* Your assessment is very important for improving the work of artificial intelligence, which forms the content of this project
Download CENTRAL LINES
Management of acute coronary syndrome wikipedia , lookup
Electrocardiography wikipedia , lookup
History of invasive and interventional cardiology wikipedia , lookup
Coronary artery disease wikipedia , lookup
Antihypertensive drug wikipedia , lookup
Cardiac surgery wikipedia , lookup
Arrhythmogenic right ventricular dysplasia wikipedia , lookup
Atrial septal defect wikipedia , lookup
Dextro-Transposition of the great arteries wikipedia , lookup
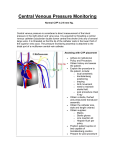
Central Venous Access Mazen Kherallah, MD, FCCP Indications Need for IV access and failure of peripheral access Peripheral access too painful or tenuous Long term IV access anticipated Medications indicated that are toxic to peripheral veins Hemodynamic monitoring Volume resuscitation with large bore central lines Special procedure: Swan Ganz, dialysis, plasmapheresis Site Selection Site Pro’s Subclavian Large vessel Can tolerate high flow Dressing easy to maintain Less restrictive for patient Lowest sepsis rate 5/25/2017 Con’s Close to lung apex, risk of pneumothorax Close to subclavian artery Hard to control bleeding Site Selection Pro’s Con’s Large vessel Easily located Easy access Short, straight path to superior vena cava Decreased risk of pneumothorax Uncomfortable for patient Difficult to maintain dressing Close to carotid artery Easily contaminated Difficult maintenance with trach or neck injury Site Internal Jugular 5/25/2017 Site Selection Site Femoral 5/25/2017 Pro’s Easy access Large vessel Good access during resuscitation Con’s Decreased mobility Increased risk of thrombosis, phlebitis & infection Easily contaminated Close to femoral artery Dressing difficult to maintain Choice of Site Subclavian IJ Femoral Success Rate 90-95% 90-99% 90-95% Arterial puncture 0.5-1% 10% 5-10% Pneumothorax 1-5% 0-0.2% 0 Infectious rate Lowest Intermediate Highest Access during cardiac arrest 2nd 3th 1st Side of body preference Left: angle of subclavian vein Right: avoid thoracic duct None Coagulopathy present 3th 2nd 1st Hypovolemia present 1st: vein supported by fibrous sheath 3th: vein collapses 2nd Pacemaker 2nd 1st 3th Anatomy of Great Vessels Anatomy of Great Vessels Anatomy of Great Vessels Seldinger Technique The Procedure Patient position: Patient is moved to the side of the bed so physician would not lean over The bed is high enough so physician would not have to stoop over Patient should be flat without a pillow, Trendelenburg position if patient is hypovolemic The head is turned away from the side of the procedure Wrist restraints if necessary The Procedure Skin preparation: Prepare before putting sterile gloves Start at the center and work outward the edges Allow time for the sterilizing agent to dry Disposable drape under the patient Betadine or Chlorhexidine are acceptable solution and have activity against gram positive organisms The Procedure Drape: Large enough Handed sterilely by the assistant Hole in the area of placement Prepare the tray: Handed sterilely by the assistant Prepare the equipment before starting Anesthesia Use local anesthesia with lidocaine YOUR ROLE AFTER THE INSERTION Dispose all sharps Place an occlusive sterile dressing Flush lumens to maintain patency Obtain a chest x-ray (ask for order if physician doesn’t mention it) Monitor site for bleeding Assess breath sounds Assess circulation Assess for hematoma Document insertion, site, dressing and flushing USING THE CENTRAL LINE Flush q shift, before and after use with NS. Some places also require heparin flush Close clamps when not is use Check P&P of facility, but usually fluids are changed every 24 hours, tubing changed every 48-72 hours Dressing is usually changed every 3 days Line can be used for blood drawing - withdraw and waste 10 cc, then withdraw blood for samples If port becomes clotted, do not use - sometimes ports can be opened up with urokinase (requires a doctor’s order) Complications Immediate Hemothorax Pneumothorax Arterial puncture Vessel erosion Nerve Injury Dysrhythmias Catheter malplacement Embolus Cardiac tamponade Complications Delayed Dysrhythmias Catheter malplacement Vessel erosion Embolus Cardiac tamponade Catheter related infection Thrombosis Vascular Erosion/Cardiac Tamponade Large vessel perforation is uncommon Vessel erosion more common with stiff catheters, like dialysis catheters Cardiac tomponade occur mainly if the tip is located in the RA Complication is fatal in 2/3 of cases Air Embolism Air is sucked in through the catheter due to negative intrathoracic pressure during inspiration Air can be pushed with flushing the catheter if it was not pulled back before flushing Complication is uncommon but can be fatal Manifests with hypoxemia, cardiovascular collapse, mental status changes and livedo reticularis Place patient to left lateral position if suspected Bleeding More common in patients with coagulopathy Easily controlled with femoral or IJ sites Place local pressure and correct coagulopathy Arterial Puncture and Cannulation If the artery is puncture local pressure is applied for 3-5 minutes, observe for hematoma formation If the artery is cannulated, pulsatile reflux of blood can be noticed, blood gas analysis reveals arterial. The catheter should not be used, and remove it after coagulopathy is corrected if present Thrombosis Sleeve fibrin surrounding the catheter (occurs on the majority of catheters) Mural thrombus on the wall of the vein (1030% of catheters) Occlusive thrombus (1-10%) Pneumothorax Most likely, pneumothorax is noticed after CXR is seen, unless patient developed tension pneumothorax with hypoxemia, cardiopulmonary collapse and absent breath sound Small pneumothorax may be watched closely without chest tube placement in the spontaneously breathing patients Large pneumothorax requires chest tube placement Even small pneumothorax in patients on positive pressure ventilation requires chest tube placement Catheter-Related Sepsis Late complications Femoral > IJ > subclavian Triple lumen > single lumen Large bore > smaller catheter Sterility of procedure Number of hub manibulations Basic Pressure Measurements from Swan Ganz Catheter Measurement Normal range Central venous pressure <10 mm Hg Right atrial pressure <10 mmHg Right ventricular pressure, systolic 15-30 mm Hg Right ventricular pressure, diastolic 0-8 mm Hg Pulmonary artery pressure, systolic 15-30 mm Hg Pulmonary artery pressure, diastolic 5-16 mm Hg Pulmonary artery pressure, mean 10-22 Pulmonary artery wedge pressure, mean 8-12 Hemodynamic Monitoring Position of Transducer Components of the Atrial Waves Differences in CVP and PCWP EKG correlation Wave EKG correlate Description A In the P-R interval RA contraction C End of QRS V Near end of T wave Closure of the tricuspid valve Filling of the RA X descent Y descent Downward slope of a wave Downward slope of v wave CVP Correlation with EKG Normal CVP Tracing Reading the mean of an A wave 22+10/2=16 Spontaneous Breathing Reading CVP Spontaneous Breathing Insp./Exp. Ratio in Rapid Breathing Spontaneous Breathing Insp./Exp. Ratio in Rapid Breathing Hemodynamic Monitoring Central Venous Pressure: normal 4-10 Increased CVP: Right heart failure Right myocardial infarction Cardiac tomponade Tricuspid insufficiency Left to right shunt Pulmonary emboli COPD and cor pulmonale ARDS Excess fluid Tricuspid stenosis Decreased CVP hypovolumia Decreased venous return Excessive veno or vasodilation Shock Central Venous Pressure Tracings Normal EKG tracing and right atrial pressure waveform Atrial fibrillation Atrioventricular dissociation Central Venous Pressure Tracings Normal EKG and right atrial waveforms Tricuspid stenosis Mild to moderate tricuspid insufficiency Severe tricuspid insufficiency Constrictive pericarditis Large A wave Secondary to Loss of Atrioventricular Synchrony Simultaneous Atrial and Ventricular Contraction Loss of A Wave Atrial Fibrillation