with limb trauma 4. Clinical examination skills 4.1 Take a temperature, radial pulse and respirations 4.2 Hand washing and infection control 4.3 Mental state of an adult 4.4 Superficial masses in neck and other parts of the body 4.5 Examine a superficial mass 4.6 Cardiovascular system including pulses 4.7 Respiratory system 4.8 Abdomen including the ano-rectum 4.9 Inguino-scrotal region 4.10 Neurology in the limbs (including gait) 4.11 Cranial nerves 4.12 Cerebellar function to include gait and co-ordination 4.13 Female breast Year Introduced 3 3 Year first signed-up or tested 3 3 3 4 3 3 4 4 4 3 4 4 4 3 4 5 3 5 3 3 5 5 3 3 3 3 3 3 3 3 3 3 3 3 4 4 4 4 3 3 3 3 3 3 3 3 4 4 4 4 4 4 4 4 1 1 3 3 3 3 3 3 3 3 3 3 3 1 1 3 3 3 3 3 3 3 3 3 3 4 Skills Practice available C C C IL C,IL, PT C,IL C,IL C,IL C,IL IL C,IL IL 69 17 – Integrated Skills List Integrated Skills List 4.14 Female pelvis 4.15 The skin 4.16 Locomotion to include mobility, limbs and back 4.17 Examine the musculo-skeletal system of the limbs in an adult (GAL) system, inc back, neck, hip, knee, ankle, foot, shoulder, elbow, hand 5. Examination using instruments 5.1 Measurement of blood pressure 5.2 The eye using an ophthalmoscope 5.3 The ear using an auriscope 5.4 Uterine cervix using Cusco speculum, take cervical smear and endocervical swab 5.5 Doppler index of foot pulses 6. Procedures to observe and explain: Imaging 6.1 CT scan 6.2 MRI scan 6.3 Lumbar puncture 6.4 Ultrasound including abdomen and pelvis 6.5 Angiography 6.6 IVU 6.7 Radionuclide scanning 7. Procedures to observe & explain: diagnostic procedures 7.1 Abdominal paracentesis 7.2 Spirometry and other respiratory function 7.3 Echocardiography/angiography 7.4 Barium enema 7.5 Gastroscopy and endoscopy of upper gastrointestinal tract 7.6 Colonoscopy 7.7 Sigmoidoscopy 7.8 Bronchoscopy 7.9 Cystoscopy 7.10 Pleural aspiration 7.11 Joint aspiration 7.12 Suprapubic catheterisation 7.13 Observe V/C Scan 7.14 Barium meal 7.15 Exercise ECG 7.16 Venography 7.17 Laparoscopy 7.18 Insertion of an arterial line 7.19 Fine needle aspiration of breast 7.20 Pre-natal testing e.g. amniocentesis 7.21 Observe calibration of a CVP monitor and interpretation of results 7.22 Arterial blood gas measurement 8. Practical skills 1: Basic skills 8.1 Take a venous blood sample 8.2 Perform sterile scrub technique and gown up Year Introduced 3 3 4 Year first signed-up or tested 4 4 4 Skills Practice available 4 4 1 3 3 1 3 3 C,IL, PT IL IL 4 3 4 5 IL IL 3 3 3 3 3 3 3 5 5 3 3 3 3 3 3 3 3 3 3 4 3 3 3 3 3 3 3 4 4 5 5 5 5 5 5 5 5 5 5 5 5 4 5 3 3 3 3 SU, IL IL 70 17 – Integrated Skills List Integrated Skills List 8.3 Perform pulse oximetry 8.4 Perform a rectal examination 9. Practical skills 2: Resuscitation skills 9.1 Basic life support for an adult (CPR) 9.2 Ventilation of an apnoeic patient using bag valve and mask 9.3 Insert a laryngeal mask airway 9.4 Advanced life support: demonstrate understanding of algorithms 9.5 Defibrillator: demonstrate use of 9.6 Resuscitation: Intermediate Life Skills certification 9.7 Endotracheal intubation: Observe 9.8 Basic Life support for a child 10. Practical skills 3: Investigation skills 10.1 Take a peak flow measurement 10.2 Perform a stick test for glucose-BM test 10.3 Perform a dip-stick test on a mid stream urine specimen 10.4 Examine and interpret x-rays inc chest x-ray, abdominal xray 10.5 Interpret clinical laboratory test results e.g. virology, microbiology 10.6 Take swabs for microbiology: a) wound b) throat c) skin 10.7 Take blood for culture 10.8 Perform joint aspiration 10.9 Perform femoral venepuncture 10.10 Observe lumbar puncture 10.11 Observe chest aspiration 10.12 Perform urine pregnancy test 10.13 Observe a arterial blood gas sample on a manikin 11. Treatment procedures 11.1 Observe a liver/renal biopsy 11.2 Observe CVP line insertion 11.3 Observe haemodialysis 11.4 Observe insertion of chest drain 11.5 Life support systems i.e. IPPV 12. Medication administration 12.1 Use of inhaler 12.2 Suppository/pessary insertion 12.3a Prepare and administer a subcutaneous injection 12.3b Prepare and administer a intramuscular injection 12.4 Prepare and administer an intravenous drug 12.5 Prescription checking 12.6 Write a prescription 12.7 Report an adverse drug reaction using the yellow card system 12.8 Contraceptives: use of barrier methods 12.9 Give drug using nebuliser 12.10 Give Oxygen at appropriate % concentration Year Introduced 3 3 Year first signed-up or tested 5 3 Skills Practice available IL IL 1 3 4 1 3 4 C,IL IL IL 4 4 5 3 4 4 4 5 IL 4 IL 1 2 1 1 2 1 C,IL,PT IL C,IL,PT 3 3 3 3 3 4 5 3 3 4 3 3 5 5 5 5 4 3 3 3 3 3 1 3 2 3 3 1 4 2 4 5 C,IL 2 3 2 3 C, IL, PT IL 3 4 3 3 5 4 5 5 C, IL,SU C, IL C,IL, PT C, IL 71 17 – Integrated Skills List Integrated Skills List 12.11 Set up and operate a syringe pump and medication 12.12 Instil eye drops/eye ointment 12.13 Use of nasal spray 12.4 Explain to a patient a skin preparation 13. General patient management 13.1 Height and weight measurement charting with BMI calculation 13.2 Record BMI 13.3 Sterile technique 13.4 Record and interpret 12 lead ECG 13.5 Interpret results of investigations inc a) haematological b) clinical chemistry c) neurological d) psychiatric 13.6 Female catheterisation 13.7 Insert a naso-gastric tube 13.8 Male catheterisation 13.9 Remove wound drains 13.10 Perform wound care 13.11 Remove sutures and staples 13.12 Immobilise the cervical spine 14. Specialist skills 14.1 Suture a wound 14.2 Assess a patient's ability to function at home 14.3 Participate in a multi-disciplinary needs assessment 14.4 Deliver a baby 14.5 Observe the assessment of a patient with delirium 15. Patient management on the wards or in community 15.1 Plan investigations and treatments 15.2 Complete a ward admission, make continuation notes 15.3 Complete investigation request forms: lab tests, X-rays 15.4 Complete a blood transfusion request form 15.5 Complete a GP prescription 15.6 Complete an inpatient prescription 15.7 Negotiate with a patient to agree an acceptable management plan 15.8 Explain procedure or operation to patient or relative 15.9 Write a discharge notification 15.10 Write a ward referral 15.11 Write an out-patient referral 15.12 Set up a blood transfusion 15.13 Certify death 15.14 Complete a death certificate 15.15 Observe the reporting of a death to a coroner Year Introduced 5 3 3 4 Year first signed-up or tested 5 Skills Practice available C,IL,SU 4 1 1 1 3 1 1 1 3 3 3 3 3 3 4 4 4 3 4 5 3 5 5 5 3 3 3 4 3 4 4 4 4 3 5 3 5 5 3 5 5 5 5 5 3 5 3 5 5 5 5 5 5 5 5 5 5 5 5 5 5 IL C,IL,SU IL,SU C,IL,SU IL,SU C,IL,SU IL IL,SU C C 72 17 – Integrated Skills List Core Patient Cases Acronyms COPD [Chronic Obstructive Airways Disease] CABG [Coronary Artery Bypass Graft (CABG)] ECG [Electrocardiogram ECG)] GTN spray ([Glyceryl Trinitate (GTN)] CVP [Central Venous Pressure] MI [Myocardial Infarct (MI)] GI [Gastrointestinal haemorrhage (GI)] CT scan [Computerised Tomography (CT)] EEG [ Electroencephalography (EEG)] EMG [Electromyography (EMG)] MRI (add “scan” Magnetic Resonance Imaging (MRI)] PET add scan [Positron Emission Tomography (PET)] ECT [Electroconsulsive therapy (ECT]) Integrated Skills List Acronyms 3.7 AUDIT [Alcohol Use Disorder Identification Test (AUDIT)] 4.17 (GAL) [Gait and Locomotion] 6.1 CT scan [Computerised Tomography (CT)] 6.2 MRI scan [Magnetic Resonance Imaging (MRI)] 6.6 IVU [Intravenous Urography (IVU)] 7.13 Observe VC scan [Vital Capacity (VC)] 7.15 Exercise ECG [Electrocardiograph (ECG)] 7.21 CVP [Central Venous Pressure (CVP)] 9.1 CPR [Cardiopulmonary resuscitation (CPR)] 10.2 Perform a stick test for glucose BM test [Boehringer Mannheim (glucose BM test)] 11.2 Observe CVP line insertion (As 7.13) 11.5 Life support system i.e. IPPV [Intermittent positive pressure ventilation (IPPV)] 13.1 and 13.2 BMI [Body Mass Index (BMI)] 13.12 ECG (As 7.15) 73 18 - Quick Contacts for Key Organizers and Campus Administrators (Key staff addresses are in the Phase 3 Handbook) HEAD OF PHASE 3 Dr Teifion Davies [email protected] 020 7848 0100 CHAIR OF PART 3 BOARD OF EXAMINERS Dr Chris Kosky [email protected] Examinations & Assessments Administrator Philip Wright [email protected] 020 7848 6723 OSCE Administrator James Hollands [email protected] 020 7848 6101 ROTATION B HEAD Prof Leone Ridsdale [email protected] 020 7848 5182 HEAD OF SSCs for Phase 3 Dr Eithne MacMahon [email protected] 20 7188 1285 (PA) Medical Student Administrator - St Thomas’ & Guys Maria Fernandes [email protected] 020 7188 5183 Medical Student Administrator – King’s Sheinaz Mahomedally [email protected] 020 7848 5224 Undergraduate Administrator – Canterbury Abigail Ballard [email protected] 01227 866394 Undergraduate Administrator – Ashford Brenda Harden [email protected] 01233 616717 Undergraduate Administrator – Margate Lisa Fletcher [email protected] 01843 225544 Ext: 62042 DEPUTY HEAD OF PHASE 3 Dr Amy Iversen [email protected] 020 7848 5509 Phase 3 Undergraduate Officer Lucy Watts [email protected] 020 7848 6102 Senior Assessments Officer (MB BS) Jo Wilson [email protected] 020 7848 6706 ROTATION A HEAD Mr Simon Atkinson [email protected] 020 7188 4195 ROTATION C HEAD TBC SSC queries (Phase 3) Ms Gillian McCormack [email protected] 020 7848 6725 Medical Student Administrator-St Thomas’ & Guys Rachel Bates [email protected] 020 7188 3735 MBBS Administrator – King’s Mary McCarthy [email protected] 020 7848 5618 Undergraduate Administrator – Kent & Medway Debbie Monticolombi [email protected] 01227 812189 Medical Student Manager - Chichester Nissrine Tollaz [email protected] 01243 788122 ext 2795 Medical Student Administrator – Medway Daniella James [email protected] 01634 8300000 ext 3238 Medical Student Administrator – Lewisham Samantha Newman [email protected] 020 8333 3000 ext 8734 Psychiatry and Neurology Teaching Administrator Wiktor Madejczyk [email protected] 020 7848 5182 General Practice Teaching Lead Dr Kerry Boardman [email protected] 020 7848 8696 General Practice Administrator Simon Power [email protected] 020 7848 4311 74 18 - Quick Contacts for Key Organizers and Campus Administrators Psychiatry Coordinator Dr Paola Dazzan [email protected] 020 7848 0590 Ophthalmology Coordinator – St Thomas’ Mr Danny Morrison [email protected] 020 7188 4334 Senior Clinical Adviser – Joseph Lister House Dr John Philpott-Howard [email protected] 020 3299 3213 Senior Clinical Adviser – Astley Cooper House Dr Anne Stephenson [email protected] 020 7848 8704 Education Advisor Michelle Robinson [email protected] 020 7848 6855 ENT Coordinator Miss Elfy Chevretton [email protected] (Secretary) 020 7188 2217 (Secretary) Ophthalmology Coordinator – King’s & Lewisham Mr Tim Jackson [email protected] 020 3299 3385 Senior Clinical Adviser – Thomas Addison House Dr Sonji Clarke [email protected] 020 7188 6865 Senior Clinical Adviser - Cicely Saunders House Prof Mary Seller [email protected] 0207 188 6098 75 What to do if you have a percutaneous or mucosal exposure to potentially HIVinfected blood or other high-risk body fluid: In all cases – whether the patient is known to be high risk for any infection or not • Encourage the wound to bleed, ideally by holding it under running water • Wash the wound using running water and plenty of soap • Don’t scrub the wound while you are washing it • Don’t suck the wound • Dry the wound and cover it with a waterproof plaster or dressing • Mucosal splash (eye, mouth): rinse with a lot of sterile water or saline for 10 minutes • Note name number and location of ‘donor’ patient, if known. Notify a senior person in the ward or clinic • Fill out an incident form (later) • Attend Occupational Health IMMEDIATELY AND ALWAYS WITHIN AN HOUR IF AT ALL POSSIBLE • OUT OF HOURS attend ACCIDENT & EMERGENCY; report a ‘needlestick injury’ and you will be seen quickly. HIV PROPHYLAXIS, IF NEEDED, MUST BE STARTED WITHIN ONE HOUR OF THE EXPOSURE IF AT ALL POSSIBLE