* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Document
Survey
Document related concepts
Transcript
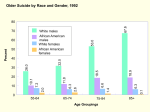
Death and Dying Chapter 13 Medical Law and Bioethics, 2nd Edition Bonnie F. Fremgen 2006 Pearson Education, Inc Pearson Prentice Hall Upper Saddle NJ, 07458 The Dying Process Death is inevitable for everyone Modern medicine has enabled people to live longer and survive disease Patients can now be kept alive by medical technology Health care professionals have a duty to preserve life Legal Definition of Death Determination of death is important for many reasons Actual determination of death is critical due to organ transplantation and life-support systems Karen Ann Quinlan Case April 15,1975: 21-year-old unconscious from a prescription drug and alcohol overdose Tracheotomy to help with breathing and nasogastric tube for nourishment Father appealed to have respirator discontinued Respirator discontinued, but feeding tube continued Lived in coma for ten years without respirator, then died Criteria for Death Assist in determination that death has occurred Loss of heartbeat, significant drop in body temperature, loss of body color, rigor mortis (stiffness) Symptoms may not appear until several hours after death or not at all if life-support equipment used Cardiac Death Death in which heart has stopped functioning Lack of pulse or breathing Considered a legal death Irreversible loss of all cardiac function Serious problem for organ transplants Brain-Oriented Death Death occurs when there is irreversible cessation of all brain function Most states accept this definition of death Heart and lung functions can be maintained by mechanical means after brain function has stopped Harvard Criteria for Definition of Irreversible Coma Unreceptive and unresponsive with total unawareness of externally applied and painful stimuli No spontaneous movements or breathing, absence of response to pain, touch, sound, or light No reflexes, with fixed dilated pupils, lack of eye movement, and lack of deep tendon reflexes Uniform Determination of Death Act 1990 approved Individual is dead if he or she has sustained either – – Irreversible cessation of circulatory and respiratory functions, or Irreversible cessation of all functions of the entire brain, including the brain stem Withdrawing Versus Withholding Treatment Withdrawing means to discontinue treatment after it has been started Withholding means never starting treatment Many people believe both are ethically wrong Patients have the legal right to refuse treatment and food Active Euthanasia Versus Passive Euthanasia Active euthanasia: intentional killing of the terminally ill is illegal in all jurisdictions in the United States except Oregon Patient-assisted suicide (PAS): physician provides patient with medical know-how or means to enable patient to end own life Passive euthanasia: allowing patient to die naturally is legal The Nancy Cruzan Case January 11, 1983: 25-year-old injured in auto accident was left in vegetative state Feeding tube implanted Family requested feeding tube be removed U.S. Supreme Court ruled against Cruzans New evidence of Nancy Cruzan not wishing to be maintained as in the Karen Quinlan case Feeding tube removed and Nancy Cruzan pronounced dead on December 26, 1990 Direct Versus Indirect Killing Direct killing: death is result of another person’s intended action or inaction Indirect killing: death is result of unintentional result of another’s action Double-effect doctrine: an action may have two consequences, one desired (and intended) and one undesired (and unintended) Ordinary Versus Extraordinary Means Ordinary: treatment or procedure that is morally required, such as fluids and comfort measures, may be called appropriate Extraordinary measures: procedures and treatment that are morally expendable, such as chemotherapy, tube feedings, CPR, and mechanical breathing or respirators may be called inappropriate Right to Die Legislation or Right to Refuse Treatment Patients have the right to refuse treatment If refusal places their lives in danger, legal action sometimes results Stages of Dying According to Dr. Elizabeth Kubler-Ross, dying process is divided into five stages patient, family members, and caregivers all experience Stages may overlap and may not be experienced by everyone in stated order, but all are present in dying patient – – – – – Denial Anger Bargaining Depression Acceptance Quality-of-Life Issues Measures to assess quality of life include – – – – – – – General health Physical functioning Role limitations Bodily pain Social function Vitality Mental health Use of Medications Dying patients often spend most of their last days in moderate or severe pain Physicians are often reluctant to overprescribe pain medications for fear patient may become addicted to drug Many physicians now believe patient’s pain and suffering should be controlled with use of adequate medications Hospice Care Originated in France Committed to keeping patients as pain-free as possible Focused on providing comfort measures, emotional support, and as pain-free as possible final environment for the patient Staff specially trained in caring for dying patient An elderly hospice patient Figure 13-1 Palliative Care Total care of patients whose disease is no longer responsive to curative therapy Consists of comfort measures Meant to provide a relief of pain and suffering so patient can die with dignity Emphasizes symptom control Opposite of curative care Viatical Settlements Allow people with terminal illness to obtain money from life insurance policies by selling them In exchange for 20 to 50 percent discount on face value of patient’s insurance policy, patient can have immediate access to money Patient names settlement company as recipient of death benefit Many use money to provide for medical and nursing care during final illness Advance Directives Documents such as living will, durable power of attorney for health care, Uniform Anatomical Gift Act, and do not resuscitate (DNR) orders Popularly known as living wills Limit type and amount of medical care and treatment patients will receive if they become incompetent and have poor prognosis Choices in Life and Death Suicide is considered morally wrong and illegal in most states No state punishes people who attempt suicide, but they may be placed in psychiatric care if present danger to themselves Many religions condemn suicide and euthanasia The Case of Conjoined Twins 50 hour operation to separate 29-year-old twins joined at head Death resulted during procedure in July 2003 Twins knew of risks but knowingly accepted risks Many ethical debates about the separation Mechanical Heart Recipient Implanted in 59-year-old man in July 2001 Did well until he suffered severe strokes from blood clots Final days of life spent partly paralyzed and breathing through a ventilator Lived for five months with mechanical heart Death Certificate Must include the following: – – – – – – – Name and address of decedent Age Place and date of birth Names of parents (including mother’s maiden name) Birthplace of parents Race Decedent’s occupation Medical Examiner Cases Legal investigation by medical examiner or coroner in case of suspicious death. Investigation is required if death is: – – – – – – – – – – Violent in nature (homicide, suicide, accident) Caused by criminal abortion Related to contagious or virulent disease Of a person confined to jail or correctional institution Result of unexplained or unexpected cause Caused by electrical, radiation, or chemical injury Of a person who had no physician in attendance within 36 hours of death Of a person whose body is not claimed by friend or relative Of a child under age of two if death is from unknown cause Of a person of unknown identity