* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download Interesting Case
Survey
Document related concepts
Transcript
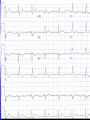
Interesting Case 82 year old man • Brought in to RAZ by EMS Presenting Complaint (nursing notes) “Ground level fall at 13:15 today. Unresponsive for 3 minutes after fall. No seizure, but incontinent of urine. Witnessed by wife.” What do you want to know? • BP 121/71 • HR 76 • RR 18 • O2 95% on 2 liters • T 36.7 Patient awake Confused Not oriented to place or time Doesn’t remember what happened Fortunately… • His wife is there Unfortunately… • She’s almost as confused as he is • She can tell you what happened, though History • Shopping – fell backwards while walking. • No prodrome • Hit back of head on floor Past Medical History • Two recent falls in the past month – wasn’t seen in hospital for these • Dementia • Rarely sees a doctor • No medications On exam • T 36.7 HR 76 RR 18 BP 121/71 O2 95% on 2 liters • CN exam normal • Hematoma right occiput • HR regular, no murmur • Wife thinks slightly more confused than usual •What next? •Any concerns? •Differential Dx? • Time to move • Needs a monitored bed • Investigations? Investigations • CBC, Lytes, Creatinine, Glucose, Mg, Phosphate, Calcium, Troponin • ECG • CT head and C-spine ECG • RBBB • Left Anterior Fascicular Block CT • CT C-spine normal • Cleared C-spine precautions CT head CT Head Report • Intraparenchymal hemorrhage involving bilateral posterior parietal lobes at occipital junction • Small SAH right frontal lobe • No midline shift Meanwhile… • Patient ticking along happily until… I hear some commotion… • Patient is slumped over and the monitor shows this rhythm • Asystole! •! •! •! • Spontaneous Resolution • Get the crash cart • Pads put on Quickly now… • Let’s have a talk about Level of Care • Full bore ahead Who ya gonna call? • A. Ghostbusters • B. Your Mom • C. The laundromat (underwear feels sort of damp) • Cardiology Next step • Transvenous Pacer • Patient agitated – required some sedation, but procedure otherwise successful Syncope • “Sudden transient loss of consciousness associated with inability to maintain postural tone.” Syncope • 1-3% of all ED visits • 1-6% Admissions Causes • Vasovagal, Carotid sinus syndrome • Neurologic – SAH, Subclavian steal • Medications • Orthostatic hypotension • Pulmonary Embolus • Cardiac Cardiac Syncope • 1. Structural – Aortic Stenosis, Cardiomyopathy, MI • 2. Dysrhythmias – Brady and Tachy Bradysrhythmias • 2nd or 3rd degree heart block • Sinus node disease • Pacemaker malfunction Tachydysrhythmias Ventricular tachycardia SVT A Fib A Flutter San Francisco Syncope Rules • CHESS • C – History of CHF • H – Hematocrit < 30% • E – Abnormal ECG • S – Shortness of Breath • S – Systolic Blood Pressure < 90 “Abnormal ECG” • Dysrhythmias • WPW • Brugada • Prolonged QTc • Any new abnormality Boston Syncope Rules • Broad set of rules – 25 criteria • Misses our patient Short-Term Prognosis of Syncope (STePS) • 4 Independent predictors – • 1. Abnormal ECG • 2. Concomitant trauma • 3. Absence of prodrome • 4. Male gender Back to our patient • Admitted to Cardiology • Transferred to Foothills for permanent pacer • Slow to recover from anaesthesia and transferred to ICU • Tachyarrhythmias – started on a metoprolol • Stabilized somewhat – transferred to CCU at PLC • Diagnosis of Sick Sinus Syndrome • No interventions regarding the intraparenchymal bleeds One more thing • Anchoring • Start with an anchor – something you know – and adjust in the direction you think is appropriate • Often not enough adjusting