* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Survey
Document related concepts
Transcript
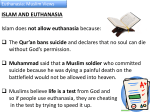
Death and Dying The Dying Process: Modern medicine has enabled people to live longer and survive illnesses that once caused death. This has created some ethical and moral dilemmas for the healthcare profession. Patients can now be kept alive by medical technology, but death is inevitable for everyone. Expired means “died.” The Legal Definition of Death: The actual determination of death is critical because of the advances in medicine such as organ transplantation and life support, so there is a Criteria or standards for death, which assist in the determination that death has occurred: Loss of heartbeat, significant drop in body temperature, loss of body color and rigor mortis (stiffness) Symptoms may not appear until several hours after death or not at all if life-support equipment is used. The best example of this is, The Karen Ann Quinlan Case Who fell into an unconscious vegetative state from prescription drugs and an alcohol overdose A tracheotomy to help with breathing and a nasogastric tube for nourishment kept her alive Parents appealed to have respirator discontinued and after many reversals in court, The respirator was discontinued, but feeding tube continued Karen lived in coma for ten years without respirator. Two definitions of death: Cardiac and Brain-oriented death Cardiac Death Death in which heart has stopped functioning Lack of pulse or breathing Irreversible loss of all cardiac function Serious problem for organ transplants Many people believe that a cardiac oriented definition of death is inadequate. Death is considered legal. Brain-Oriented Death Death occurs when there is irreversible cessation of all brain function Most states accept this definition of death Heart and lung functions can be maintained by mechanical means after brain function has stopped, so time of death depends on cessation of brain activity. Harvard Medical: Criteria for Definition of Irreversible Coma, i.e. Brain Death Unreceptive and unresponsive with total unawareness of externally applied and painful stimuli No spontaneous movements or breathing, absence of response to pain, touch, sound, or light No reflexes, with fixed dilated pupils, lack of eye movement, and lack of deep tendon reflexes Because of controversy over the criteria for determining brain death, in 1990 Congress enacted, The Uniform Determination of Death Act: which states the following: An Individual is dead if he or she has sustained either: Irreversible cessation of circulatory and respiratory functions, or Irreversible cessation of all functions of the entire brain, including the brain stem Types of Patient Treatment in Final Stages Withdrawing vs. Withholding Treatment Withdrawing means to discontinue treatment after it has been started Withholding means never starting treatment Many believe both are ethically wrong. Patients have the legal right to refuse treatment and food Active Euthanasia Versus Passive Euthanasia Active euthanasia: intentional killing of the terminally ill is illegal in all jurisdictions in the United States except Oregon Patient-assisted suicide (PAS): physician provides patient with medical know-how or means to enable patient to end own life. Oregon requires Passive euthanasia: allowing patient to die naturally, which is legal, discontinuing chemotherapy which is ineffective and burdensome, or painful intravenous tubes. See Nancy Cruzan Arguments for Euthanasia Patient self-determination Harvesting viable organs Relief for family if patient has irreversible condition. Provides means to end patients suffering. Some arguments in opposition No certainty regarding death Research and technology may find a cure for a terminal disease. Can relieve financial burden from m families and patient Euthanasia can be used indiscriminately You Be The Judge! Remember, While you are reading the scenario, try not to make comments as I want everyone to be able to fully read the case, OK? Let’s get started During State performed executions it is common practice for physicians to be present in order to certify that the prisoner is dead. He is also there to certify the date day and time of death. In states where lethal injection is used as a form of execution,, the physician administers the lethal drugs. A state medical association has objected to The participation of physicians in any and all executions. They feel that physicians take an oath to “do no harm.” Physician should no inject lethal doses of drugs in order to promote death….. They (physicians should not act as accessories in taking of life during execution. The association contends that the physician is nothing more than an accessory to murder. What are your thoughts on execution? Should physicians take part in executions… Why? Why Not? Answer with comments. Is the physicians role in executions ethical? Why/Why Not? Direct Vs. Indirect Killing Direct killing: death is result of another person’s intended action or inaction Indirect killing: death is result of unintentional result of another’s action Double-effect doctrine: an action may have two consequences, one desired (and intended) and one undesired (and unintended) Ordinary Vs. Extraordinary Treatment Ordinary: treatment or procedure that is morally required, such as fluids and comfort measures, may be called appropriate Extraordinary measures: procedures and treatment that are morally expendable, such as chemotherapy, tube feedings, CPR, and mechanical breathing or respirators may be called inappropriate Additional examples of treatment that might be ordered for the terminally ill: CPR: Cardiopulmonary Resuscitation Respirator, Tube Feeding Kidney Dialysis Chemotherapy What would you do? Right to Die or Right to Refuse Treatment Patients have the right to refuse treatment If refusal places their lives in danger, physicians sometimes take legal action through the courts. Five Stages of Dying According to Dr. Elizabeth Kubler-Ross, author of Death and Dying, the dying process is divided into five stages, which the patient, family members and caregivers all experience. The stages may overlap and may not be experienced by everyone involved in stated order, but all are present in a dying patient. These stages are important to all concerned, they are • Denial: Refusal to believe that dying is taking place. • Anger: Patient may be angry with everyone and express that anger often to those around him/her. • Bargaining: Gaining time by making promises to God in return for a cure. • Depression: There is a deep sadness over loss of independence, health and eventually life. • Acceptance : This stage carries a sense of peace and calm. All stages of the dying process have impact on Quality-of-Life Issues. The medical profession uses: general health, physical functioning, role limitations, bodily pain, social function, vitality and mental health to assist and assess the patient quality of life and comfort. Dying patients often spend most of their last days in moderate or severe pain. Physicians are often reluctant to overprescribe pain medications for fear patient may become addicted to a drug or drugs. Many physicians now believe a patient’s pain and suffering should be controlled with use of Medication and other measures Types of care for End Stage: Hospice Care: Originated in France. Committed to keeping patients as pain-free as possible. They are focused on providing comfort measures, emotional support, and as pain-free as possible environment for the patient at end of life. The staff is specially trained to provide the proper and necessary care for a patient in the final stages. Palliative Care: Total care of patients whose disease is no longer responsive to curative therapy. Palliative care consists of comfort measures meant to provide a relief of pain and suffering so patient can die with dignity. Emphasizes symptom control, which is opposite of curative care In Palliative and Hospice care, emphasis is on the patient and their end of life, death with dignity. Suicide is considered morally wrong and illegal in most states. No state punishes people who attempt suicide, but they may be placed in psychiatric care if present danger to themselves Many religions condemn suicide and euthanasia Many insurance companies will deny payment on a insurance policy if the cause of death is ruled a suicide. Advance Directives Documents such as living will, durable power of attorney for health care, Uniform Anatomical Gift Act, and do not resuscitate (DNR) orders, must be in place while the patient is competent to make decisions. Appointing one individual to be a Durable Power of Attorney is vital to having the patient desires and needs followed. Providing a copy to the patient’s medical team is also vital. Advance Directives Limit type and amount of medical care and treatment patients will /wish to receive if they become incompetent and have poor prognosis. They provide choices in life and death for the patient. Be sure patient and physician are in agreement over advanced directives. Death Certificates Must be signed with time, place, date and cause of death by an administering physician. They Must also include the following: Name and address of decedent, Age, Place and date of birth, Names parents (including mother’s maiden name),Birthplace of parents, Race, Decedent’s occupation. Two types: Certified and Non certified. Always get copies of both. Death certificates, must be provided to certain agencies, i.e. Social Security, Pension Funds, Insurance companies, and some require certified copies other agencies do not. Medical Examiner Cases: Legal investigation by medical examiner or coroner in case of suspicious death. Investigation is required if death is: Violent in nature (homicide, suicide, accident) Caused by criminal abortion Related to contagious or virulent disease A person confined to jail or correctional institution Result of unexplained or unexpected cause Caused by electrical, radiation, or chemical injury A person who had no physician in attendance within 36 hours of death A person whose body is not claimed by friend or relative A child under age of two if death is from unknown cause A person of unknown identity Glenn Ross is 55. He is diagnosed with inoperable pancreatic cancer. Prognosis is poor. Drs. Say he will live about six months. Chemotherapy provided no relief or benefit. After three months with his condition worsening, he stops treatment. Thereafter he was admitted to a nursing facility for terminal care. Glenn’s son, who lived in another state visited his father at the nursing home and demanded that his father be hospitalized and placed on chemotherapy immediately. When the physician explained that chemotherapy would not provide any recovery, his son threatened to sue. Does the son have a legitimate reason to sue? What are the ethical issues? What a possible solutions to this case? You will need to think about some legal, moral and ethical issues in the health care system to discuss in your paper . Research some of the issues we discussed throughout the term and check other sources…. Please be sure to answer questions in full and complete statements. Watch your spelling grammar and punctuation. Be sure to reference. Remember there are many sites available on lone for guiding you through proper citations. If you provide the writing center 48 hours, they can review your work. Do not wait until the last minute to complete your work. What can go wrong will go wrong, if you know what I mean. I want you to be successful. You know where to find me if you need questions answered.